Original Fixation Technique for Periprosthetic Humeral Fractures: Locking Plate for Lockable Stem
Abstract
Introduction: The prevalence of periprosthetic humeral fractures is 0.6% to 3%. These periprosthetic fractures are very challenging to treat because of the risk of complications and reduced function, especially when the humeral implant needs to be changed. The aim of this study was to evaluate the possibility of stabilizing the fracture without removing the existing humeral stem.
Materials and Methods: Five patients with a mean age of 82 years (69-99) were analyzed. These patients had suffered a periprosthetic humeral fracture. The shoulder arthroplasty implant was either anatomical or reversed with a locked humeral stem. The fractures (4 Worland type C and 1 type B2) occurred an average of 57.5 months (1-156) after the arthroplasty. Plate fixation was done in all cases through an anterior surgical approach; the screws associated with the plate were inserted through the plate and into the holes in the existing humeral stem. The functional outcomes (Constant score, QuickDASH) and radiological outcomes (bone union, displacement) were evaluated until the fracture healed.
Results: Four patients were followed prospectively and the other was reviewed after a minimum follow-up of 1 year. There were no infections. One patient was lost to follow-up after 2 months. The mean surgery duration was 50 minutes (45-60). Four fractures healed within 3 months and one at 2 months. There were no intraoperative or postoperative complications. At a minimum follow-up of 6 months, the mean Constant score was 51 (32-60), the weighted Constant score was 79 (64-85) and the mean QuickDASH was 42 (18-38). All patients had regained the range of motion they had before the fracture. None of the patients required reoperation and all had returned to the same quality of life as before the fracture within 3 months.
Conclusion: Analysis of these five cases shows the feasibility and simplicity of using the holes in the existing lockable humeral stem to stabilize a plate manufactured specifically for this type of stem. For periprosthetic fractures in patients who already have a lockable humeral stem, a stable construct can be achieved that firmly binds the diaphysis and implant. This type of construct allows the existing humeral stem to be preserved in cases of complex periprosthetic fractures in older adults and the operating time to be shortened.
Keywords
Periprosthetic humeral fracture, Locking plate, Original technique
Introduction
The indications for anatomical or reversed shoulder arthroplasty have increased as the world population ages. Lockable humeral stems are being increasingly used in trauma cases and in scheduled surgery as they do not require cementing and they eliminate potential complications during implant revision, especially in older adults. In 2019, 4100 lockable stems were implanted in France and other countries with a 200% growth rate over 4 years.
