Functional Results of the Management of Carpometacarpal Dislocations of the Long Fingers: A Series of 11 Cases
Abstract
Introduction: Dislocations of the carpometacarpal joint of the fingers are infrequent, accounting for less than 1% of all injuries of the hand. We reported the functional results of 11 cases of CMC dislocations, presented the epidemiological, clinical and management characteristics of these lesions.
Patients and methods: We conducted a retrospective study with the prospective collection over 2 years including all the patients, who presented a carpometacarpal dislocation from 2 to 5 rays with a minimum follow-up of 6 months. Quick DASH score and PRWE score were used to assess functional outcomes.
Results: Eleven patients were collected, including 9 men and 2 women, mean age was 33-years-old. The dislocation was simple in 3 cases and complex in 8 cases. The displacement of the dislocation was convergent in 10 cases. The dislocation was classified as complete spatular in 4 cases (36.36%), partial spatular in 4 cases as well, and isolated spatular in 3 cases. The definitive treatment was surgical in 8 cases. Complications were noted more in patients who had undergone intramedullary pinning than a direct cross pinning of the metacarpal bases. The average clamping force was 77.27, The average PRWE score was 73.5 with extremes of 20.5 to 90.5 and the average Quick Dash score at 3 months was 24.8 and at 6 months 21.7.
Conclusion: CMC dislocations of long fingers are rare lesions. Intramedullary spotting appears to be linked to a rate of complications such as stiffness and chronic pain over the long term.
Keywords
Osteosynthesis, Stiffness, Wrist, Carpometacarpal joint, Dorsal, Palmar carpometacarpal dislocation
Introduction
Dislocations of the carpometacarpal joint (CMC) of the fingers are uncommon injuries, representing less than 1% of all injuries to the hand and wrist, and are most commonly seen during high kinetic trauma with associated carpal or metacarpal injuries [1-10]. Often converging dorsally in more than 85%, or rarely palmar and in some cases, the displacement of the metacarpals is divergent [11,12]. These lesions are characterised by their difficult diagnosis with a clinical presentation dominated by very significant oedema of the hand and X-rays are difficult to interpret due to this geometric complexity of the CMC lines, thus increasing the risk of diagnostic error. A CT scan could be of great help in confirming the diagnosis [9,13-16]. The functional outcome of lesions that are managed early is often excellent; in neglected or poorly managed forms, they are the source of significant functional disability of the hand and wrist. We report the functional results of 11 cases of CMC dislocations and present the epidemiological and clinical characteristics and management of these lesions.
Materials and Methods
We conducted a retrospective study with prospective data collection in the department of trauma surgery and orthopaedics, Wing 4 of the Ibn Rochd University Hospital in Casablanca, for 2-years from January 2018 to December 2020, including all patients who had suffered a carpometacarpal dislocation of the 2nd to 5th fingers and excluding the dislocation of the thumb.
All patients with complete records were included in our series. Non-operative and surgically treated patients were followed up at 3 months, 6 months and some at more than 12 months, and the minimum follow-up was 6 months for all patients.
The following variables were studied: Age, sex, dominant and affected side, time to consultation and management, traumatic mechanism, the direction of dislocation, associated lesions, clinical examination assessing the presence or absence of oedema or deformity, presence or absence of a skin opening, and the existence of vascular or nerve signs and other remote lesions. The X-ray assessment of the hand included an AP X-ray face, lateral view and oblique view and a CT scan of the hand was requested to look for associated lesions of the carpal or metacarpal.
