Dementia Research Activity in Sri Lanka: A Review
Abstract
Background
As a result of the global rise in life expectancy, dementia has become a major global health concern; it is considered to be one of the most burdensome conditions of later life. Despite 66% of older adults with dementia living in Low-and-Middle Income countries (LMIC), only 10% of dementia research has been conducted in these countries and more information is needed about research activity within LMIC to inform on global dementia research strategies. To-date no systematic reviews have been carried out to explore existing evidence of dementia research reported from Sri Lanka, despite it having the fastest ageing population in the region.
Objective
To describe dementia research activity conducted in Sri Lanka.
Method
Systematic searches of databases (MEDLINE, EMBASE, PsycINFO, AMED, CINAHL, SLJOL, Cochrane Library) and grey literature were conducted from each database inception to April 2020. Pre-defined inclusion and exclusion criteria were applied and papers were screened and quality assessed. Research activity by individual studies were mapped into four research domains. A narrative synthesis was conducted to describe dementia research activity.
Findings and conclusions
Out of 971 papers retrieved from searches, 28 studies were included in the review. Results show evidence across four research domains; epidemiology (n = 6), pathophysiology (n = 4), screening for dementia (n = 13), and dementia management (n = 7). In comparison to the International Consortium for Health Outcome Measurement (ICHOM) standard set for dementia, this review found a lack of dementia research activity in Sri Lanka generally, as well as a lack of high-quality research, particularly in the areas of dementia prevalence, dementia care, characteristics of formal and informal caregivers, and service provision for people with dementia and their and families. There is a need for more high-quality research, with robust methodologies, which would inform policy and service provision in Sri Lanka for people with dementia.
Keywords
Dementia, Research activity, Sri Lanka, Review
Background and Introduction
As a result of the global rise in life expectancy, dementia has become a major global health concern; it is considered to be one of the most burdensome conditions of later life and many older adults will experience and live with dementia in the future [1-4]. Out of the diseases labelled as a global burden, dementia contributes to 11.2% of disability in people aged 60 and older [5], more so than many other common conditions, including stroke, musculoskeletal disorders, cardiovascular diseases, and cancer. Whilst the number of older adults with dementia across regions and countries show a clear increase over time, differences in prevalence rates have been reported across regions [6,7]. A Delphi consensus study among international dementia experts reported that 60% of people with dementia were living in Low-and-Middle Income countries (LMIC), and will rise up to 71% by 2040 [8] . Importantly there is a disparity in the projected rates of dementia by relative income per country [7-10]; for example, numbers in High-Income countries (HIC) are forecast to increase by 100% between 2001 and 2040, but by more than 300% in South Asian and Western Pacific region [8]. Furthermore, the Alzheimer's Disease International (ADI) report on dementia in the Asia Pacific region shows that countries in this region have a growing dementia burden [11], and it is projected that Asia will be the region with highest number of people living with dementia worldwide [12].
Despite these projections, the evidence base within Asia, more so South and Southeast Asia [12,13], show an imbalance in term of research, with 66% of older adults with dementia living in LMIC [14] but only 10% of dementia research having been carried out in LMIC [15]. It is timely to review dementia research activity within LMIC, and this review particularly focuses on Sri Lanka as it is estimated by the World Bank Report (2008) that in the coming years Sri Lanka will experience the fastest ageing population among South Asian countries [8]. Furthermore, whilst many systematic reviews on dementia have been carried out previously in HIC on aspects including prevalence, awareness, dementia management, patient and caregiver characteristics, effectiveness of interventions, factors associated with caregiver burden and the challenges of dementia care [6,16-20] , none has been carried out to explore dementia research activity in Sri Lanka. In addressing this gap, this paper reports on a systematic review aiming to describe dementia research activity in Sri Lanka.
Methods
Protocol development
The protocol was developed based on the Population, Intervention, Comparison, Outcomes of interest, Setting and study design (PICOS) format and the protocol and search strategy are registered in the Prospero International Prospective Register of systematic reviews (Reg No: CRD42017052071).
Inclusion criteria
The review included all the papers published at present regardless of study design, publication status and the date of publication. The following criteria based on the PICOS format was used when assessing eligibility:
• All types of research studies (e.g. full papers, editorials, reviews, commentaries, opinion pieces) conducted in Sri Lanka were included if they had a focus on any aspect of dementia.
• Studies whose subject were older adults with dementia (i.e., age 60 years or above), and formal or informal caregivers who are involved in care provision for people with dementia.
• Evidence relating to cognitive impairment were also included. Whilst this differs from dementia, these studies were considered relevant as in many cases minor cognitive impairment may later progress to dementia.
Exclusion criteria
Papers on any other memory problem distinct from dementia (for example early-onset dementia, delirium, memory loss due to traumatic events or amnesia) were excluded.
Search strategy and search terms
The search strategy aimed to find both published and unpublished studies. A combination of specific keywords consisted of search terms and Boolean operators; for example, (dement* OR neurocognitive disorder* OR alzheimer* OR 'lewy bod*' OR 'vascular cognitive impair*' OR 'cognitive impairment') AND ('Sri Lanka*' OR Colombo OR Ceylon). The search was carried out by using NHS Open Athens interface, the Cochrane Central Register of Systematic Reviews and Controlled Trials. The online databases searched were: Medline, CINAHL, PsycINFO, EMBASE and AMED. In order to obtain relevant locally published articles within the context, Sri Lanka Journals Online (SLJOL), a database for online published journals in Sri Lanka (www.sljol.info/) was also searched. A grey literature search was also carried out manually from the Post Graduate Institute of Medicine (PGIM) library, Sri Lanka (the submitted theses and dissertations for PhD, MD and MSc up to the last search date). PhD theses, MD and MSc dissertations submitted to PGIM were also searched manually using the library catalogue to find any related information in the unpublished dementia studies. Papers of on-going research, conference proceedings and theses were also hand searched for unpublished research findings. Reference lists of included papers and relevant journal or book reviews were searched by hand, and authors of included papers were contacted where possible, to request full papers which were not available online and to ask if they knew of other relevant studies. We conducted the initial search between September to October 2016 and a top-up search was conducted in April 2020.
