Outcomes of Extended Trochanteric Osteotomy in Revision Total Hip Arthroplasty for Periprosthetic Joint Infection: A Systematic Review
Abstract
Background: Extended trochanteric osteotomy (ETO) is a technique to remove well-fixed femoral stems in revision total hip arthroplasty (THA). ETO is commonly utilized in the setting of chronic periprosthetic joint infection (PJI). This article presents a systematic review concerning outcomes after ETO in the setting of PJI.
Methods: The US National Library of Medicine (Pubmed/MEDLINE) and Embase were searched from 1980 to 2020 for publications using the keywords: ("extended" AND "trochanteric" AND "osteotomy" AND "infection"). The inclusion criteria were the following: (1) Human subjects of any age or gender, (2) Outcomes after two-stage exchange revision THA with ETO in patients with chronic periprosthetic joint infection, (3) Minimum of two years follow-up, (4) Minimum ten subjects, and (5) Included a measurable outcome (PROs, complication rates, functional scores, pain scale, union rate, or stem subsidence rate). Studies that did not delineate outcomes between aseptic vs. septic revision THAs were also excluded.
Results: Following the PRISMA guideline for systematic reviews, six papers were analyzed comprising a total of 285 unique ETOs. The cohort included 140 male patients (50%). The average age was 64.9 years. The mean length of follow-up was 60.4 months. All ETOs were initiated in Stage 1 surgery and 96 required reopening in Stage 2 surgery. The ETO union rate was 94% with a mean time to union of 12.0 weeks. Complications included intraoperative fracture (8.4%), dislocation (7.0%), stem subsidence (6.0%), and aseptic loosening (1.1%). The average improvement in Harris Hip Score was 45.5 points. Reinfection free survival was achieved in 94.1% of cases.
Conclusions: There is moderate quality evidence to support that ETO is safe and effective technique for patients undergoing THA revision for chronic PJI. ETO has a high union rate and does not appear to increase risk of infection recurrence or aseptic loosening. ETO is recommended in revision THA cases for PJI involving well-fixed femoral stems.
Keywords
ETO: Extended trochanteric osteotomy, Total hip arthroplasty, Revision total hip arthroplasty, Periprosthetic joint infection
Introduction
As the incidence of total hip arthroplasty (THA) continues to rise, demand for revision THA is also increasing [1-4]. Instability, aseptic loosening, and periprosthetic joint infection (PJI) are the most common indications for revision hip replacement [2,5]. Compared to primary THA, revision THA carries a higher risk of intraoperative and postoperative complications including fracture, infection, dislocation, and reoperation [6-8]. Understanding how to best manage this challenging patient population is crucial to optimize surgical outcomes.
Extended trochanteric osteotomy (ETO) has been popularized as a technique to safely and efficiently remove femoral implants in revision hip arthroplasty [9]. Via a controlled opening of the proximal femur, this technique allows the surgeon to access the medullary canal and manipulate the femoral component while minimizing damage to remaining bone stock and the abductor musculature. Wide femoral exposure facilitates component removal, cement removal, reaming, debridement, and preparation of a new implant insertion while minimizing surgical complications such as canal perforation, trochanteric fracture, and shaft fracture [3,8].
Though useful in a multitude of revision indications, one of the more common situations for ETO is component removal for chronic periprosthetic joint infection (PJI) [3,5,10,11]. Approximately 1% of primary THAs are complicated by PJI [12]. The gold standard for PJI following THA is two-stage exchange with implant removal followed by spacer, antimicrobial therapy, and delayed reimplantation. In these cases, ETO is often necessary for well-fixed component removal and also facilitates thorough debridement of the femoral canal to prepare for revision prosthesis implantation [13-15].
While multiple studies demonstrate improved outcomes with ETO in revision THA, these studies do not analyze the outcomes of revision THA with ETO for PJI separately from other revision indications [16-23]. Unlike revision of non-septic THA, revision of an infected hip arthroplasty often requires a planned two-stage approach for revision including placement of an antibiotic spacer and infection eradication before reimplantation. Additionally, infected THA often result in superimposed osteomyelitis with reactive bone formation, which may compromise the bone quality and healing potential. Due to the increased complexity of revision THA for chronic periprosthetic infection, it is unclear whether these generalized findings can be applied to patients undergoing revision THA for PJI.