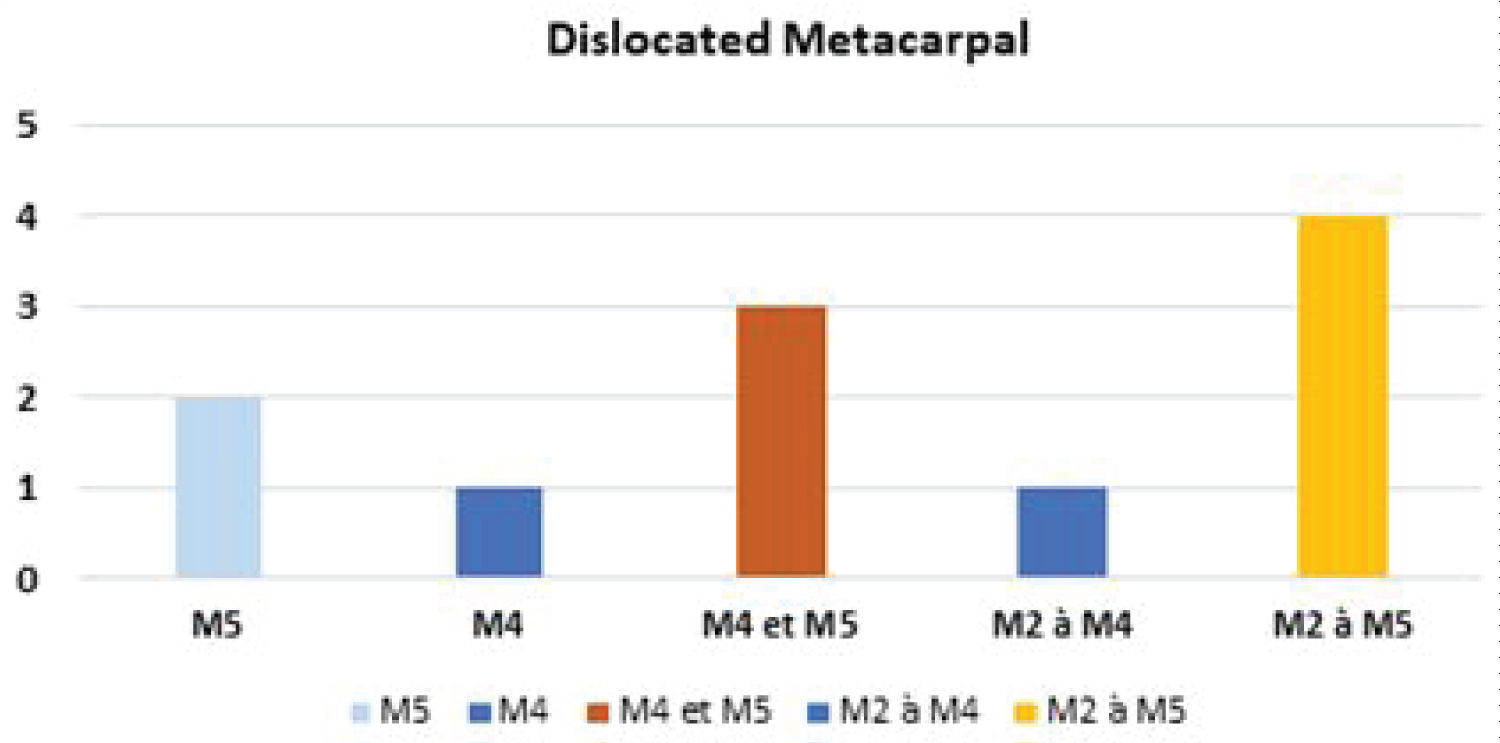
Dislocations were classified as convergent or divergent, and as dorsal, palmar, and lateral. The spatular character was considered for the last 4 rays, thus separating them into complete spatular when the dislocation involved all 4 fingers, partial spatular for the dislocation of 2 or 3 fingers and isolated spatular when it involved only one ray.
The delay in management was assessed and its impact on prognosis evaluated. The reduction was performed in some patients before the decision was made whether or not to proceed with surgery. Fixation was performed, either closed or open focus, and associated capsuloligamentous lesions were investigated and repaired. Different types of pinning were performed and evaluated in the results, and immobilization with a short arm cast for 6 weeks was performed in patients treated orthopedically and even after surgery.
All patients were assessed for postoperative X-rays after removal of the immobilization, clamping force and return to work. Postoperative and immobilization-related complications were investigated.
The Quick DASH score was used to assess functional outcome at 3 and 6 months, this score ranged from 0 to 100, with 0 corresponding to normal function, and 100 to almost no function. The Patient-Rated Wrist Evaluation (PRWE) score was also studied to assess the outcomes of the series. Descriptive analysis was performed on all baseline variables. The results are presented as means, percentages, or figures.
