Efficacy and Safety of Curcuma longa L: Relevant Results for Cancer Treatment
Abstract
Cancer represents an important public health challenge, and its occurrence has been increasingly observed at human and veterinary medicine. However, despite of the significant results published by the scientific community, the use of medicinal plants for cancer treatment is not properly widespread. Thus, considering that Curcuma longa Linn. has demonstrated an important antitumor activity, the objective of this study was to present the main results of in vitro and in vivo studies. The anticancer activity of turmeric was found by the capability to induce apoptosis, reduce metastatic potential and inhibiting different tumor types of proliferation. In addition, other activities such as immunomodulatory, anti-inflammatory, and the inhibitory effect on modulating proteins of drug resistance are relevant for tumor therapy. Therefore, the results demonstrated by in vitro and in vivo studies showed that C. longa presents important evidence of prophylactic and curative effect for cancer treatment.
Keywords
Antitumor, Medicinal plants, Neoplasms Curcuma longa, Turmeric
Introduction
Cancer represents an important public health challenge, and its occurrence has been increasingly observed in both human and veterinary medicine [1,2]. Several modalities of natural medicine have been used as complementary therapy in oncological treatment, emphasizing the use of medicinal plants [3]. The diffusion of these natural therapies among cancer patients is mainly due to the dissatisfaction with the results of conventional medicine and the ability to reduce the usual side effects of chemotherapy and radiotherapy [3]. In addition, the affinity for the use of natural products and the search for lower cost treatments are considered [4].
The use of medicinal plants accentuated from the 90's, mainly due to aspects as safety, effectiveness, and low cost in comparison to chemical drugs. However, despite of the significant results published by the scientific community, an important obstacle to adequate use of medicinal plants is the fact that this knowledge is not properly widespread. In cases that cancer patients are not attended in their request regarding the use of medicinal plants, it is often observed the independent use of these plants by themselves. So, the most patient adept at medicinal plants obtains the information from popular knowledge, using them in oncological treatments in an empirical way [5].
Empirical use may be detrimental to the health and efficacy of cancer treatment and may lead to hepatotoxicity, nephrotoxicity, and cardiovascular toxicity [6]. Therefore, the development and dissemination of research related to the use of medicinal plants in oncology is justified not only by the growing interest but also especially by the need to sensitize health professionals to the possibility of effective complementary therapy. Thus, considering that C. longa has been shown to present an important antitumor potential, the objective of this study was to discuss the main relevant results of in vitro and in vivo studies about the antitumor activity of Curcuma longa Linn.
Review Methodology
The studies presented in this review were identified through a literature review conducted on Google Scholar, Scielo, Medline and Science Direct. The key terms used were: Antineoplastic, antitumor, medicinal herbs, neoplasms, saffron and turmeric.
In spite of the intense effort on the conduction of research aimed to cancer therapies, many patients continue to receive an unfavorable prognosis. Thus, the effort for finding anticancer treatments with better efficacy and lesser side effects has been continued. This review was focused on the beneficial effects of C. longa for various types of cancer. The main findings of these results were also summarized and discussed.
Historical Background
Compounds and antitumoral activity
C. longa or zerdeçal, is also known as turmeric in English-speaking countries, jiang huang in eastern countries, and curcuma or saffron in latin-speaking countries. Belonging to the family Zingiberaceae, turmeric is herbaceous plant, perennial that present large and long leaves and ovoid rhizomes. It is native to India and southeast of Asia, but it is spread throughout Europe and America.
The turmeric anticancer activity was evidenced by the ability to induce apoptosis (Table 1) [7-16], inhibit proliferation of different tumor types and favor metastasis reduction (Table 2) [17-27].
Inhibitory effect against angiogenesis, growth factor receptors and cell adhesion molecules involved in tumor growth was associated to the potential to reduce metastasis. Curcuminoid compounds such as demethoxycurcumin, bisdemethoxycurcumin, and tetrahydrocurcumin were isolated from turmeric root. Among the commonly isolated curcuminoids, curcumin is the most abundant, highlighting that 13 curcuminoids with anticancer activity were described [28].