Study selection
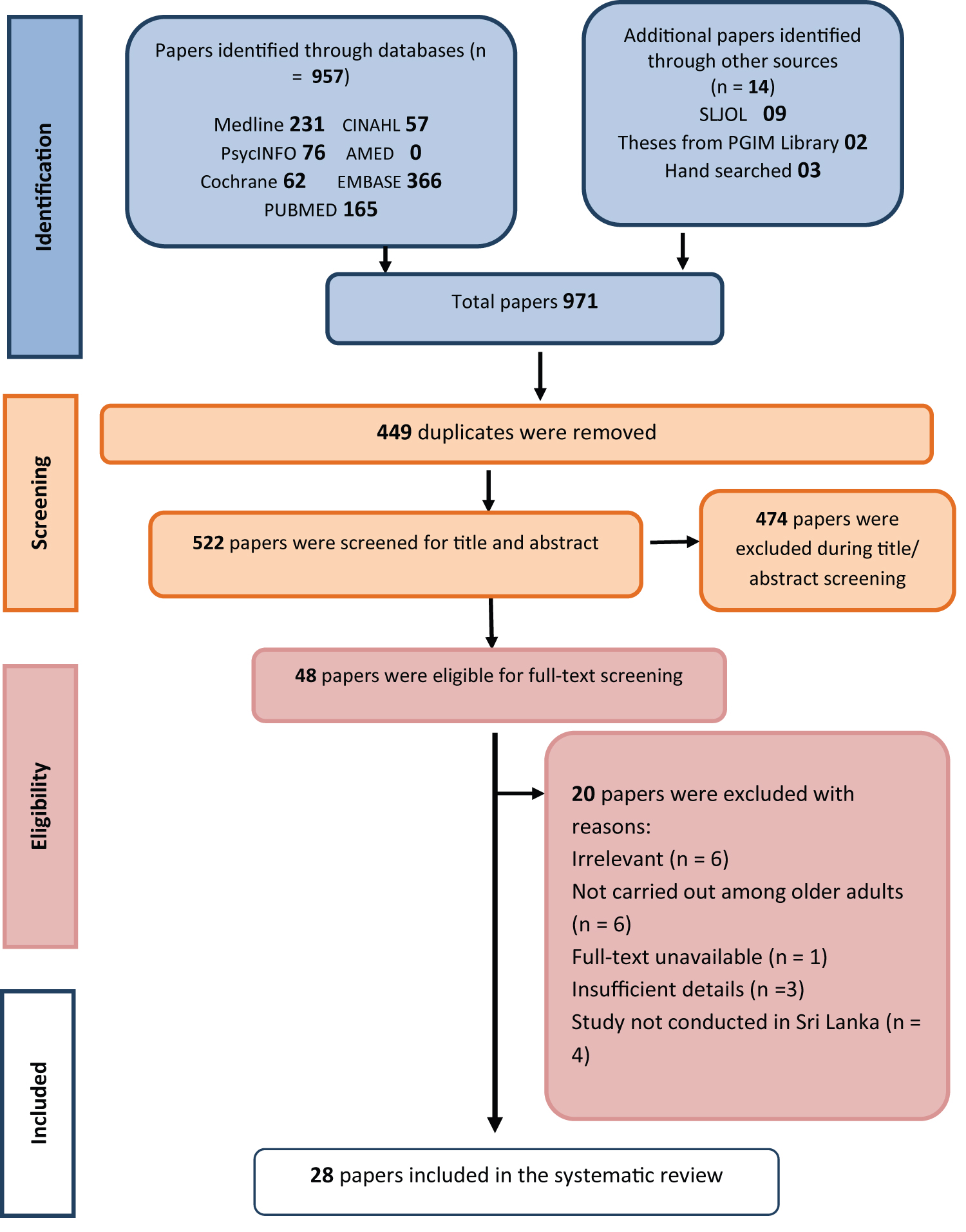
Inclusion of papers involved several selection stages following steps outlined by Boland, Cherry and Dickson [21]. The first step of title, abstract and full-text screening was to remove duplicates. The 'Exact Match' (i.e., the similar papers with the same title, abstract and full-text included in different databases) and then 'Close Match' articles (i.e., same paper with minor differences in how a reference is indexed in different databases) on the search results were removed. After that, the lists of references were reviewed in order to find additional relevant papers. Papers were excluded if they showed no relation to the inclusion criteria based on the title and abstract. Porritt, et al. recommend two reviewers select papers in order to ensure transparency and reproducibility of the study selection process [22]. Accordingly, the first round of searches was conducted independently by two reviewers (KA) and (AS). Both agreed on the inclusion of papers if the relevant information was provided in the title or abstract. In cases where it was unclear from the title or abstract whether a paper was relevant, the full texts were also screened. The number of papers remaining after each stage was recorded. This process is illustrated in Figure 1: PRISMA criteria for paper selection.
Quality appraisal of included studies
Risk of bias assessment for each included study is recommended in systematic reviews in order to evaluate rigour and relevancy of the papers and to establish transparency of the review results [21]. Two authors (KA and LD) assessed full-text papers and performed critical appraisal for evidence using a quality assessment tool (i.e., the Joanna Briggs Institute (JBI) critical appraisal tools - http://joannabriggs.org/research/critical-appraisal-tools.html) to rate the sources of potential bias in each study. JBI critical appraisal tools are a set of checklists (thirteen) or standardised assessment tools for variety of study designs. The JBI critical appraisal tools were chosen as they cover the full range of study designs included in the current review (for example; qualitative studies, case reports, case studies, cohort studies, diagnose test accuracy, mixed-method studies, validation studies, text and opinion papers). Quality assessment was carried out independently by KA and LD; sub-samples were cross-checked with AS for consistency and any disagreement about the papers was resolved.