The prevalence of periprosthetic fracture after shoulder arthroplasty is 0.6% to 3% and it makes up 20% of complications according to Steinmann, et al. [1]. The incidence of periprosthetic fractures in the humerus is reported to be between 1.6% and 2.4% according to Seybold and al [2]. Periprosthetic fractures of the humerus following shoulder arthroplasty are very complex cases to treat and have a risk of complications and loss of function. Current treatment options are conservative treatment, surgical treatment involving fixation (typically wire cerclage) and revision arthroplasty with a longer stem combined with wire cerclage. The indication depends on the fracture's location as defined by Worland, the fracture's displacement, and the patient's overall health.
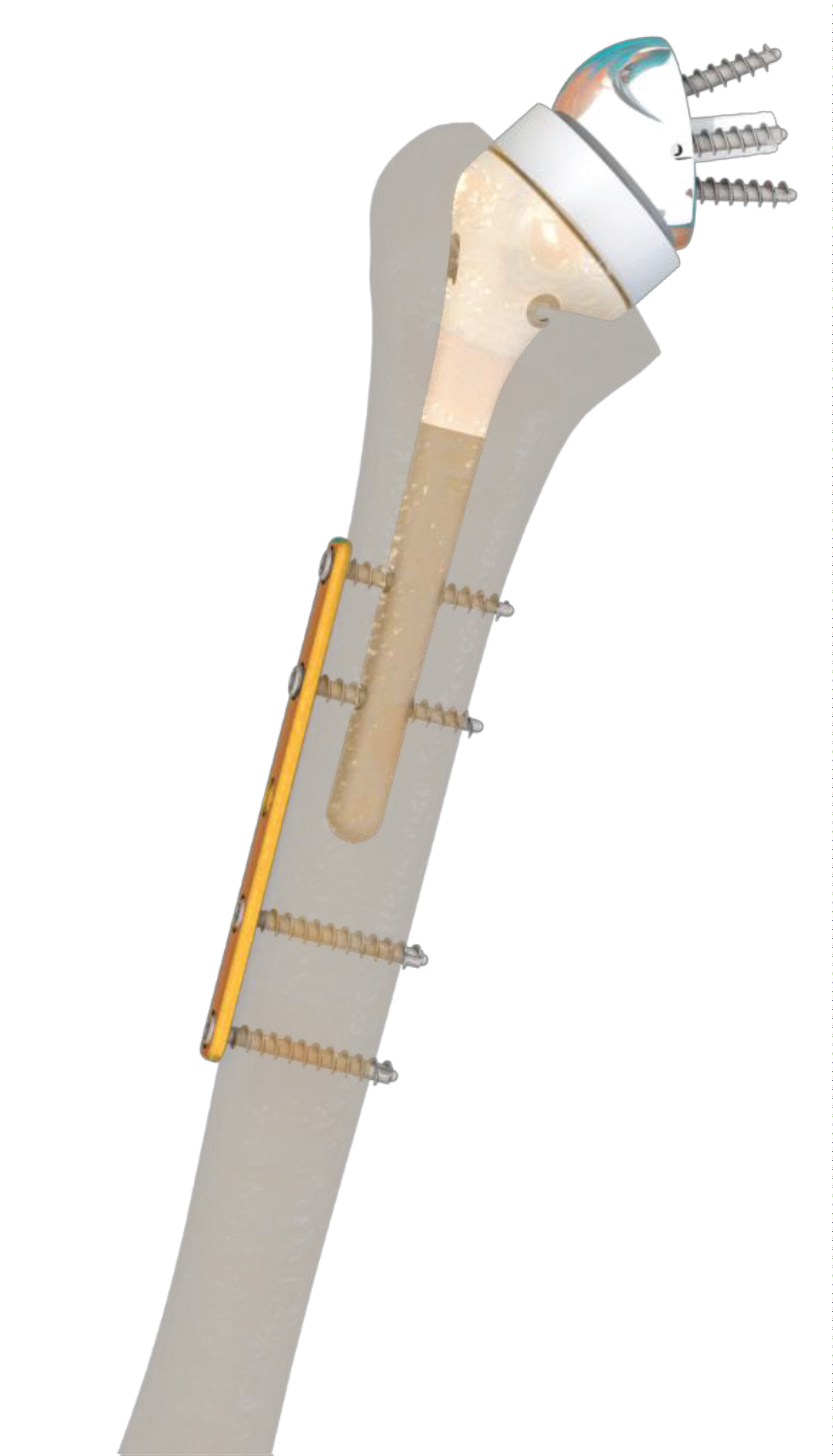
We have devised an alternative fixation technique in which a specifically designed plate is used to secure the fracture, with the plate's screws being inserted in the locking holes on the existing humeral stem. The fact that the humeral stem is mechanically interdependent with the plate via the locking screws eliminates potential stem instability; instability would theoretically require replacing the existing stem with a longer one. The concept behind this technique is to use the stem's locking holes to secure an osteosynthesis plate. These locking holes are initially designed to stabilize the stem at the desired height and retroversion.
The stems that can be used are the Humelock 2 and Humelock reversed stems:
The Humelock 2 is a lockable stem that exists in an anatomical or inverted version, low profile, developed in 2008, dedicated to cephalo-tuberosity fractures where the humeral head's vascularization is compromised, with slightly comminuted and ideally non osteoporotic tuberosities, and accessible to an anatomical reconstruction.
The Humelock Reversed is an inverted cementless stem, with a locking option if necessary, developed in 2011. The epiphyso-diaphyseal angle is 145 degrees. It can be used either in elective surgeries like in the context of rotator cuff arthropathy, or in trauma cases for example in cephalo-tuberosity fractures with high degrees of tuberous comminution, and possible osteoporosis.
The aim of this study was to determine if this fixation technique will allow early mobilization of the patients' shoulder so they can regain the function they had before the fracture and allow us to consider treating more complex fractures by stabilizing the humeral stem instead of changing it.
Methods
We present the results of a retrospective, multicenter case series.
All the surgeons (17, across 4 centers) who ordered the PRCT 2 plate from the FX Solutions laboratory were contacted. A discussion with the surgeon was able to exclude cases in which the plate was used for a humeral fracture in the absence of an orthopedic implant.
5 cases of actual periprosthetic fractures where the locking holes were used to stabilize the fracture were identified. We were able to study all 5 cases, with none lost to follow-up.
We compiled the cases operated using this technique up to now: 5 patients with a mean age of 82 years (69-99) who suffered a periprosthetic fracture after shoulder arthroplasty (4 weeks to 13 years after) in 2018 or 2019 at the Princess Grace, Saint Etienne and Savoie de Chambéry hospitals. The existing humeral stems were not cemented and could be locked with two optional screws; the arthroplasty had either an anatomical or reversed configuration. The patients' preoperative characteristics are shown in Table 1.