Comparing the cell growth inhibition effect by pure curcumin and turmeric methanolic extract, it was presented much more effective inhibition by curcumin (half maximal inhibitory concentration (IC50) = 41.69 ± 2.87 μg mL-1) than the turmeric methanolic extract (IC50 = 196.12 ± 5.25 μg mL-1) [15]. But factors such as tumor type [7,29,30] and dose-time-dependent action [7,27,30-32] appear to interfere in anticancer activity.
Curcumin (2 μM) decreased mesenchymal cell proliferation while cell death was detected only at 50 μM. Highly migratory cells decrease on migration speed and directionality about 50% and 40% when treated with 2 or 5 μM of curcumin, respectively. In addition, the curcumin decreased cell adhesion with dose dependence, especially on tumor-derived spheroids [27].
Although the curcumin antitumor activity has been demonstrated to be important, in the same way the antitumor effect of turmeric has also been observed both in the form of extracts [23,33,34] and essential oil [14].
Studies that evaluated curcumin-free turmeric observed suppression of benzo[a] pyrene-induced tumorigenesis in mice [33] and inhibition of 7,12-dimethylbenz[a]anthracene-induced mammary tumorigenesis in rats [34]. Antiproliferative activity between curcumin and turmeric was compared in seven cancer cell lines. Both treatments presented similar amounts of curcumin, with a higher inhibition percentage for turmeric in all cell lines tested [23]. Therefore, other components than curcumin also contribute to the turmeric anticancer activities.
Curzerene is a sesquiterpene that presented dose-dependent antiproliferative effect both in vitro and in vivo test [32]. The crude turmeric methanolic extract was evaluated by gas chromatography-mass spectrometry analysis (GC-MS). 50 compounds were detected, and the major compounds were ar-turmerone (20.50%), β-sesquiphellandrene (5.20%) and curcumenol (5.11%) [15]. Recently evaluating turmeric ethanolic extract, four new sesquiterpenes were isolated [35].
Concerning the form of essential oil obtained from rhizomes, sesquiterpenes and oxygenated monoterpenes such as ar-Turmerone (33.2%), α-Turmerone (23.5%) and β-Turmerone (22.7%) were recorded using CG-MS and nuclear magnetic resonance (NMR) spectroscopy [14].
Likewise, using GC-MS to evaluate the essential oil, turmerone (35.9%) was the majority component among the 23 compounds identified [36]. Complementarily, it should be noted that beyond the direct antineoplastic effects, the indirect effects such as immunomodulatory and anti-inflammatory activities are relevant for tumor therapy (Table 3) [37-40].
Pre-clinical and clinical assays also demonstrated promising results (Table 4) [41-49]. But, although these tests were performed in mice, rats, dogs and other experimental animals, the development of research directly for veterinary medicine is scarce.
The use of curcumin associated with other cancer therapies
The combination of curcumin and cisplatin in the treatment of lung adenocarcinoma cells (A549) was favorable due to reversing tumor resistance. It was demonstrated (in vitro) the inhibition of factor induced by hypoxia-1 (FIH-α) and reduction of P-glycoprotein, these proteins are related to tumor resistance [50]. Furthermore, curcumin reduced neurotoxicity [51] and cisplastin nephrotoxicity [52].
The use associated with radiotherapy indicated that curcumin favored the action of radiation on colon cancer cells (HCT116 and HT29), increased sensitivity to this type of treatment by inhibiting nuclear factor kappa B (NF-κB) [47].
Promising results were found regards the effect of curcumin as a sensitizing agent to enhance the apoptotic potential of doxorubicin [31]. These researchers evaluated IC50 dose (5 nM) of doxorubicin and a lower dose (2.5 nM). They found that both curcumin (10 μM) and doxorubicin (5 nM) induced apoptosis. However, the association of curcumin (10 μM) with doxorubicin at a lower dose than its IC50 (2.5 nM) was able to induce a higher level of apoptosis in Pre-B acute lymphoblastic leukemia cell lines. It was also observed dose dependence which suggests enhanced level of apoptosis when curcumin was supplemented with doxorubicin in cell culture.