Results
During the study period, we collected 11 patients, including 9 men and 2 women with a sex ratio of 4.5. The average age of the series was 33 years with extremes ranging from 21 years to 43 years; 90.91% of the patients had the right hand as the dominant hand, the affected side concerned the right hand in 7 cases and the left hand in 4 cases, thus the dominant hand was affected in 7 cases.
The main aetiology observed in the series was road traffic accidents in 6 cases (54.55%), sports accidents in 3 cases (27.27%) and defenestration in 2 cases (18.18%). Smoking was noted as the main antecedent in 9 cases (81.81%). The average consultation time was 33 hours, including 8 cases within 24 hours of the trauma, 2 cases between 24 and 48 hours, and 1 case beyond 72 hours after the trauma.
One hundred per cent (100%) of the patients examined had pain and swelling of the hand, with deformity observed in more than half of the cases, 6 cases (54.55%), one patient had a punctiform skin opening, 1 case had a sensory deficit of the dorsal aspect of the ulnar border, no vascular involvement was observed in the series.
AP and oblique X-rays of the hand were requested in all patients, and CT scans with 3D reconstruction in 6 cases (54.55%) and not done in 5 cases (45.45%).
Of the 11 cases, the dislocation was simple in 3 cases and complex in 8 cases. The displacement of the dislocation was convergent in 10 cases with a dorsal displacement in 9 cases (81.82%), palmar in 1 case (9.09%), and divergent in 1 case (9.09%).
The dislocation was classified as complete spatular in 4 cases (36.36%), partial spatular in 4 cases and isolated spatular in 3 cases (Figure 1).
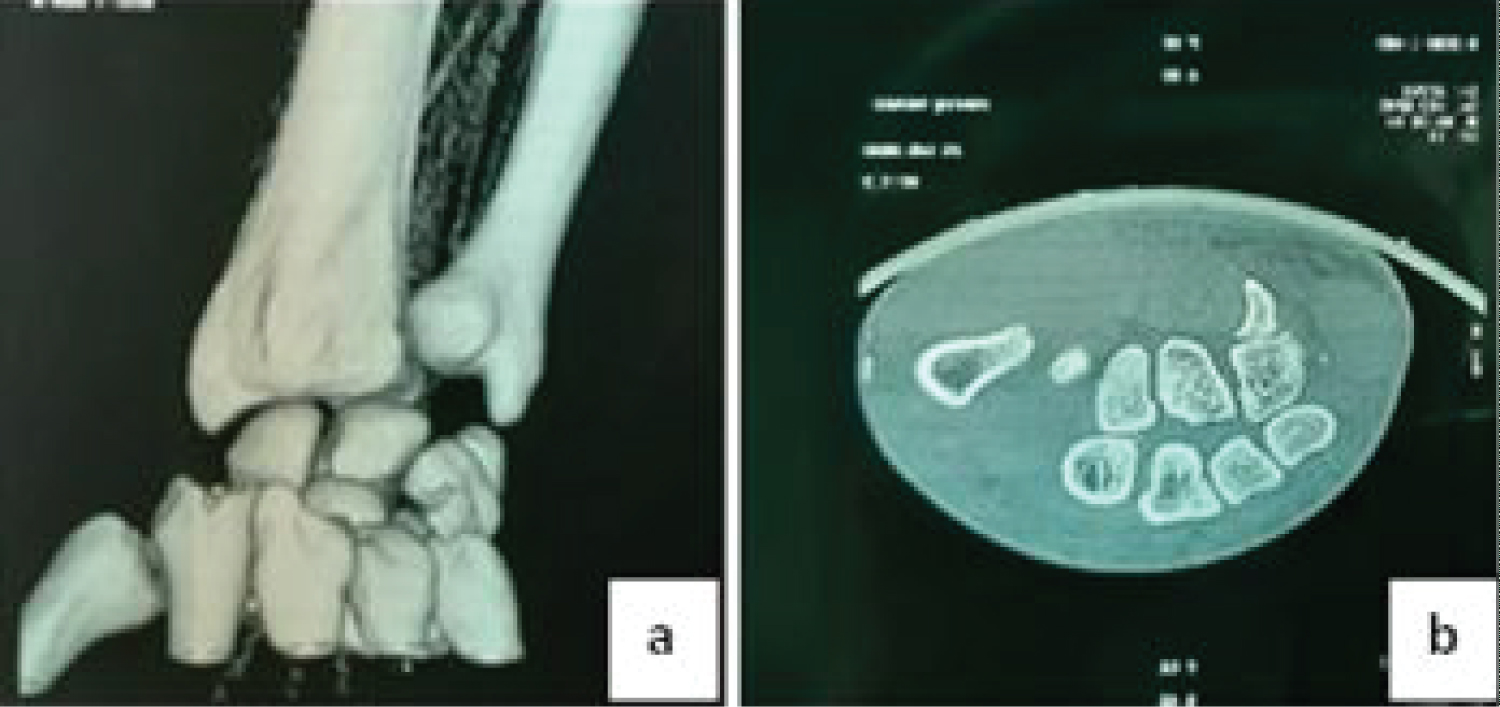
The associated lesions noted in the series were a fracture of the base of the 2nd metacarpal in 2 cases, of the base of the 3rd metacarpal in 2 cases, of the base of the 4th metacarpal in 3 cases, and the base of the 5th metacarpal in 5 cases. The CT scan revealed, in addition to the fractures of the metacarpal bases, the fracture of the hamatum in 1 case (Figure 2).
Associated remote injuries included dislocation of the metacarpophalangeal joint of the 5th finger in 1 case and an unfortunately terrible triad of the elbow in 1 case.