Each paper included was rated based on the study purpose, study design, sample size, response rate, method of data analysis, the validity of the results and reporting of the findings. A scale (of 0-10) was used to rate the overall quality of the paper including risk of bias and strength of evidence drawn from each study. Consequently, review items were judged and rated to be of either high quality (total score 7-10), moderate quality (total score 4-6), or low quality (total score 0-3). Papers that met the inclusion criteria and contained information regarding dementia research activity in Sri Lanka were included in the review, none were excluded based on their quality (for example, opinion pieces). The quality ratings were used to develop a greater understanding of the papers and their results, and as a measure of credibility of the findings presented [21].
Data extraction
The data extraction was performed by KA, and all papers were cross-checked by the second reviewer (LD); a third reviewer (AS) resolved any disagreements. The following information was extracted from the papers:
• Paper title, authors, year of publication
• Aim and objectives of the study (not applicable for commentary or opinion pieces)
• Methodological characteristics of the study (e.g. study design, study setting, inclusion/exclusion criteria, recruitment procedures used, sample size, response rate), type of analyses methods used (for example qualitative, quantitative, mixed-methods or case study)
• Data collection tools used in the study
• Descriptors of the intervention (if an intervention was used)
• Dementia severity and diagnostic details (dementia type, information about non-responders)
• Demographic information including incidence rate and prevalence rate of dementia
• Caregiver burden measures, risk factors for caregiver burden (patient characteristics, caregiver characteristics)
• Details of relevant outcome measures and summary outcome data (results, conclusions, recommendations, limitations of the study and personal notes and remarks (e.g. limitations of the study)
Narrative Synthesis
Aligned to the aims of the review, a descriptive narrative analysis was carried out, this was appropriate due to the expected heterogeneity of study designs, sample sizes, study aims, interventions and reported outcomes. The initial step of the narrative synthesis was to cluster and map the papers into domains. Each study was assigned to one or more domains, namely: Epidemiology, pathophysiology, screening for dementia (e.g. instrument validation and screening process), and management of dementia (e.g. treatment, caregiving and care models). Mapped papers were tabulated based on their domain and compared within and across studies. The 'narrative synthesis' approach allowed the identification of evidence reported in the reviewed papers to draw informative conclusions relevant to the review objectives.
Results
Based on the initial searches, 971 papers were retrieved (up to April 2020). Among these, 449 duplicates were removed. Out of the remaining 522 papers, 474 were excluded based on title and abstract screening, as they did not match the screening criteria (see Figure 1). Forty-eight papers were eligible for full-text screening; among them, 20 were excluded for the following reasons: irrelevant full-texts (not related to older adults or dementia), studies were not conducted in Sri Lanka, or full paper not available. Twenty-eight papers were included in the narrative synthesis. Among the selected papers there were 20 journal articles (full papers), three opinion papers for journals, three conference abstracts and two MD theses. Where appropriate, we contacted the study authors for further information; three papers which were not available online were received from the authors upon request.
Mapping the dementia research conducted in Sri Lanka
Research reported in the included papers represented evidence across four key domains. These domains were generated from the extracted evidence. Some papers reported information on more than one domain. Figure 2 illustrates the number of papers categorised within each domain. Table 1 summarises the papers and grey literature included in the review [23-50].
Domain 1: Epidemiology
Six papers reported on prevalence (see Table 2). No island-wide prevalence studies were found in this systematic review. De Silva, et al. reported the first prevalence study with an overall prevalence rate of 3.98% of people with dementia in the Ragama area (95% CI = 2.6% - 5.7%) [23]. Among them 20 (71.4%) had probable Alzheimer's disease (AD), four (14.3%) had Vascular dementia (VD), two (7.1%) had mixed dementia (AD and VD) and one person had Lewy body's dementia. One participant was diagnosed as having dementia due to syphilis. Advanced age, female gender and illiteracy were associated with a higher prevalence of dementia among the study group of older adults aged 65 and over (n = 703) [23]. Another brief report on a study among a group of older adults (n = 50) aged 60-85 reported that 66% demonstrated mild to severe cognitive deficits and 44% of older people demonstrated moderate to severe cognitive deficits according to the Mini Mental State Examination (MMSE) [48]. However, this brief report does not include any information on dementia diagnosis.
Dahanayake, et al. reported that, amongst a sample of 122 patients diagnosed with dementia in Colombo (mean age 71.3%, the mean duration of cognitive impairment was 2.9 years), 32.8% had mild dementia, 42.6% had moderate dementia and 24.6% severe dementia [43]. The majority of them presented with behavioural and psychological symptoms of dementia (BPSD) including delusions (42.6%), irritability (41%), appetite changes (34.4%) and depression (32%). Depression and anxiety symptoms were common among people with mild dementia (p < 0.05) in the study sample [43].
Rajakumaraswamy, Rajapakse and Fernando reported a high rate of cognitive impairment (32.8%) and dementia prevalence (11.8%) among an elderly population (n = 204) with type two Diabetes in Sri Lanka [47]. A study conducted among a group of older adults who attended clinics in the National Hospital in Sri Lanka revealed a high prevalence (50%) of cognitive impairment; however, there was no association found between the severity of cognitive impairment and the older adults' education le vel or social support [49].
Unpublished data from an MD thesis on prevalence of mild cognitive impairment (MCI) and selected correlates among older people in the Jaffna district reported a relatively high prevalence of MCI (20.9% with 95% CI = 18.4 -23.4) [38] (Table 3).