Unfortunately, unfavorable associations may occur mainly if high doses of curcumin are used. It was verified that 6000 mg of curcumin per day represent the limit dose capable to induce adverse effects. Higher doses (8000 mg daily) demonstrated to affect negatively the association with docetaxel in breast cancer [42]. The same association was studied in MCF7 and MDA-MB-231 breast cancer cells [29]. Curcumin at 10 mg L-1 in cotreatment with docetaxel induced modifications in glutathione and lipid metabolisms and glucose utilization. Some of these changes were biphasic depending on the exposure duration to curcumin. Thus, the continuity of research involving the use of curcumin to cancer treatment is increasingly justified. Despite the various publications in recent years, the mechanisms of action involved still need to be best clarifying, mainly when combining two active principles [29].
The association between medicinal plants may also determine benefits to oncological treatment. Curcumin associated with Zingiber officinale promoted growth inhibition of prostate cancer and presented superior results when compared to both treatments [53,54].
Contribution of C. longa in drug resistance control
One of the major obstacles to the success of chemotherapy is the fact that some tumor cells develop multidrug pharmacological resistance (MDR) [55]. This process may be associated with overexpression of efflux pumps drug. P-glycoprotein is a drug efflux pump that is often found to be overexpressed in cases of acquired MDR. However, there are no P-glycoprotein inhibitors used in current clinical practice due to toxicity problems, drug interactions or pharmacokinetic problems. Thus, it has been carried out to search for natural products that can inhibit glycoproteins such as P-glycoprotein. Curcumin has shown important inhibition [56,57], emerging as a potential drug for the antitumor treatment response.
Limiting factors of curcumin use: Bioavailability
The high metabolism and low half-life of curcumin impairs its absorption when administered orally [17,26,41,44,45,56]. Therefore, in order to increase the solubility, bioavailability and anticancer activity of curcumin, associations with liposomes [17,26,44,45], nanoparticles [43,58] and mainly piperine [59,60] have been proposed.
The incorporation of curcumin into liposomes promoted growth inhibition of pancreatic carcinoma cell lines [17]. Similarly, liposomal curcumin suppresses the growth of head and neck squamous cell carcinoma (HNSCC) cell lines CAL27 and UM-SCC1 in vitro and in vivo tests [26]. Association between curcumin and liposomes was also evaluated from intravenous infusion of 10 mg Kg-1 in dogs [44]. These results indicated high plasma concentration of curcumin two hours after infusion, suggesting that this combination may be used in plasma cell and multiple myeloma tumors. This study was also performed by Matabudul, et al. [45] and after eight hours of infusion it was observed a significant increase of curcumin in lung, spleen and liver, demonstrating that the infusion time determined a better distribution of curcumin.
The nanoparticles associated with curcumin favor physical stability with maintenance of the cytotoxic activity of this curcuminoid in cancerous cells [43,54,56].
By intravenous administration (2.5 mg Kg-1) in mice, this association increased the bioavailability of curcumin in almost two times [56]. These authors also confirmed the antiproliferative activity in human chronic myeloid leukemia (KBM-5), human T-cell leukemia (Jurkat), prostate cancer cells (DU145), breast tumor (MDA-MB-231), esophageal cancer (SEG-1) and colon cancer (line HCT116). It was demonstrated that curcumin loaded nanoparticulate formulation based on poly lactide-co-glycolide (PLGA) has enhanced cellular uptake and increased bioactivity in vitro and superior bioavailability in vivo over curcumin. They also observed increased cellular uptake of curcumin and inhibition of nuclear factor- kappa B (NF-κB) expression level.
Rats submitted to curcumin with nanoparticles by the oral route demonstrated increased solubility and bioavailability in five to six times and had a longer half-life. The results showed that the effect in improving oral bioavailability of curcumin may be associated with improved water solubility, higher release rate in the intestinal juice, enhanced absorption by improved permeability, inhibition of P-glycoprotein-mediated efflux and increased residence time in the intestinal cavity [43].