Several publications have investigated the outcomes after ETO in revision THA for chronic periprosthetic joint infection. To improve the quality of conclusions, we conducted a systematic review to assess the efficacy and outcomes of ETO in revision THA for chronic periprosthetic infection. The goal of this study is to compile and characterize patient demographics, complications, and clinical outcomes following ETO in the treatment of infected THA.
Materials & Methods
Search criteria
The US National Library of Medicine (PubMed/MEDLINE) and Embase data bases were searched for publications from January 1, 1980 to November 1, 2020 using the following query: ("extended" AND "trochanteric" AND "osteotomy" AND "infection"). Abstracts that evaluated the outcomes after extended troch anteric osteotomy (ETO) in patients under going revision hip replacement for chronic peri-prosthetic joint infection were reviewed according to inclusion criteria.
Inclusion and exclusion criteria
The inclusion criteria were the following: (1) Human subjects of any age or gender, (2) Outcomes after two-stage exchange revision total hip arthroplasty (THA) with ETO in patients with chronic periprosthetic joint infection, (3) Minimum of two years follow-up, (4) Minimum ten subjects, and (5) Included a measurable outcome (patient reported outcomes, complication rates, functional scores, pain scale, union rate, or stem subsidence rate). Studies that did not delineate outcomes between aseptic vs. septic revision THAs were also excluded.
Data collection
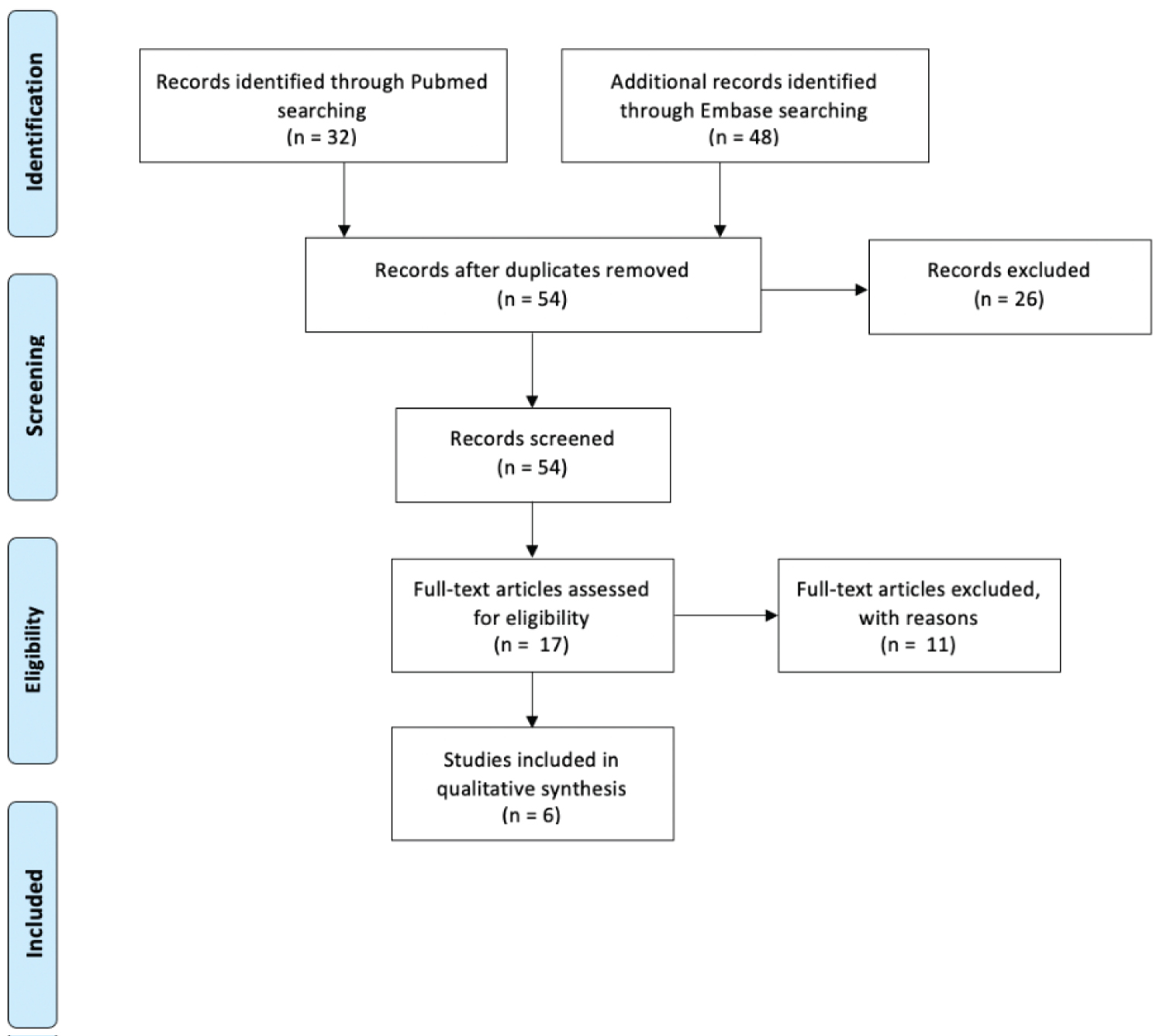
Two of the authors in this study performed above search independently. Six papers met inclusion criteria for review after abstract and full text screening. There were no disagreements on whether a paper met inclusion criteria. The six papers that met inclusion criteria after full-text review were included for data analysis (Figure 1).