The average time between diagnosis and treatment was 1.73 days, with 5 cases within 24 hours, 2 cases between 24 and 48 hours, and 2 cases beyond 72 hours. The emergency reduction was successful in 8 cases (72.73%) and unsuccessful in 3 cases (27.27%). Post-reduction instability was noted in 3 cases (18.18%).
The final treatment was orthopaedics in 3 cases and surgical in 8 cases. Of the 8 cases treated surgically, auxiliary plexus blockade was used in 7 cases and general anaesthesia in 1 case. The surgical treatment was closed in 3 cases and open in 5 cases (Figure 3). The approach was dorsal in 5 cases. In 1 case of the operated patients, a lesion of the posterior capsule was noted and in 4 cases no lesion of the posterior capsule was noted. Of the 8 patients operated on, wire splinting was intramedullary in 4 cases, intramedullary and transverse pinning in 2 cases and cross pinning in 2 cases (Figure 4).
All patients were immobilized with a short arm cast in 10 cases and a brachio-ante-brachio-palmar cast in 1 case for 6 weeks. The wires were removed at 6 weeks in the cases of patients with intramedullary wires, and at 2 months in the case of patients for who the cross-wire splinting had been carried out. The average follow-up time was 6.64 months, with extremes of months 6 and 16 months.
Complications were dominated by infections on k-wire in 2 cases, 1 case of hand stiffness and chronic pain, 1 case of wrist arthrosis, 1 case of algodystrophy, mainly in patients with total spatular dislocation. There were more complications in patients with intramedullary wire splinting than a direct cross pinning of the metacarpal bases.
No revision surgery was performed in the series. The average clamping force was 77.27 with extremes 25 to 100, and in 10 cases the patients had returned to their previous activities at 3 months, and 1 patient who had a dislocation of elbow associated had lost his job due to a clamping force of 25 and stiffness of elbow and wrist metacarpophalangeal joints (Figure 5).
The mean PRWE score was 73.5 with extremes from 20.5 to 90.5. The Quick DASH score was excellent in 1 case at 3 months, good in 4 cases, satisfied in 4 cases and poor in 2 cases at 3 months; and at 6 months follow-up, excellent results were noted in 3 cases, good in 4 cases, satisfied in 2 cases and poor in 2 cases. The mean Quick Dash score at 3 months was 24.8 and at 6 months 21.7.