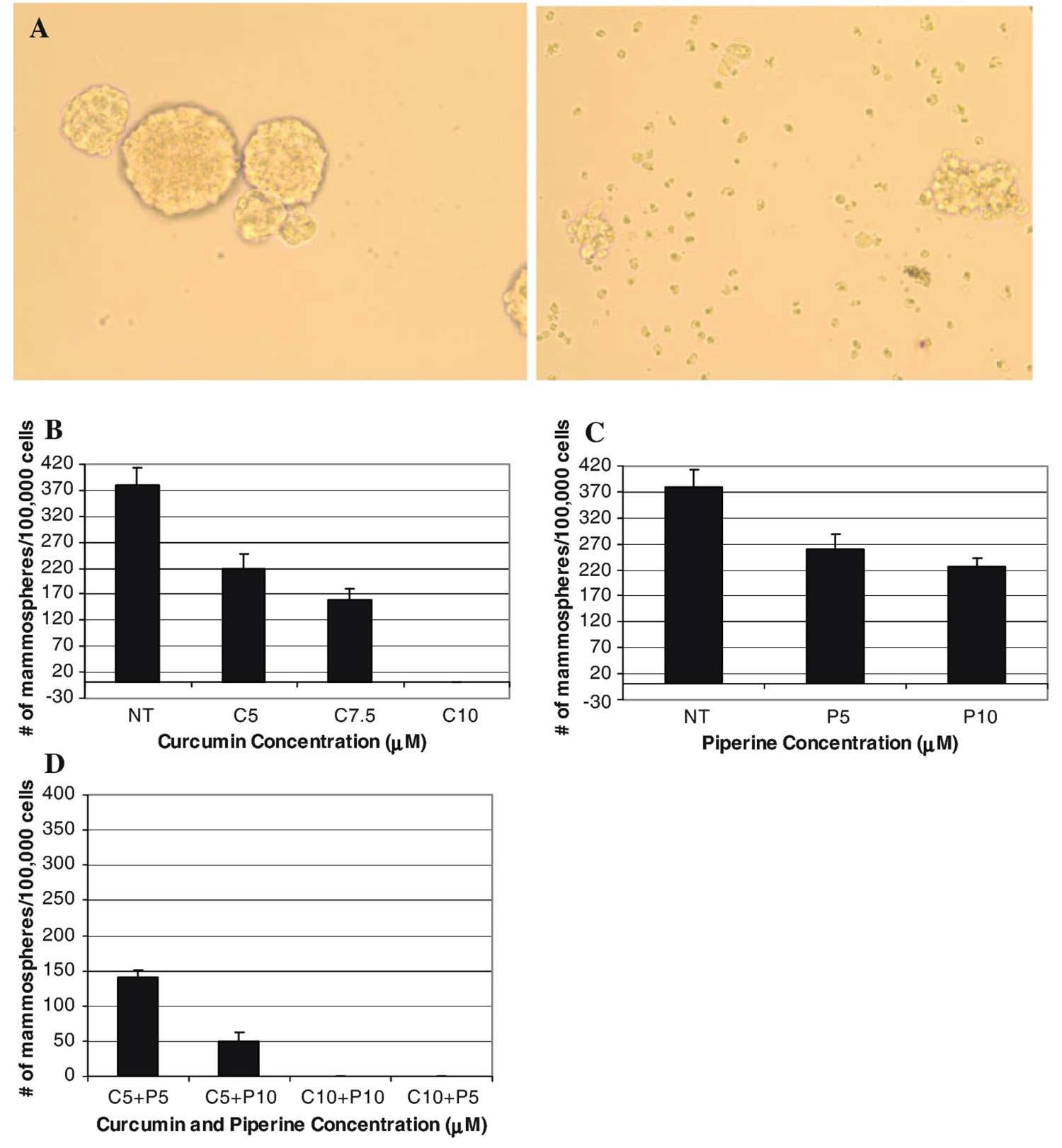
The association of curcumin with piperine, a polyphenol isolated from black peppers, increased the curcumin oral bioavailability [58,61]. In order to determine the ability to modulate the self-renewal of normal and malignant breast cells, Kakarala, et al. [58,61,62] examined multiple spheres formation trait and the expression of the breast stem cells with aldehyde marker dehydrogenase (ALDH) signaled by Wnt pathway. Both curcumin and piperine were able to inhibit the formation of the multiple beads, however, the addition of piperine to curcumin potentiated this reduction compared to the compounds used separately (Figure 1).