Search process
The search process was conducted according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for conducting a systematic review (Figure 1). Eighty articles were identified using the search query outlined above. Among these, 26 duplicate articles were identified and removed. The remaining 54 abstracts were screened using the predetermined inclusion and exclusion criteria. In ten cases, the full text was reviewed to confirm exclusion status due to ambiguity in the abstract concerning analysis of outcomes after revision THA for infection. These papers were ultimately excluded because the cohort of patients who underwent revision THA for infection was not analyzed separately from patients who underwent revision THA for non-septic indications (aseptic loosening, recurrent dislocation, fracture, etc.). This process yielded seven eligible studies [12,15,24-28]. One additional study was excluded from the systematic review due to uncertain loss to follow-up and limited outcomes analysis [25].
Overall, abstract and full-text review yielded six studies for data analysis [12,13,15,24,26,28]. Five of the six studies were retrospective single-institution studies including a consecutive series of patients who under went revision THA for chronic periprosthetic joint infection (PJI). One study followed patients prospectively after two-stage revision for a minimum follow-up period of at least two years [24]. Four studies only included patients who underwent ETO, and two studies included comparison groups including patients who did not undergo ETO or under went ETO for indications other than revision [12,28]. All studies limited their analysis to outcomes after two-stage revision THA for chronic periprosthetic infection among patients with a minimum 2-year follow-up.
Four of the six studies reported clinical outcomes scores including pre- and postoperative Harris Hip Scores (HHS) [12,24,26,28]. Preoperative and postoperative radiographic evaluation was performed in all studies. Four studies analyzed postoperative X-rays at three, six, twelve weeks and annually following surgery [12,15,24,26]. Femoral defects were classified according to the Paprosky classification system using radiographs taken before reimplantation surgery in three studies [13,15,24,29].
Surgical information
The indication for ETO in all cases was revision THA for chronic PJI. Two studies diagnosed PJI using the criteria established by Zimmerli, et al. which requires that one of the following criteria to be met: Bacterial growth in two or more cultures, purulence of synovial fluid at the implant site, histopathology showing acute inflammation, or presence of a sinus tract at the prosthetic site [12,28,30]. Another study defined PJI as the presence of two of the following factors: Bacterial growth on two or more culture specimens, histopathology showing an average of greater than ten polymorphonuclear cells in the five most cellular fields, or grossly infected appearing tissue at revision [15]. In one study, presence of PJI was confirmed preoperatively using hip aspiration [24]. Morshed, et al. and Petrie, et al. did not comment on the definition of PJI used [13,26].
Stage one revision surgery included ETO, removal of the primary prosthesis, irrigation and debridement, and implantation of an antibiotic spacer. All patients received organism-specific intravenous antibiotics following stage one revision. The most common infective organism(s) identified from cultures taken in stage one surgery are summarized in Table 1. Three studies noted repeat I&D in three of 147 cases (2.0%) where clinical and lab values did not normalize after first stage [15,24,28].