Domain 2: Pathophysiology
Only four papers [29-31,38] reported the pathophysiology of dementia; one low-quality opinion paper, one moderate quality journal article, one moderate quality conference proceeding from the same study and one moderate quality thesis. De Silva, et al. first reported that high mean plasma homocysteine (tHcy) levels, presence of apoE4 allele and MTL atrophy are associated with a study population of people with Alzheimer's disease in Sri Lanka (n = 23 patients with AD and 21 control) [29]. The study found a significant increase in mean plasma tHcy levels (p = 0.001) and frequency of apoE4 genotype (p = 0.003) among people with AD. Wijesinghe, et al. conducted the first autopsy study to investigate genetic polymorphisms using 76 post-mortem brain samples of older adults in Sri Lanka and India [30]. Findings indicated that ageing cytoskeletal pathologies are higher in older adults in Sri Lanka when compared to Indian older adults; illiteracy and genes (e.g. apoE4 and thal β-amyloid phase) were significantly associated in determining the aetiology of AD [30]. Wijesinghe, et al. reported that genetic, dietary and/or environmental variations are associated with ageing cytoskeletal pathologies among older adults in Sri Lanka [31].
Coonghe reports socio-demographic factors (such as age > 75, education of less than 10 years, unstable income) and habitual risk factors (such as beetle chewing, night-time sleep less than seven hours, vegetarian diet and lack of socialisation) were found to be the correlating factors for MCI. Even though MCI is different from dementia these findings are important as the MCI can progress to dementia [38].
Domain 3: Screening for dementia
Screening older adults for dementia and cognitive impairment: According to Samaraweera most of the general elders' clinics in Sri Lanka had missed detecting cognitive impairment and dementia among elderly patients due to time constraints and lack of emphasis on the systematic evaluation of older adults [50]. Author also highlights a need for using specific screening tools in general clinics to detect geriatric psychological problems among older adults. Further to this, in his thesis, Coonghe (2015) reports diagnosis by the consultant neurologist is the gold standard for diagnosis of MCI and AD [38].
Screening tools used in the studies: As reported from the evidence within the review, the MMSE is the most common screening tool used to detect cognitive impairment in older adults. This tool has been translated and validated for both Sinhalese [32,33,48] and Tamil languages [38,47]. Clinical diagnosis of participants in the included studies is mostly based on DSM IV, ICD 10 and NINCDS-ADRDA criteria which included structured neuropsychiatric assessment using the Cambridge examination for mental disorders of the elderly (CAMDEX), Cambridge Cognitive Score (CAMCOG), Montreal Cognitive Assessment (MoCA), Neuropsychiatric Inventory (NPI) [23,43], Clinical Dementia Rating (CDR) scale [36], laboratory investigations and axial CT scan of the brain and participant interviews [23]. Findings of the review also indicate that biochemical screening and neuro-imaging tests such as a computerised tomography (CT) scan and magnetic resonance imaging (MRI) scan are used for the detection of dementia types and to exclude other causes [42].
Translating and validating of instruments for Dementia Screening: The majority of the studies included in this review were instrument validations. There were eight studies on translating and validating of dementia screening tools [1,34,35,37,38,42].
The MMSE is the first Sinhalese translated and validated screening tool with culturally appropriate modifications of the content. Sensitivity and specificity of the translated MMSE was reported as 93.5% and 84.6%, respectively (with cut off value of 17) [23,32] The authors reported that the translated version is a useful and sensitive instrument to screen for cognitive impairment in Sri Lanka. A Tamil translation and criterion validity of MMSE has been assessed by Coonghe; the area under the ROC was 0.85 (95% CI 0.80 - 0.89) [38].
Karunaratne, Hanwella and De Silva translated the MoCA into Sinhalese for the first time. Validation of the MoCA reported a sensitivity of 100% and specificity of 87% in detecting mild Alzheimer's disease at a cut-off of 26 with a sensitivity of 90% in detecting MCI [35]. A Tamil translation and criterion validity of MoCA has been assessed by Coonghe for MCI (mean score = 21.16; SD ± 2.55) and AD (mean score = 14.05; SD ± 3.81); there was also a high correlation between MoCA and MMSE Tamil versions (0.853). The area under the ROC was 0.87 (95% CI 0.83 - 0.91) [38].
Kathriarachchi, et al. compared the use of the Sinhalese version of MMSE, Informant Questionnaire on Cognitive Decline (IQCODE) and CDR scales, and found these to be sensitive and culturally adapted screening tools for dementia in Sri Lanka [37]. Umayal, et al. validated two scales: the modified Bristol Activities of Daily Living Scale (BADLS) and Blessed Activities of Daily Living Scale which are two questionnaires designed to measure the ability of a person with dementia to carry out their activities of daily living (ADL) [36]. The scales were found to be highly sensitive and specific for detecting dementia among older people living in care homes in Sri Lanka. The modified Bristol scale (area under the ROC: 0.933) was reported as being a better instrument than the modified Blessed scale (area under the ROC: 0.892) [36].
Suraweera, et al. validated and culturally adapted the Sinhala version of the Repeatable Battery for Assessment of Neuropsychological Status (RBANS) [42]. The authors report that the MMSE and MoCA scales that are currently used are difficult for people with cognitive impairment to complete and also not sensitive to mild cognitive impairment. The authors report that RBANS is sensitive in detecting both mild and severe cognitive impairment when compared to the MoCA and MMSE tools. The study shows the RBANS total scale correlated highly with the MMSE total score, (Pearson correlational coefficient = 0.793 p = 0.01). The sensitivity and specificity for the RBANS was 89% and 85%, respectively, at a total score of 80.5 (reliability coefficient was 0.929).