Discussion
Dislocations of the carpometacarpal joint (CMC) of the fingers represent less than 1% of all injuries to the hand and wrist and are an entity of the young subject during high kinetic trauma. These infrequent injuries are often accompanied by complete or partial fractures of the carpal or metacarpal bones. In our series, 81.82% of the displacement was convergent and dorsal, a result which is similar to those of the literature, where nearly 85% of the cases were convergent and dorsally displaced. Palmar forms are relatively rare lesions, the first historical cases of which were described by Rivington in 1873 [17]. Since then, several isolated cases of palmar carpometacarpal dislocation have been mentioned in the literature with direct dorsal trauma as the main mechanism in the case of direct dorsal trauma, we noted a rare and isolated form of palmar dislocation of the 4th ray of the CMC (Figure 4), these isolated dislocations most often concern the peripheral rays, as emphasised by D. Gangl off, et al. who reported, in a series of 31 cases, isolated dislocation of the carpometacarpal of the 5th finger with a dorsal predominance in the displacement [18].
But in rare cases, the displacement of the metacarpals may be divergent. Divergent varieties are exceptional and are thought to result from a compound traumatic mechanism [2,12,19-21] . One case of divergent dislocation was noted in our series.
These dislocations are usually accompanied by damage to neurovascular structures such as the dorsal sensitive branch of the ulnar nerve, which is closely related to the carpometacarpal joint of the fifth finger, or the deep palmar arch with the carpometacarpal joint, which may be damaged in dislocations with palmar displacement. One case in our series was accompanied by hypoesthesia of the ulnar border of the hand with good recovery after reduction, and no neurovascular damage was noted in the series at a distance.
These dislocations are characterised by their diagnostic difficulty with a clinical presentation dominated by very significant oedema of the hand and that standard radiographs remain difficult to interpret, thus increasing the risk of diagnosis error. In case of doubt, many authors recommend a longitudinal CT study for diagnosis and thus detect associated lesions that have gone unnoticed on standard X-rays.
In almost half of the cases (54.55%) in the series, a CT scan was necessary to assess associated lesions, in one case involving a fracture of the base of the unciform process of the hamulus, as well as osteochondral lesions of the metacarpal bases. A CT scan may be necessary at the slightest doubt to confirm the diagnosis and avoid the diagnosis of these lesions at a neglected stage, which is often difficult to manage and often have a poor prognosis.
The treatment of acute, displaced or unstable forms after reduction is almost always surgical. Pinning with arthrorise or arthrodesis from the outset remains the technique of choice for these injuries. Stabilization with k-wire in the carpometacarpal joint remains the best option for these injuries; it can be oblique, especially for peripheral metacarpals, intramedullary or crosswise. In our series, complete spatular dislocations treated by intramedullary pinning with a point of introduction at the level of the metacarpal heads were often accompanied by stiffness, chronic pain of the metacarpophalangeal joint and delayed early mobilisation of the hand joints. And in partial or isolated forms, pinning with a cross or transverse arthrodesis of the carpometacarpal had been used with support on the adjacent unharmed beam.
We opted for a 6 weeks immobilization in our series, but this varies greatly according to the authors, the majority of them, however, are unanimous in favour of using a splint in the intrinsic position, which is maintained for 5 to 6 weeks.
The Quick Dash score was significantly worse in patients with complete spatular complex dislocation at 3 months, but improved at 6 months, with an average Quick Dash score of 24.8 at 3 months and 21.7 at 6 months. The result was poor in cases with associated lesions, there were 2 poor long-term results in the series, one associated with an unfortunate ipsilateral triad with the stiffness of both elbow and hand, and the other related to a divergent carpometacarpal dislocation was marked by an equally unfavourable evolution.
Conclusion
Complete carpometacarpal dislocations of the long fingers are very rare injuries. They require an early and accurate diagnosis to allow adequate initial management, which guarantees a favourable long-term functional prognosis. Open or closed CMC pinning is the treatment of choice for this type of lesion. Intramedullary pinning seems to be associated with a higher rate of complications such as stiffness and chronic pain in the long term.
Conflicts of Interest
None.