Second stage followed standard protocols including lab markers to confirm infection clearance, cultures, and at times frozen sections taken at reimplantation. Second stage reimplantation included removal of the spacer and revision prosthesis implantation with ETO fixation. Average time from first to second stage revision THA ranged from 8.9 weeks [26] to 46.5 weeks [28] with a weighted average of 24 weeks. Intraoperative cultures and frozen pathology sections were obtained during stage two surgery to confirm infection clearance in five studies [12,15,24,26,28]. In three of the studies, it was noted that 96 out of 147 (65%) patients required re-opening of the osteotomy (Table 2). This was not commented on in other studies.
All ETOs were performed using a traditional posterior approach (Table 2), with no reports of anterior or lateral based approaches [12,13,15,26,28]. The studies reported a mean osteotomy length of 15.7 cm (range, 8 to 30.9 cm) and five of six reported use of cerclage wires or cables for ETO reconstruction/closure during the first stage. The protocol for reopening the osteotomy site in stage two of revision varied, with some authors reopening the osteotomy site routinely and others only on occasion or none (Table 2).
Implant type
Five studies reported on primary femoral stem fixation and included 89 cemented primary stems (49%) and 94 cementless primary stems (51%) [12,15,24,26,28]. The type of antibiotic spacer used in stage one revision surgery varied. Overall, the majority of cases received either an articulating or static antibiotic-coated cement spacer (62%). The remaining patients received cement antibiotic beads without a spacer (35%) or had a reimplantation of the original prosthesis coated in antibiotic-loaded cement (3%) [14,15].
Most patients received a cementless revision femoral stem in second stage revision surgery 69%, (Table 2). Eighty-five of 87 cemented revision stems were implanted in one study [15]. Four studies assessing a total of 160 patients used cementless femoral stems in all cases for a total of 160 cementless stems [12,24,26,28]. The types of femoral stems utilized are summarized in Table 2.
Results
Demographics
In total, the six studies reported on a total of 285 ETOs performed during revision THA for periprosthetic joint infection. Two studies also included comparison groups including a total of 87 revision THAs either without ETO or with ETO for non-infection indications (Table 3). The ETO for PJI cohort included 140 males (50%) and 142 females (50%) with an average age of 64.9 years (range, 52.6 to 70.7 years). Average reported body mass index was 27.5 kg/m2 [12,28]. Reported femoral defects according to the Paprosky classification system before reimplantation included 63 Type 1 (32%), 64 Type 2 (33%), 46 Type 3A (23%), 12 type 3B (6%), and 7 type 4 defects (4%) [13,15,24]. The weighted mean follow-up time across ETO groups was 60.4 months (range, 39 to 72.4 months). These findings are summarized in Table 3.
Radiographic outcomes
ETO union rates were consistently high, ranging from 87% [13] to 100% [12,26] with acumulative average of 94%. The average time to union was reported in four studies and ranged from 10.6 weeks [12] to 15.6 weeks [26] with an average of 12.0 weeks (Table 4). There was no difference in the time to union or union rate between patients who required osteotomy reopening in second stage surgery and patients who did not [15,28].
Femoral component stability was 94.0% (156 out of 166 components). The rate of > 5 mm stem subsidence was 6.0% (10 out of 166), although seven of these patients were ultimately asymptomatic and did not require re-operation for stem subsidence, likely due to stable fibrous in growth [12,15,24,28]. Separately from stem subsidence, 1.1% of stems were reported aseptically loose and required revision [17,28]. Summary of these findings are listed in Table 4. Additionally, Petrie, et al. reported four cases of heterotopic ossification (4%) and nine cases of trochanteric avulsion (9%) [13].
Infection recurrence
Infection recurrence and reinfection-free success rates are summarized in Table 4. Overall, recurrent infection occurred in 17 of 285 cases (6.0%).
Perioperative and postoperative complications
Perioperative and postoperative complication rates are summarized in Table 4. The average incidences of intraoperative and postoperative fracture were 12.6% and 4.4%, respectively (Table 4). Postoperative dislocation occurred in 7.0% of cases. The revision rate with minimum 2-year follow-up after second stage reimplantation was 7.0% (20 of 285 cases). Implant revision diagnoses included postoperative periprosthetic fracture (6 cases), recurrent infection (6 cases), dislocation (4 cases), femoral stem subsidence (3 case), and aseptic loosening of acetabular component (1 case).
Clinical outcomes
Preoperative and postoperative HHS was reported in four studies (Table 5). In addition to HHS, Levine, et al. reported a significant change in D'Aubigne and Postel hip scores from an average of 5.3 (range, 2-10) preoperatively to an average of 10.0 (range, 7-12) at final follow-up [15].