Domain 4: Dementia management in Sri Lanka
Recent situation of dementia care in Sri Lanka: De Silva has highlighted the importance of starting a national programme to tackle dementia in Sri Lanka [28]. In the absence of formal care services for people with dementia in Sri Lanka, there is a heavy reliance on informal care [28]. However, the credibility of the findings reported in this opinion paper is uncertain due to the lack of empirical evidence. Availability of specific drugs for all diagnosed patients, developing support and care programmes for patients and family caregivers, and further research was recommended to address the issue at a national level. Kuruppuarachchi and Lawrence argued that the Sri Lankan health system is lacking in health care services, such as providing emotional support, advice on practical and emotional aspects of caring, coping and loss, and keeping a balance between caregivers' personal life and their caring role [51].
Samaraweera states that Sri Lanka does not have a structured programme for detection and management of problems or conditions that are common among the elderly even though it has a National Policy for Elders [50]. Rodrigo, et al. in a letter to a journal, highlight the importance of improving mental health among older adults, the need for coordinating psychiatric and medical care to reduce disease burden and the need for routine screening of elderly patients for cognitive impairment [49]. Samaraweera contributes to this by suggesting a system to detect psychogeriatric problems such as dementia and depression at general out-patient clinics for older adults and to refer them to relevant professionals for further evaluation and treatments of the detected conditions; and also, to develop services both in acute and primary care settings [50].
Williams states in a conference abstract that 'developing a cost-effective, sustainable and equitable service for older adults with dementia is a challenge in Sri Lanka' [21]. His suggestion is to deviate from the medical model and to focus on implementing a social model of care for people with dementia in collaboration with families and the community. The author further stresses that the westernised 'resource-hungry models' applied in high-income countries would not be applicable to Sri Lanka. Samaraweera suggests integrating volunteers from elders' societies, village leaders, social workers with health care professionals in both community and hospitals to care for both affected older adults and their caregivers and also to enable quality care for the elderly in Sri Lanka [50]. The authors also stress the importance of non-pharmacological interventions [50] and community-based activities [38] to control and manage dementia among older adults. According to the experience and observations of Marçal-Grilo [26] (a volunteer community dementia nursing specialist), most of the dementia care provision is limited to the city of Colombo and provided primarily in the hospital setting rather than via community-based services. He writes that the 'medical model is practised widely and considered as the best approach currently due to limited numbers of nurses and doctors available in the older age care'. Encouraging informal care, introducing new care models and nurses' to take part in community-based dementia care services is 'challenge worthy' in managing dementia within local communities as the number of patients with dementia increase [26].
In addition to the government services, Marçal-Grilo (2014) discusses the work of the Lanka Alzheimer's Foundation (LAF), which acts as a non-governmental, charity organization to advocate and support the needs of people with dementia and people with cognitive impairment and their family members. Main activities of LAF include producing information about dementia, offering confidential support, training and psychological support for the informal caregivers, cognitive stimulating activities for people with dementia, programmes to reduce the level of stigma such as challenging some of the beliefs about dementia and encouraging open dialogue [26]. However, these services are only centralised in the district of Colombo.
Two papers describe the Ayurveda care model in treating dementia in Sri Lanka [45,46]. The authors report that medicinal and nutraceutical properties of ingredients of their Ayurveda drug called Sarasvata Choorna have memory enhancement and antidepressant qualities; therefore, the new drug may be used in the management of dementia and Alzheimer's disease. Sarasvata Choorna is a herbal preparation which consists of 12 medicinal plants and rock salt.
Caregiver Characteristics: Two papers [24,28] highlight that caring for people with dementia in Sri Lanka is mainly done by the family members. Abeywickrema, et al. report that, in a sample of 77 participants, the majority of informal caregivers (71.4%) were female (37.7% daughters and 21.1% wives) and 11.7% of them were over the age of 65 (mean age = 49 years). 83.1% of informal caregivers lived in the same household as the person with dementia [24].
Issues and Challenges of Caregiving: Samaraweera argues that not having a systematic referral system within the current health care system delays the identification of dementia and impairs the health services for people with dementia and their families [50]. The following challenges were identified in the formal, community and home-based care settings when providing care services to people with dementia by Marçal-Grilo [26]:
• No professional assistance for families who are living with a person with dementia.
• Diagnoses at the community level are difficult as specialist dementia care services are scattered or not available.
• Power struggles and resistance to change among health care professionals.
• Authoritative expert role among some health professionals offers little room for multidisciplinary approaches to dementia care.
• Health information and knowledge are considered as 'resources to hold on to' rather than share with the patient or family members.
Concerning informal caregiving, Marçal-Grilo (2014) identified the lack of understanding of behavioural problems, lack of access to health care, shame and stigma, limited support in the caregiving role, and emotional and practical aspects of caregiving as the main challenges faced by informal caregivers. He stated that memory loss and disorientation is commonly mistaken as a part of normal ageing; therefore, the signs and symptoms are usually ignored until the issues become unmanageable. According to this report dementia often drags families into social deprivation and poverty, and contributes to inequalities in society and access to health care.
Though it is only indirectly related to dementia caregiving, Thanthrige, Dassanayake and Dissanayake report that older adults with severe cognitive impairment have a significantly higher falling tendency (p = 0.001) [48]. In their study, the older people with cognitive impairment demonstrated poor functional lower extremity strength and balance, with a positive correlation observed between cognitive function and lower extremity strength (r = 0.469, p = 0.001) [48].
Perceived stigma around mental illness has been argued to be the main obstacle for seeking help and medical advice in Sri Lanka [26] Looking after older adults with dementia within the family is becoming a challenge in Sri Lanka as the traditional 'closely-knit' family structure is changing due to demographic transitions such as the increased tendency for nuclear families and migration for employment [51].