In addition, it is important to consider that some compounds of piperine may be able to determine some synergic action mechanism with turmeric. Genotoxicity was evaluated in hamsters induced by single dose (30 mg Kg-1) intraperitoneal injection of 7,12-dimethylbenz[a]anthracene. The curcumin association with piperine was able to potentiate its antigenotoxic effect, evidenced by the decrease of polychromatic erythrocytes and acrosomal aberrations [61,62].
Considering the antitumoral effect of β-elemene derived from Curcuma wenyujin, it was synthesized five novel β-elements from the piperazine: 13-(3-methyl-1-piperazinyl)-b-elemene (DX1), 13-(cis-3,5-dimethyl-1-piperazinyl)-b (DX2), 13-(4-isopropyl-1-piperazinyl)-b-eel (DX4) and 13-piperazinyl-b-element (DX5) [7]. These researchers reported that activation of caspase-8 by these new β-elemene, piperazine derivatives, was correlated with the decrease of cellular FLICE-like inhibitory protein (c-FLIP) levels and H2O2 production, which determined the activation of the apoptotic pathways mediated by mitochondria, suggesting the influence of a synergic action mechanism.
Conclusion
Turmeric anticancer activity was evidenced by antiproliferative, apoptotic and antimetastatic activities. Its use associated with nanoparticles, liposomes and mainly piperazine, promoted greater bioavailability of curcumin when administered orally, signaling a promising future. Additionally, the anti-inflammatory and immunomodulatory activities presented by curcumin represent an important adjuvant mechanism of control for neoplastic pathogenesis. Therefore, the results of in vitro and in vivo tests, and pre-clinical and clinical trials showed that C. longa presents evidence of prophylactic and curative effects in cancer treatment.
Conflict of Interest
The authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Acknowledgments
We would like to thank the Araucária Foundation and National Council for Scientific and Technological Development (CNPq) for the financial support and scholarships granted.
References
- Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66: 7-30.
- Tostes RA, Branco A, Cestari FK (2017) Retrospective study of canine cutaneous neoplasia. Archives of Veterinary Sciences 22: 71-80.
- Zavery B, Appleton L, Sandiford K, et al. (2013) Complementary and alternative medicine use amongst oncology patients attending a large cancer centre in England. Progress in Palliative Care 18: 89-93.
- Hosseini A, Ghorbani A (2015) Cancer therapy with phytochemicals: Evidence from clinical studies. Avicenna J Phytomed 5: 84-97.
- Damery S, Gratus C, Grieve R, et al. (2011) The use of herbal medicines by people with cancer: A cross-sectional survey. Br J Cancer 104: 927-933.
- Chiu J, Yau T, Epstein RJ (2008) Complications of traditional Chinese/herbal medicines (TCM) - a guide for perplexed oncologists and other cancer caregivers. Supportive Care Cancer 17: 231-240.
- Yue GGL, Chan BCL, Hon P, et al. (2010) Evaluation of in vitro anti-proliferative and immunomodulatory activities of compounds isolated from Curcuma longa. Food Chem Toxicol 48: 2011-2020.
- Wu SH, Hang LW, Yang JS, et al. (2010) Curcumin induces apoptosis in human non-small cell lung cancer NCI-H460 cells through ER stress and caspase cascade - and mitochondria-dependent pathways. Anticancer Res 30: 2125-2133.
- Senft C, Polacin M, Priester M, et al. (2010) The nontoxic natural compound curcumin exerts anti-proliferative, anti-migratory, and anti-invasive properties against malignant gliomas. BMC Cancer 10: 1-8.
- Bill MA, Bakan C, Benson DM, et al. (2009) Curcumin induces proapoptotic effects against human melanoma cells and modulates the cellular response to immunotherapeutic cytokines. Mol Cancer Ther 8: 2726-2735.
- Ibrahim A, El-Meligy A, Lungu G, et al. (2011) Curcumin induces apoptosis in a murine mammary gland adenocarcinoma cell line through the mitochondrial pathway. Eur J Pharmacol 668: 127-132.
- Prakobwong S, Gupta SC, Kim JH, et al. (2011) Curcumin suppresses proliferation and induces apoptosis in human biliary cancer cells through modulation of multiple cell signaling pathways. Carcinogenesis 32: 1372-1380.