Discussion
The purpose of this study was to compile and characterize patient demographics, complications, and clinical outcomes following ETO in the treatment of infected THA. This review of current literature suggests that ETO in the setting of revision THA for PJI provides high rates of infection eradication, high rates of ETO union, and similar outcomes between patients who underwent ETOs for septic versus aseptic revision THA.
In the setting of chronic periprosthetic joint infection, removal of a well-fixed femoral component is necessitated and can be technically challenging due to modern fixation techniques and component designs. ETO is a powerful technique that can facilitate removal of fully porous stems, well fixed proximally coated stems, long cement mantles, or varus/valgus remodeling [5,8,11]. Importantly, ETO minimizes the risk of intraoperative fracture and promotes predictable healing of the abductor on the osteotomized fragment [8,15,26,31].
Multiple studies have reported favorable outcomes after revision THA with high union rates and minimal postoperative complications in patients undergoing ETOs [31-33]. In a recent systematic review published by Malahias, et al. ETO for the revision of aseptic THA demonstrated excellent outcomes across nineteen papers including an overall ETO union rate of 93%, complication rate of 8.1%, and re-revision rate of 5.7% [14]. These excellent outcomes led the authors to recommend ETO in single-stage revision THA cases requiring stem reimplantation where stem or cement removal is associated with high risk of intraoperative fracture [33].
Importantly, nearly half of the cases reviewed in this study involved the revision of cemented primary stems (49%), with the remaining 51% involving cementless primary stems. The majority of patients were revised to a cementless stem (69%), including modular and diaphyseal-engaging stems. The majority of cemented stems (85 out of 87 stems) were implanted by Petrie, et al. to investigate the impact of stem type on outcomes after ETO. Excluding the study by Petrie, et al. 181 out of 183 revision stems (99%) were cement less. These findings provide support for the use of either cementless or cemented stems following ETO for PJI, although the optimal reimplant stem type has yet to be identified.
Fixation of the osteotomy fragment during second stage revision surgery was performed with multiple cerclage wires or cables in all cases. A range of fixation technique for ETO in revision hip arthroplasty has been studied. Huffman, et al. found that combined vertical and horizontal cable fixation of ETO resulted in 100% osteotomy healing and excellent implant stability [22]. MacDonald, et al. found that using a lateral approach for ETO, fixation using cerclage wires was associated with significantly more proximal migration of the osteotomized fragment than fixation with cables [34]. Biomechanical studies have demonstrated increased stability and decreased incidence of nonunion using cable fixation compared to wire fixation [35,36]. However, Morshed, et al. also demonstrated that delayed fixation at stage two can yield high union rates and femoral stability, suggesting that fixation with wires/cables may not be needed at stage one. The authors of this systematic review prefer to use smooth wire fixation of the ETO site during stage one revision to avoid the use of braided cables in the setting of active infection and exchange the wires for the more robust cables at the second stage. The papers reviewed in this study suggest that cerclage wires and cables either at stage one or two are effective in fixation of ETO after periprosthetic joint infection, although there is no consensuson the timing or method of ETO fixation in current literature.
Eradication of infection at intermediate follow-up was achieved in 94% of cases in this review (268 of 285 cases). While four studies reported the infective organism(s) identified before stage one revision surgery (Table 1), no studies discussed the impact of organism type on ETO healing and treatment outcomes [12,15,24,28]. Future studies should assess the impact of organism type on outcomes after revision THA for PJI. Two studies did include comparison groups: 1) ETO for PJI compared to ETO for non-PJI revision THAs, and 2) ETO for PJI compared to non-ETO for PJI revision THAs [12,28]. There was no significant difference in outcomes measurements between the groups who underwent ETO for infected and non-infected hip arthroplasties [12]. This suggests that the outcomes after ETO for infection are comparable to those after non-septic revision. Similarly, there was no difference in postoperative HHS, femoral component stability, or femoral component subsidence between patients who underwent ETO for PJI and those who did not undergo ETO. Patients in the ETO group had a significantly lower risk of repeated debridement. The authors hypothesized that this may be because ETO provides excellent visualization of the femoral canal which allows for a more complete and thorough intraoperative debridement [28].