A study focuses specifically on caregiver burden which is measured using the Zarit Burden Interview [24]. In this study sample (n = 77), 43% were experiencing a mild to moderate burden, 26% were experiencing moderate to severe levels of caregiver burden and 6.5% of the family caregivers reported a severe burden. The increased age of the caregiver (p = 0.02) and lack of family support (p = 0.04) increased the caregiver burden, while increased household income significantly reduced the burden of care (p = 0.004) [24]. This study revealed that marital status, employment status of the caregivers and BPSD exhibited by the affected older adults were not associated with caregiver burden. There was no significant association between the level of caregiver burden and the presence of depression (p = 0.31). However, 3.9% of the study participants presented with major depression when screened [24]. De Silva et al. investigated the efficacy of treatment of AD patients with rivastigmine for 20 weeks, finding that this produces a significant improvement in their ADL functioning (p < 0.001), and subsequently lowers the caregiver burden [27].
Skills in dementia care: According to Marçal-Grilo, specialised care for older adults is in the hands of a limited number of health professionals and the percentage of nursing staff working directly with those aged 65 and over is unknown [26]. Based on the author's observations during his volunteer work in Sri Lanka, Marçal-Grilo reports that specialised dementia support is 'patchy and limited' due to a lack of formal post-registration training in old age care and mental health for nurses in Sri Lanka [26]. Findings of another study [50] suggests to include geriatrics as a mandatory requirement in undergraduate and postgraduate curricula in order to improve the knowledge and skills among nurses, doctors and paramedical professionals.
Discussion
A total of 28 papers on dementia-related studies or opinion pieces specifically looking at older adults conducted in Sri Lanka were identified and included in the narrative synthesis in the review. The papers reviewed were mapped across four results-generated domains: epidemiology, pathophysiology, screening for dementia, and dementia management. The International Consortium for Health Outcome Measurement (ICHOM) standard set for dementia (https://www.ichom.org/portfolio/dementia/) recommends a set of domains which highlights the outcomes that matter most to persons with dementia. These five broader domains include: Symptoms, functioning and quality of life, carer, sustainability, safety and clinical status of the person with dementia. When compared to these domains, the evidence extracted from the current systematic review indicated that most of the aspects are missing in Sri Lankan dementia literature. It appeared that the aspects related to carers and the people with dementia (e.g. quality of life, wellbeing, full-time care engagement, falls, hospital admissions, disease progression and overall survival) have not yet been explored in the Sri Lankan context.
Results indicate that dementia prevalence has been studied in only three districts in Sri Lanka: Matara, Colombo and Jaffna [23,38,43]. Furthermore, there are limitations of these studies, such as small sample size, high dropouts [23] and no community samples [43]; leading to these papers being appraised as low-quality. Due to lower strength of evidence from most of the papers included it is not possible to draw any firm conclusions from the data available. Despite the limitations, the findings suggest a high prevalence of dementia among the rapidly increasing ageing population in Sri Lanka, when compared to other South Asian countries [52].
The review found very few studies reporting on dementia care management, and only one on caregiver burden in Sri Lanka. The only study conducted among informal caregivers was a descriptive survey using the ZBI questionnaire with a sample size of 77, and the researchers had not assessed the early issues and challenges of caregiving as they excluded the caregivers of patients with dementia diagnosed for less than 6 months [24]. The other papers on caregiving were opinion papers and conference abstracts [25,51] There is therefore a lack of empirical evidence on dementia management and caregiving in Sri Lanka, and, in particular, very little research exploring the views and experiences of caregivers and people with dementia.
Most papers [13] were classified in the domain of 'screening for dementia' and among them, eight were on translating and validating of screening instruments. This signifies an emerging research base in Sri Lanka, that dementia researchers are looking to culturally adapt and validate existing measures in order to compare with international standards. However, the practical application of most of these tools in assessment and screening for dementia during general clinic settings was minimal and less reported.
Although the global dementia literature continues to expand, the research output from Sri Lanka is limited. With the exception of five papers, all were published in 2015 or earlier. In particular, there are no recent prevalence studies; therefore, most of these findings may be out of date. It was noted that research gaps exist in areas such as dementia care, characteristics of formal and informal caregivers, and service provision for people and families with dementia. There is a need for high-quality research, as well as more empirical research, as several of the papers included in the review are opinion pieces, conference abstracts or letters to journal editors. Furthermore, it has also been argued that there is a need for more studies on the elderly concerning improving the health services such as conducting a psychological screening of older adults as routine clinic activities [50]. Kuruppuarachchi & Lawrence write in their opinion piece that 'there is a dearth of research related to dementia caregiver burden in Sri Lanka' [51]. This paper is now 14 years old, yet our review suggests that research in this area has not been forthcoming. A recent paper suggests further research on dementia caregivers in Sri Lanka in order to identify the true magnitude of the caregiver burden, issues and challenges and to develop services and support for caregivers [24].
Even though prevalence, caregiver burden and challenges of caregiving are universally reported [2,6,8,53-55], current information and research on the caregiver experience is lacking in Sri Lanka, reflecting the similar situation in other LMIC. Information at a localised level is important because emerging evidence suggests different models of care exist within different cultural contexts. For example, the majority of the studies and caregiving models on dementia predominantly come from developed western countries [14]. Also, studies have shown significant differences in how caregivers perceive the caregiving role for those with dementia in different countries [56-60].
Conclusion
This review has identified a dearth of high‐quality research activity on dementia in Sri Lanka. The majority of the studies were on validation of screening instruments. It was noted that research gaps exist in areas such as dementia prevalence, dementia care, characteristics of formal and informal caregivers, and service provision for people with dementia and their caregivers. The gaps identified through this systematic review regarding the lack of research on dementia management in Sri Lanka and particularly in care giving in informal settings where there have been no studies to-date- provides a strong rationale for encouraging more empirical research relating to dementia in Sri Lanka. Further research in these identified areas could have an important role in informing future policy on dementia care at local and national levels, and in the development of dementia care services, as well as understanding the challenges faced by families caring for people with dementia in the community and identifying ways to support these families.