- Song F, Zhang L, Yu HX, et al. (2012) The mechanism underlying proliferation-inhibitory and apoptosis-inducing effects of curcumin on papillary thyroid cancer cells. Food Chem 32: 43-50.
- Santos Pasr, Avanco GB, Nerilo SB, et al. (2016) Assessment of cytotoxic activity of rosemary (Rosmarinus officinalis L.), turmeric (Curcuma longa L.), and ginger (Zingiber officinale R.) essential oils in cervical cancer cells (Hela). Scientific World Journal 2016: 9273078.
- Abdel-Lateef E, Mahmoud F, Hammam O, et al. (2016) Bioactive chemical constituents of Curcuma longa L. rhizomes extract inhibit the growth of human hepatoma cell line (HepG2). Acta Pharm 66: 387-398.
- Mou S, Zhou Z, He Y, et al. (2017) Curcumin inhibits cell proliferation and promotes apoptosis of laryngeal cancer cells through Bcl-2 And PI3k/Akt, and by upregulating mir- Oncol Lett 14: 4937-4942.
- Li L, Braiteh FS, Kurzrock R (2005) Liposome-encapsulated curcumin in vitro and in vivo effects on proliferation, apoptosis, signaling, and angiogenesis. Cancer 104: 1322-1331.
- Lu W, Tinsley HN, Keeton A, et al. (2009) Suppression of Wnt/β-catenin signaling inhibits prostate cancer cell proliferation. Eur J Pharmacol 602: 8-14.
- Cai XZ, Wang J, Xiao-Dong L, et al. (2009) curcumin suppresses proliferation and invasion in human gastric cancer cells by downregulation of PAK1 activity and cyclin D1 Cancer Bio Ther 8: 1360-1368.
- Saha A, Kuzuhara T, Echigo N, et al. (2010) Apoptosis of human lung cancer cells by curcumin mediated through up-regulation of "Growth arrest and DNA damage inducible genes 45 And 153". Biological and Pharmaceutical Bulletin 33: 1291-1299.
- Mudduluru G, George-William JN, Muppala S, et al. (2011) Curcumin regulates mir-21 expression and inhibits invasion and metastasis in colorectal cancer. Biosci Rep 31: 185-197.
- Teiten M, Gaascht F, Cronauer M, et al. (2011) Anti-proliferative potential of curcumin in androgen dependent prostate cancer cells occurs through modulation of the wingless signaling pathway. Int J Oncol 38: 603-611.
- Kim JH, Gupta SC, Park B, et al. (2011) Turmeric (Curcuma longa) inhibits inflammatory nuclear factor (Nf)-Κb and Nf-Κb-regulated gene products and induces death receptors leading to suppressed proliferation, induced chemosensitization, and suppressed osteoclastogenesis. Mol Nutr Food Res 56: 454-465.
- Tsai K, Lin JC, Yang SM, et al. (2012) Curcumin protects against uvb-induced skin cancers in skh-1 hairless mouse: Analysis of early molecular markers in carcinogenesis. Evid Based Complement and Alternat Med 2012: 1-11.
- Li Y, Zhang J, Ma D, et al. (2012) Curcumin inhibits proliferation and invasion of osteosarcoma cells through inactivation of Notch-1 signaling. Febs J 279: 2247-2259.
- Wang D, Veena MS, Stevenson K, et al. (2008) Liposome-encapsulated curcumin suppresses growth of head and neck squamous cell carcinoma in vitro and in xenografts through the inhibition of nuclear factor κb by an akt-independent pathway. Clin Cancer Res 14: 6228-6236.
- Campos PS, Matte BF, Diel LF, et al. (2017) Low doses of curcuma longa modulates cell migration and cell-cell adhesion. Phytother Res 31: 1433-1440.
- Jiang J, Jin X, Zhang H, et al. (2012) Identification of antitumor constituents in curcuminoids from curcuma longa based on the composition-activity relationship. J Pharm Biomed Anal 70: 664-670.
- Bayet-Robert M, Morvan D (2013) Metabolomics reveals metabolic targets and biphasic responses in breast cancer cells treated by curcumin alone and in association with docetaxel. PLoS One 8: e57971.