There are several limitations to the studies included in this analysis. Due to the selection process and retrospective nature of this review, there is potential for publication bias, selection bias, and potential loss to follow-up in the studies. Furthermore, the studies were all retrospective, with only one study following patients prospectively after surgery. Four of the six studies were level IV retrospective reviews, and two of the six studies were level III retrospective cohort studies. Not all studies identified the same peri-operative variables, patient demographics, infective organism, or surgical technique, resulting in a heterogenous pool for assessment and most without a controlled cohort to compare to. Of the level III studies, only one compared outcomes after ETO between patients undergoing revision of septic versus non-septic THA [12]. The other level III study compared outcomes of patients who underwent revision THA for PJI with and without ETO as discussed above [28]. Additionally, the type of primary and revision implants as well as fixation technique varied between studies. The studies included in this review only reported posterior approaches, but ETOs or equivalent osteotomies can also be performed via anterior or anterolateral approaches. Future studies should explore the impact of implant type, fixation method, and surgical approach on the outcomes after ETO for revision of infected THA. Despite these variations, ETO healing rates, complication rates, and patient outcomes remained consistent across studies. This systematic review provides a valuable summary of existing literature regarding the utilization of ETOs in managing PJIs in THA.
Conclusions
In conclusion, current literature provides evidence that the use of ETOs in revision THA for chronic periprosthetic joint infection is safe and effective. Existing data suggest high rates of infection eradication, high rates of ETO unionand similar outcomes between patients who underwent ETOs for septic versus aseptic THA revisions diagnoses. Total joint specialists should consider the use of ETOs when managing infected THAs, especially when retained stems cannot be safely extracted.
Funding Sources
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Kurtz S, Ong K, Lau E, et al. (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am 89: 780-785.
- Gwam CU, Mistry JB, Mohamed NS, et al. (2017) Current epidemiology of revision total hip arthroplasty in the United States: National inpatient sample 2009 to 2013. J Arthroplasty 32: 2088-2092.
- Prudhon JL, Tardy N (2018) Extended trochanteric osteotomy: Comparison of 3 modes of fixation: Metallic wires, cables, plate, about a series of 157 cases. SICOT J 4: 21.
- Pabinger C, Lothaller H, Portner N, et al. (2018) Projections of hip arthroplasty in OECD countries up to 2050. Hip Int 28: 498-506.
- Brown JM, Mistry JB, Cherian JJ, et al. (2016) Femoral component revision of total hip arthroplasty. Orthopedics 39: e1129-e1139.
- Zhan C, Kaczmarek R, Berrios NL, et al. (2007) Incidence and short-term outcomes of primary and revision hip replacement in the United States. J Bone Joint Surg Am 89: 526-533.
- Mahomed NN, Jane A Barrett, Katz JN, et al. (2003) Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am 85: 27-32.
- Sambandam SN, Duraisamy G, Chandrasekharan J, et al. (2016) Extended trochanteric osteotomy: Current concepts review. Eur J Orthop Surg Traumatol 26: 231-245.
- Younger TI, Bradford MS, Magnus RE, et al. (1995) Extended proximal femoral osteotomy. A new technique for femoral revision arthroplasty. J Arthroplasty 10: 329-338.
- McGrory BJ, Bal BS, Harris WH (1996) Trochanteric osteotomy for total hip arthroplasty: Six variations and indications for their use. J Am Acad Orthop Surg 4: 258-267.
- Sundaram K, Siddiqi A, Kamath AF, et al. (2020) Trochanteric osteotomy in revision total hip arthroplasty. EFORT Open Rev 5: 477-485.
- Lim SJ, Moon YW, Park YS (2011) Is extended trochanteric osteotomy safe for use in 2-stage revision of periprosthetic hip infection? J Arthroplasty 26: 1067-1071.
- Petrie MJ, Harrison TP, Buckley SC, et al. (2017) Stay short or go long? can a standard cemented femoral prosthesis be used at second-stage total hip arthroplasty revision for infection following an extended trochanteric osteotomy? J Arthroplasty 32: 2226-2230.
- Wronka KS, Wilson MG, Peel E, et al. (2020) Extended trochanteric osteotomy: Improving the access and reducing the risk in revision THA. EFORT Open Rev 5: 104-112.
- Levine BR, Valle CJD, Hamming M, et al. (2009) Use of the extended trochanteric osteotomy in treating prosthetic hip infection. J Arthroplasty 24: 49-55.