Acknowledgement
The authors would like to thank Dr Jo Jordan, Dr. Opeyemi Babatunde and Dr Kaushalya Jayaweera for their guidance and support in developing the search strategy for the systematic review. Special thanks to the Post Graduate Institute of Medicine - Sri Lanka for giving library access for grey literature search.
Authors' Contribution
KA is the first reviewer of this systematic review. KA and AS carried out the study selection. KA and LD carried out quality appraisal and data extraction. KA wrote the initial draft of the paper; BS, PC and AS supervised overall review process and contributed in editing and correcting the paper.
Funding Sources
This work was supported by the School of Primary, Community and Social Care, Keele University, UK as a part of a PhD project of the first author.
Declaration of Conflicting Interests
We confirm that all authors had access to the data and a role in writing the manuscript. The authors declare that they have no conflicts of interest.
References
- WHO (2018) Global Health and Aging.
- Cao Q, Tan CC, Xu W, et al. (2020) The prevalence of dementia: A systematic review and meta-analysis. J Alzheimers Dis 73 :1157-1166.
- Hogan DB, Jetté N, Fiest KM, et al. (2016) The prevalence and incidence of Frontotemporal dementia: A systematic review. Can J Neurol Sci 43: 96-109.
- Nichols E, Szoeke CEI, Vollset SE, et al. (2019) Global, regional, and national burden of Alzheimer's disease and other dementias, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 18: 88-106.
- WHO (2015) WHO takes up the baton on dementia. Lancet Neurol 14: 455.
- Prince M, Bryce R, Albanese E, et al. (2013) The global prevalence of dementia: a systematic review and meta-analysis. Alzheimer's Dement. 9: 63-75.
- Ferri CP, Jacob KS (2017) Dementia in low-income and middle-income countries: different realities mandate tailored solutions. PLoS Med.
- Ferri CP, Prince M, Brayne C, et al. (2005) Global prevalence of dementia: a Delphi consensus study. Lancet 366: 2112-2117.
- Wu Y-T, Beiser AS, Breteler MMB, et al. (2017) The changing prevalence and incidence of dementia over time - current evidence. Nat Rev Neurol 13: 327-339.
- ADI (2015) The Global Impact of Dementia: An analysis of prevalence, incidence, cost and trends. London.
- ADI (2014) Dementia in the Asia Pacific region. Alzheimer's Australia, Alzheimer's Disease International.
- Makimoto K, Kang Y, Kobayashi S, et al. (2019) Prevalence of behavioural and psychological symptoms of dementia in cognitively impaired elderly residents of long-term care facilities in East Asia: A cross-sectional study. Psychogeriatrics 19: 171-180.
- Patel V, Shaji KS (2010) Mental illness in the elderly in South Asia. In: Principles and practice of geriatric psychiatry. (3rd edn), 730-733.
- Prince M, Acosta D, Ferri CP, et al. (2012) Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve: A 10/66 Dementia Research Group population-based cohort study. Lancet 380: 50-58.
- Patel V (2007) Closing the 10/90 divide in global mental health research. Acta Psychiatr Scand 115: 257-259.
- Chiao CY, Wu HS, Hsiao CY (2015) Caregiver burden for informal caregivers of patients with dementia: A systematic review. Int Nurs Rev 62: 340-350.
- Etters L, Goodall D, Harrison BE (2008) Caregiver burden among dementia patient caregivers: A review of the literature. J Am Acad Nurse Pract 20: 423-428.
- Hossain M, Crossland J, Stores R, et al. (2018) Awareness and understanding of dementia in South Asians: A synthesis of qualitative evidence. Dementia 1-33.
- Blakemore A, Kenning C, Mirza N, et al. (2018) Dementia in UK South Asians: A scoping review of the literature. BMJ Open.
- Peacock SC, Forbes DA (2003) Interventions for caregivers of persons with dementia: A systematic review. Can J Nurs Res 35: 88-107.
- Boland A, Cherry MG, Dickson R (2014) Doing a Systematic Review: A Student's Guide. (2nd Edn), Sage, London, England.
- Porritt BK, Gomersall J, Lockwood C (2014) Study selection and critical appraisal. Am J Nurs 114: 47-52
- De Silva HA, Gunatilake SB, Smith AD (2003) Prevalence of dementia in a semi-urban population in Sri Lanka: Report from a regional survey. Int J Geriatr Psychiatry 18: 711-715.
- Abeywickrema S, Weerasundera R, Ranasinghe K (2015) Assessment of the level of care-burden in informal caregivers of patients with dementia. SL J Psychiatry 6: 4-8.
- Williams S (2018) Dementia care: Issues and challenges in a developing Asian country. In: Asian Journal of Psychiatry.
- Marçal-Grilo J (2014) Sharing skills in dementia care with staff overseas. Nurs Older People 26: 35-39.
- De Silva HA, Pathmeswaran A, Gunatilake SB (2005) Efficacy of rivastigmine on activities of daily living in Sri Lankan patients with Alzheimer disease and on improving caregiver burden: A prospective study. Ceylon Med J 3: 106-109.
- De Silva HA (2005) Alzheimer's disease-time to act is now. Ceylon Med J 50: 1-4.
- De Silva HA, Gunatilake SB, Johnston C, et al. (2005) Medial temporal lobe atrophy, apolipoprotein genotype, and plasma homocysteine in Sri Lankan patients with Alzheimer's disease. Exp Ageing Res 31: 345-354.
- Wijesinghe P, Shankar SK, Chickabasaviah TY, et al. (2016) Cytoskeletal pathologies of age-related diseases between elderly Sri Lankan (Colombo) and Indian (Bangalore) brain samples. Curr Alzheimer Res13: 268-280.