- Sankpal UT, Nagaraju GP, Gottipolu SR, et al. (2015) Combination of tolfenamic acid and curcumin induces colon cancer cell growth inhibition through modulating specific transcription factors and reactive oxygen species. Oncotarget 7: 3186-3200.
- Mishra D, Singh S, Narayan G (2016) Curcumin induces apoptosis in pre-b acute lymphoblastic leukemia cell lines via parp-1 cleavage. Asian Pac J Cancer Prev 17: 3865-3869.
- Wang Y, Li J, Guo J, et al. (2016) Cytotoxic and antitumor effects of curzerene from curcuma longa. Planta Med 83: 23-29.
- Deshpande SS, Ingle AD, Maru GB (1997) Inhibitory effects of curcumin-free aqueous turmeric extract on benzo[a]pyrene-induced forestomach papillomas in mice. Cancer Lett 118: 79-85.
- Deshpande SS, Ingle AD, Maru GB (1998) Chemopreventive efficacy of curcumin-free aqueous turmeric extract in 7,12-dimethylbenz[a]anthracene-induced rat mammary tumorigenesis. Cancer Lett 123: 35-40.
- Wen J, Qiu T, Yan X, et al. (2017) Four novel bisabolane-type sesquiterpenes from curcuma longa. J Asian Nat Prod Res 20: 928-933.
- Oyemitan IA, Elusiyan CA, Onifade AO, et al. (2017) Neuropharmacological profile and chemical analysis of fresh rhizome essential oil of curcuma longa (turmeric) cultivated in Southwest Nigeria. Toxicol Rep 4: 391-398.
- Basnet P, Skalko-Basnet N (2011) Curcumin: An anti-inflammatory molecule from a curry spice on the path to cancer treatment. Molecules 16: 4567-4598.
- Huang S, Pettaway CA, Uehara H, et al. (2001) Blockade of Nf-kappaB activity in human prostate cancer cells is associated with suppression of angiogenesis, invasion, and metastasis. Oncogene 20: 4188-4197.
- Bhattacharyya S, Mandal D, Sen GS, et al. (2007) Tumor-induced oxidative stress perturbs nuclear factor-κappaB activity-augmenting tumor necrosis factor-a-mediated t-cell death: Protection by curcumin. Cancer Res 67: 362-370.
- Zong H, Wang F, Fan Q, et al. (2011) Curcumin inhibits metastatic progression of breast cancer cell through suppression of urokinase-type plasminogen activator by Nf-kappaβ signaling pathways. Mol Biol Rep 39: 4803-4808.
- Garcea G, Berry DP, Jones DJL, et al. (2005) Consumption of the putative chemopreventive agent curcumin by cancer patients: Assessment of curcumin levels in the colorectum and their pharmacodynamic consequences. Cancer Epidemiol Biomarkers Prev 14: 120-125.
- Bayet-Robert M, Kwiatkowski F, Leheurteur M, et al. (2010) Phase I dose escalation trial of docetaxel plus curcumin in patients with advanced and metastatic breast cancer. Cancer Biol Ther 9: 8-14.
- Xie X, Tao Q, Zou Y, et al. (2011) PLGA nanoparticles improve the oral bioavailability of curcumin in rats: Characterizations and mechanisms. J Agric Food Chem 59: 9280-9289.
- Helson L, Bolger G, Majeed M, et al. (2012) Infusion pharmacokinetics of lipocurc™ (Liposomal curcumin) and its metabolite tetrahydrocurcumin in beagle dogs. Anticancer Res 32: 4365-4370.
- Matabudul D, Pucaj K, Bolger G, et al. (2012) Tissue distribution of (Lipocurc™) liposomal curcumin and tetrahydrocurcumin following two- and eight-hour infusions in beagle dogs. Anticancer Res 32: 4359-4364.
- Morsy MA, Ibrahim SA, Amin EF, et al. (2013) Curcumin ameliorates methotrexate-induced nephrotoxicity in rats. Adv Pharmacol Sci 2013: 387071.