- Ladurner A, Zdravkovic V, Grob K (2018) Femoral bone restoration patterns in revision total hip arthroplasty using distally fixed modular tapered titanium stems and an extended trochanteric osteotomy approach. J Arthroplasty 33: 2210-2217.
- Rieger B, Ilchmann T, Bolliger L, et al. (2018) Mid-term results of revision total hip arthroplasty with an uncemented modular femoral component. Hip Int 28: 84-89.
- Lim CT, Amanatullah DF, Huddleston JI, et al. (2017) Use of cortical strut allograft after extended trochanteric osteotomy in revision total hip arthroplasty. J Arthroplasty 32: 1599-1605.
- Smith MA, Deakin AH, Allen D, et al. (2016) Midterm outcomes of revision total hip arthroplasty using a modular revision hip system. J Arthroplasty 31: 446-450.
- Baktır A, Karaaslan F, Gencer K, et al. (2015) Femoral revision using the wagner sl revision stem: A single-surgeon experience featuring 11-19 years of follow-up. J Arthroplasty 30: 827-834.
- Lakstein D, Kosashvili Y, Backstein D, et al. (2010) Modified extended trochanteric osteotomy with preservation of posterior structures. Hip Int 20: 102-108.
- Huffman GR, Ries MD (2003) Combined vertical and horizontal cable fixation of an extended trochanteric osteotomy site. J Bone Joint Surg Am 85: 273-277.
- Miner TM, Momberger NG, Chong D, et al. (2001) The extended trochanteric osteotomy in revision hip arthroplasty: A critical review of 166 cases at mean 3-year, 9-month follow-up. J Arthroplasty 16: 188-194.
- Fink B, Oremek D (2016) The transfemoral approach for removal of well-fixed femoral stems in 2-stage septic hip revision. J Arthroplasty 31: 1065-1071.
- Jones CW, Selemon N, Nocon A, et al. (2019) The influence of spacer design on the rate of complications in two-stage revision hip arthroplasty. J Arthroplasty 34: 1201-1206.
- Morshed S, Huffman GR, Ries MD (2005) Extended trochanteric osteotomy for 2-stage revision of infected total hip arthroplasty. J Arthroplasty 20: 294-301.
- Petrie J, Haidukewych GJ, Liporace FA, et al. (2018) Practical surgical techniques for revision total hip arthroplasty. Instr Course Lect 67: 191-205.
- Shi X, Zhou Z, Shen B, et al. (2019) The use of extended trochanteric osteotomy in 2-stage reconstruction of the hip for infection. J Arthroplasty 34: 1470-1475.
- Paprosky WG, Perona PG, Lawrence JM (1994) Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty 9: 33-44.
- Zimmerli W, Trampuz A, Ochsner PE, (2004) Prosthetic-joint infections. N Engl J Med 351: 1645-1654.
- Paprosky WG, Martin EL (2003) Cemented stem failure requires extended trochanteric osteotomy. Orthopedics 26: 28, 38.
- León SA, Xin Mei Y, Ethan Sanders B, et al. (2019) Does trochanteric osteotomy length affect the amount of proximal trochanteric migration during revision total hip arthroplasty? T Arthroplasty 34: 2718-2723.
- Malahias MA, Gkiatas I, Selemon NA, et al. (2020) Outcomes and risk factors of extended trochanteric osteotomy in aseptic revision total hip arthroplasty: A systematic review. J Arthroplasty 35: 3410-3416.
- MacDonald SJ, Cole C, Guerin J, et al. (2003) Extended trochanteric osteotomy via the direct lateral approach in revision hip arthroplasty. Clin Orthop Relat Res 417: 210-216.
- Zhu Z, Ding H, Shao H, et al. (2013) An in-vitro biomechanical study of different fixation techniques for the extended trochanteric osteotomy in revision THA. J Orthop Surg Res 8: 7.
- Barrack RL, Butler RA (2005) Current status of trochanteric reattachment in complex total hip arthroplasty. Clin Orthop Relat Res 441: 237-242.
Corresponding Author
Jeffrey Barry, MD, Department of Orthopaedic Surgery, University of California, San Francisco, 500 Parnassus Ave, MU-323W, San Francisco, CA 94143, USA
Copyright
© 2021 Salesky M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.