- Wijesinghe P, Shankar SK, Chickabasaviah TY, et al. (2017) Vascular risk factors in manifestation of Alzheimer's disease related neuropathological changes: First autopsy and genetic evidence from a South Asian ageing population. J Cereb Blood Flow Metab 37: 196-197.
- De Silva HA, Gunatilake SB (2002) Mini Mental State Examination in Sinhalese : A sensitive test to screen for dementia in Sri Lanka. Int J Geriatr Psychiatry 17: 134-139.
- De Silva R, Disanayaka S, de Zoysa N, et al. (2009) Norms for the mini-mental state examination from a sample of Sri Lankan older people. Int J Geriatr Psychiatry 24: 666-670.
- Srinivasan S, Jaleel Q (2015) Norms for a neuropsychological test battery to diagnose dementia in the elderly: A study from Sri Lanka. J Neurosci Rural Pract 6: 177-181.
- Karunaratne S, Hanwella R, Silva V De (2011) Validation of the Sinhala version of the Montreal Cognitive Assessment in screening for dementia. Ceylon Med J 56: 147-153.
- Umayal S, Kulathunga M, Somaratne S, et al. (2010) Validation of a functional screening instrument for dementia in an elderly Sri Lankan population: Comparison of modified Bristol and Blessed activities of daily living scales. BMC Res Notes 3: 268.
- Kathriarachchi ST, Sivayogan S, Jayaratna SD, et al. (2005) Comparison of three instruments used in the assessment of dementia in Sri Lanka. Indian J Psychiatry 47: 109-112.
- Coonghe PAD (2015) Prevalence of mild cognitive impairment and its selected correlates among elders in Jaffna district.
- De Silva HA (2003) Alzheimer's disease in Sri Lanka. J Ceylon Coll Physicians 36: 14-26.
- Suraweera CU, Hanwella R, De Silva VA (2015) Medications used in dementia : A review of evidence. SL J Psychiatary 6: 3-8.
- Suraweera C, Hanwella R, Sivayokan S, et al. (2013) Rating scales validated for Sri Lankan populations. SL J Psychiatary 4: 16-24.
- Suraweera CU, Anandakumar D, Dahanayake D, et al. (2016) Validation of the Sinhala version of the Repeatable Battery for Assessment of Neuropsychological Status ( RBANS ). Ceylon Med J 61: 163-170.
- Dahanayake DMA, Isuru LLA, Aththanayake NNK, et al. (2016) Prevalence of behavioral and psychological symptoms of dementia and its association with the degree of cognitive impairment in patients presenting to the National Institute of Mental Health, Sri Lanka. SL J Psychiatary 7: 4-8.
- Ramanayaka RPJC (2004) Reasons for encounter and existing medical and psychosocial problems of geriatric patients in a general practice.
- Karunaratne TDN, Sugataratana K, Ariyawansa HAS, et al. (2017) A critical drug review of ingredients of Sarasvatha Choorna: Used as a remedy for dementia. J Innov Pharm Biol Sci 4: 43-47.
- Karunaratne TDN, Sugataratana K, Ariyawansa HAS, et al. (2015) Standardization of Sarasvatha Choorna: Used as a remedy for dementia. Am J Clin Exp Med 3: 288-292.
- Rajakumaraswamy N, Rajapakse IH, Fernando DJS (2008) The frequency of cognitive dysfunction in elderly Sri Lankans with type 2 diabetes mellitus. Int J Geriatr Psychiatry 23: 1205-1206.
- Thanthrige RS, Dassanayake S, Dissanayake D (2014) Relationship between increased risk of falling and cognitive impairment in residents of an elderly home in the Colombo district. Ceylon Med J 59: 21-23.
- Rodrigo C, Perera S, Adhikari M, et al. (2010) Cognitive impairment and symptoms of depression among geriatric patients in a tertiary care unit in Sri Lanka. Indian J Psychiatry 52: 279-280.
- Samaraweera DN (2014) Care of the elderly: A multidisciplinary approach. J Ceylon Coll Physicians 45: 45-48.
- Kuruppuarachchi K, Lawrence T (2006) Carer burden in dementia. Ceylon Med J 51: 44.
- The World Bank (2008) Sri Lanka Addressing the Needs of an Aging Population.
- Cao Y, Yang F (2020) Objective and subjective dementia caregiving burden: The moderating role of immanent justice reasoning and social support. Int J Environ Res Public Health 17: 455 .
- Alzheimer's Association (2015) Alzheimer's disease facts and figures. Alzheimer's Dement 11: 332-384.
- Rizzi L, Rosset I, Roriz-Cruz M (2014) Global epidemiology of dementia: Alzheimer's and vascular types. Biomed Res Int.
- Wijeratne C (2015) Dementia handbook for carers and health care professionals in Sri Lanka. One. Institute for Research & Development.
- Wang J, Xiao LD, He G, et al. (2014) Family caregiver challenges in dementia care in a country with undeveloped dementia services. J Adv Nurs 70: 1369-1380.
- Pattanayak RD, Jena R, Tripathi M, et al. (2010) Assessment of burden in caregivers of Alzheimer's disease from India. Asian J Psychiatr 3: 112-116.
- Schoonover J, Lipkin S, Javid M, et al. (2014) Perceptions of traditional healing for mental illness in rural Gujarat. Ann Glob Heal 80: 96-102.
- Hughes J (2013) Models of dementia care: Person-centred, palliative and supportive. A Discussion Paper for Alzheimer's Australia on Death and Dementia.
Corresponding Author
Kalpani Abhayasinghe, Faculty of Allied Health Sciences, General Sir John Kotelawala Defence University, Ratmalana, 10390 Sri Lanka; Institute for Research and Development in Health & Social Care, Battaramulla, Sri Lanka; Faculty of Medicine and Health Sciences, School of Primary, Community & Social Care, Keele University, Staffordshire, United Kingdom.
Copyright
© 2020 Abhayasinghe K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.