- Sandur SK, Deorukhkar A, Pandey MK, et al. (2009) Curcumin modulates the radiosensitivity of colorectal cancer cells by suppressing constitutive and inducible Nf-kb activity. Int J Radiat Oncol Biol Phys 75: 534-542.
- Meng H, Fu G, Shen J, et al. (2017) Ameliorative effect of daidzein on cisplatin-induced nephrotoxicity in mice via modulation of inflammation, oxidative stress, and cell death. Oxid Med Cell Longev 2017: 3140680.
- Wu J, Pan X, Fu H, et al. (2017) Effect of curcumin on glycerol-induced acute kidney injury in rats. Sci Rep 7: 10114.
- Ye M, Zhao Y, Li Y, et al. (2012) Curcumin reverses cis-platin resistance and promotes human lung adenocarcinoma A549/DDP cell apoptosis through Hif-1α and caspase-3 mechanisms. phytomedicine 19: 779-787.
- Mendonca LM, Machado CS, Teixeira CCC, et al. (2013) Curcumin reduces cisplatin-induced neurotoxicity in NGF-differentiated PC12 cells. Neurotoxicology 34: 205-211.
- Ueki M, Ueno M, Morishita J, et al. (2013) Curcumin ameliorates cisplatin-induced nephrotoxicity by inhibiting renal inflammation in mice. J Biosci Bioeng 115: 547-551.
- Kurapati KR, Samikkannu T, Kadiyala DB, et al. (2012) Combinatorial cytotoxic effects of curcuma longa and Zingiber officinale on the PC-3m prostate cancer cell line. J Basic Clin Physiol Pharmacol 23: 139-146.
- Yang QQ, Cheng LZ, Zhang T,et al. (2020) Phenolic profiles, antioxidant, and antiproliferative activities of turmeric (Curcuma longa). Industrial Crops and Products 152: 112561.
- Huber PC, Maruiama CH, Almeida WP (2010) Glicoproteina-P, resistencia a multiplas drogas (mdr) e relacao estrutura-atividade de moduladores. Quim Nova 33: 2148-2154.
- Neerati P, Sudhakar YA, Kanwar J (2013) Curcumin regulates colon cancer by inhibiting p-glycoprotein in in-situ cancerous colon perfusion rat model. J Cancer Sci Ther 5: 313-319.
- Lopes-Rodrigues V, Oliveira A, Correia-Da-Silva M, et al. (2017) A novel curcumin derivative which inhibits p-glycoprotein, arrests cell cycle and induces apoptosis in multidrug resistance cells. Bioorg Med Chem 25: 581-596.
- Anand P, Nair HB, Sung B, et al. (2010) Design of curcumin loaded PLGA nanoparticles formulation with enhanced cellular uptake, and increased bioactivity in vitro and superior bioavailability in vivo. Biochem Pharmacol 79: 330-338.
- Shaikh J, Ankola DD, Beniwal V, et al. (2009) Nanoparticle encapsulation improves oral bioavailability of curcumin by at least 9-fold when compared to curcumin administered with piperine as absorption enhancer. Eur J Pharm Sci 37: 223-230.
- Kakarala M, Brenner DE, Korkaya H, et al. (2009) Targeting breast stem cells with the cancer preventive compounds curcumin and piperine. Breast Cancer Res Treat 122: 777-785.
- Balakrishnan S, Vellaichamy L, Menon VP, et al. (2008) Antigenotoxic effects of curcumin and piperine alone or in combination against 7,12-dimethylbenz(a)anthracene induced genotoxicity in Bone marrow of golden syrian hamsters. Toxicol Mech Methods 18: 691-696.
- Paradkar PH, Juvekar AS, Barkume MS, et al. (2021) In vitro and In vivo evaluation of a standardized haridra (Curcuma longa linn) formulation in cervical cancer. Journal of Ayurveda and Integrative Medicine 12: 616-622.
Corresponding Author
Regildo Márcio Gonçalves da Silva, Department of Biotechnology, Laboratory of Herbal Medicine and Natural Products, Faculty of Sciences, Humanities and Languages, São Paulo State University (UNESP), Assis, São Paulo, Dom Antonio Avenue 2100, 19806-900, Brazil, Tel: +55-18-33025800
Copyright
© 2022 Peixoto ECTDM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.