References
- Gibson MF, Clancy MJ (1990) Carpometacarpal dislocation: An unusual complex injury of the hand. Arch Emerg Med 7: 56-57.
- Lawlis JF, Gunther SF (1991) Carpometacarpal dislocations. Long-term follow-up. J Bone Joint Surg Am 73: 52-59.
- Pérez Serna AG, Figueroa-Cal y Mayor F (2009) Multiple carpometacarpal fracture-dislocation. Acta Ortop Mex 23: 149-152.
- Pundkare GT, Patil AM (2015) carpometacarpal joint fracture dislocation of second to fifth finger. Clin Orthop Surg 7: 430-435.
- Jumeau H, Lechien P, Dupriez F (2016) Conservative treatment of carpometacarpal dislocation of the three last fingers. Case Rep Emerg Med 2016: 1-3.
- Garcia Elias M, Rossignani P, Cots M (1996) Combined fracture of the hook of the hamate and palmar dislocation of the fifth carpometacarpal joint. J Hand Surg Br 21: 446-450.
- Jiménez I, Dury M (2017) Combined perihamateperipisiform and peritrapezium open axial carpal dislocation: Description of a new pattern of crush injury. Hand (N Y) 12: 73-77.
- Gil JA, Goodman AD, Starr A (2017) Coronal hamate fracture associated with carpometacarpal dislocations of all of the fingers: Review of the literature and case report. Hand (N Y) 12: 51-54.
- Brinkman JN, Hartholt KA, De Vries MR (2016) Multiple carpometacarpal dislocations and an associated fracture of the hamate: An uncommon injury. BMJ Case Rep 2016: bcr2015213106.
- Motomiya M, Tazaki Y, Iwasaki N (2015) Various diagnostic and treatment pitfalls of combined fracture dislocations of trapezoid and multiple carpometacarpal joints. Hand Surg 20: 325-329.
- Masquelet AC, Nordin JY, Savary L, et al. (1986) Case of volar dislocation of 4 ulnar metacarpals. Ann Chir Main 5: 63-66.
- Hani R, Jeddi I, Berrada MS (2018) Divergent dislocation of the carpometacarpal joints: A case report. J Med Case Rep 12: 157.
- Soubeyrand M, Apard T, Crézé M (2019) Luxations carpométacarpiennes. EMC - Appareil locomoteur 14: 1-16.
- Frick L, Mezzadri G, Yzem I, et al. (2011) Luxations carpométacarpiennes fraîches des doigts longs. Étude à propos de 100 cas. Chirurgie de la Main 30: 333-339.
- Yoshida R, Obopilwe E, Rodner CM (2018) Biomechanical comparison of fifth carpometacarpal fusion methods: Kirschner wires versus plate and screws. Tech Orthop 33: 271-273.
- Valente L, Sousa A, Gonçalves AM, et al. (2007) Fracture of the hamate with carpometacarpal dislocation. Acta Med Port 20: 179-184.
- Tsepelidis D, Schuind F (2014) Luxation carpométacarpienne palmaire du cinquième doigt : A propos d’un cas. Chirurgie de la Main 33: 227-230.
- Gangloff D, Mansat P, Gaston A, et al. (2007) Carpometacarpal dislocation of the fifth finger: A descriptive study of 31 cases. Chir Main 26: 206-213.
- Dlimi F, El Bardouni A, Lahlou A, et al. (2011) Luxation carpométacarpienne divergente des doigts longs : A propos d’un cas. Journal de Traumatologie du Sport 28: 194-196.
- Mestagh A, D’Ambreville A (1976) Les luxations carpométacarpiennes. Lille Chir 31: 37-42.
- Pundkare GT, Deshpande SS (2018) Proposal for a radiological classification system for carpo-metacarpal joint dislocations with or without fractures. Malays Orthop J 12: 42-46.
Corresponding Author
Dr. Zengui Francis Zifa, Resident, Department of Trauma Surgery and Orthopaedic, Hospital University Center Ibn Rochd of Casablanca, 8 Rue Lahcen El Arjoun Casablanca 20100, Morocco
Copyright
© 2022 Zengui ZF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.