Preoperative planning consisted of AP and lateral radiographic views of the humerus and a CT scan to define the fracture line, bone stock and implant stability.
The Humelock reversed and Humelock 2 stems (FX Solutions©, Viriat, France) have the distinctive feature of being lockable with two 4.5-mm holes in the stem. The PRCT 2 plate marketed by the same company is a diaphyseal plate that has the same center-to-center hole spacing as the locking holes on the stem. Thus, the spacing between the two holes on the stem is the same as the spacing between the two proximal holes on the plate. Each hole in the plate can accept a screw, which can be either locking or cortical. The plate is available with 5, 7 and 9 holes, while the 4.5-mm diameter screws are available in 20 mm to 60 mm lengths with a 5 mm thread. The stem, plate and screws are made of TA6V titanium alloy.
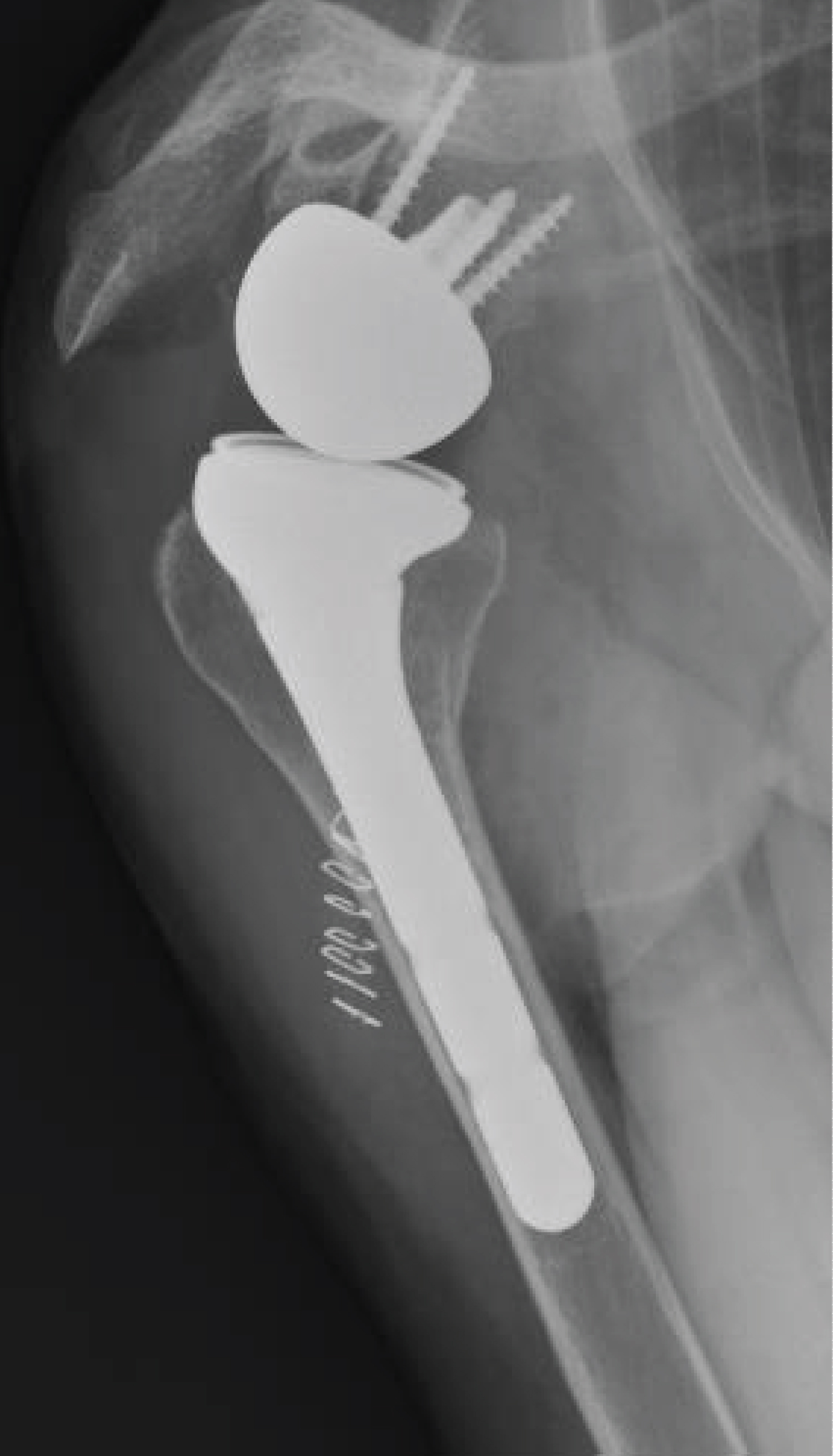
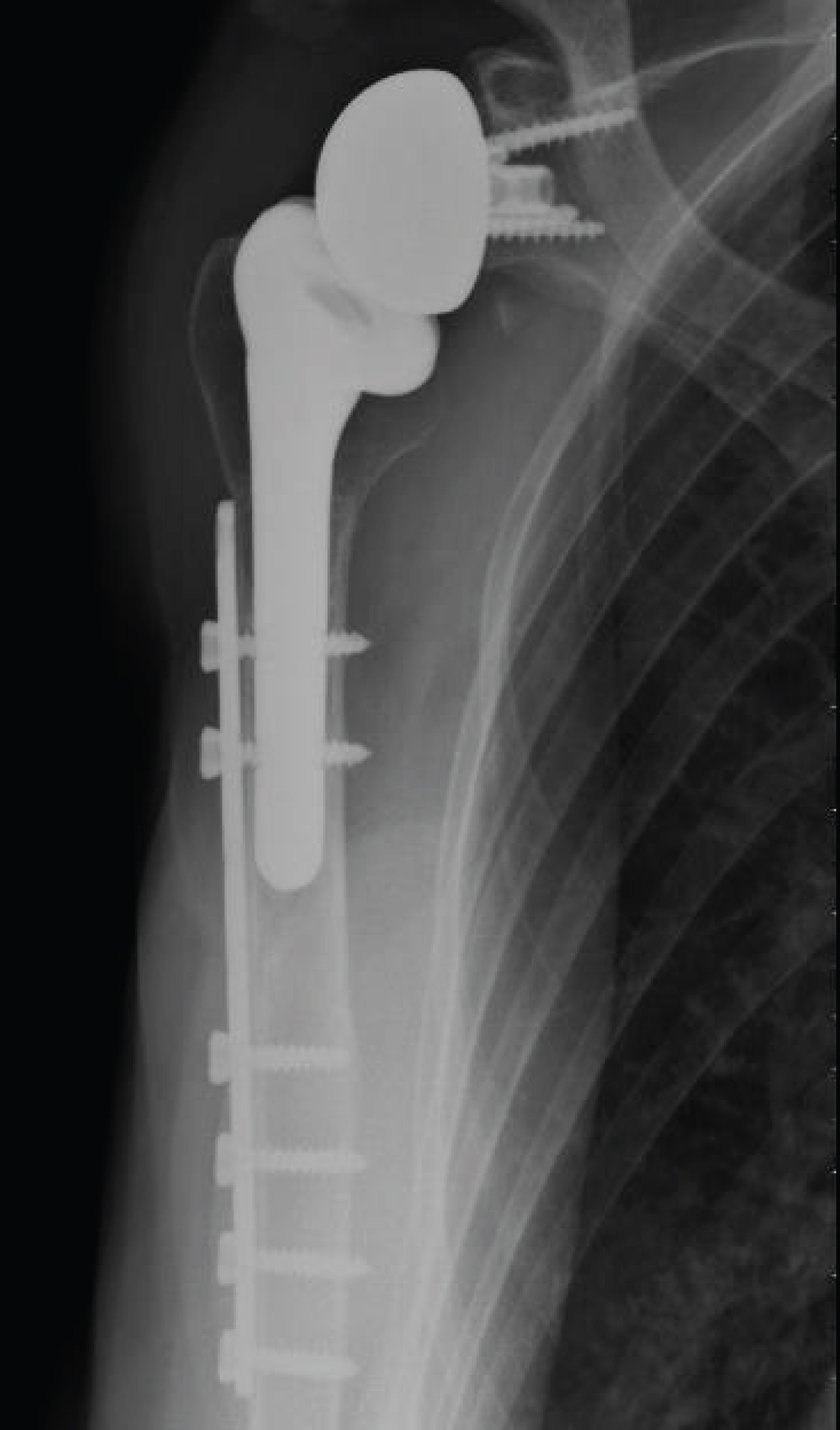
Patients were set up in the beach-chair position, and the deltopectoral approach was extended toward the diaphysis using a lateral approach. The absence of implant loosening was confirmed intraoperatively. Once the fracture site had been exposed, it was reduced with a clamp. The holes on the existing stem were located using the round hole technique with fluoroscopy. Then the fracture plate was applied. A shoulder immobilizer was used immediately after the surgery to control pain and was removed 10 days later. Physiotherapy was initiated early on with instructions to use modalities to reduce pain and to passively mobilize the shoulder, elbow and wrist below the pain threshold. Active mobilization was initiated on the 15th postoperative day. Figure 1 and Figure 2 illustrate this technique.
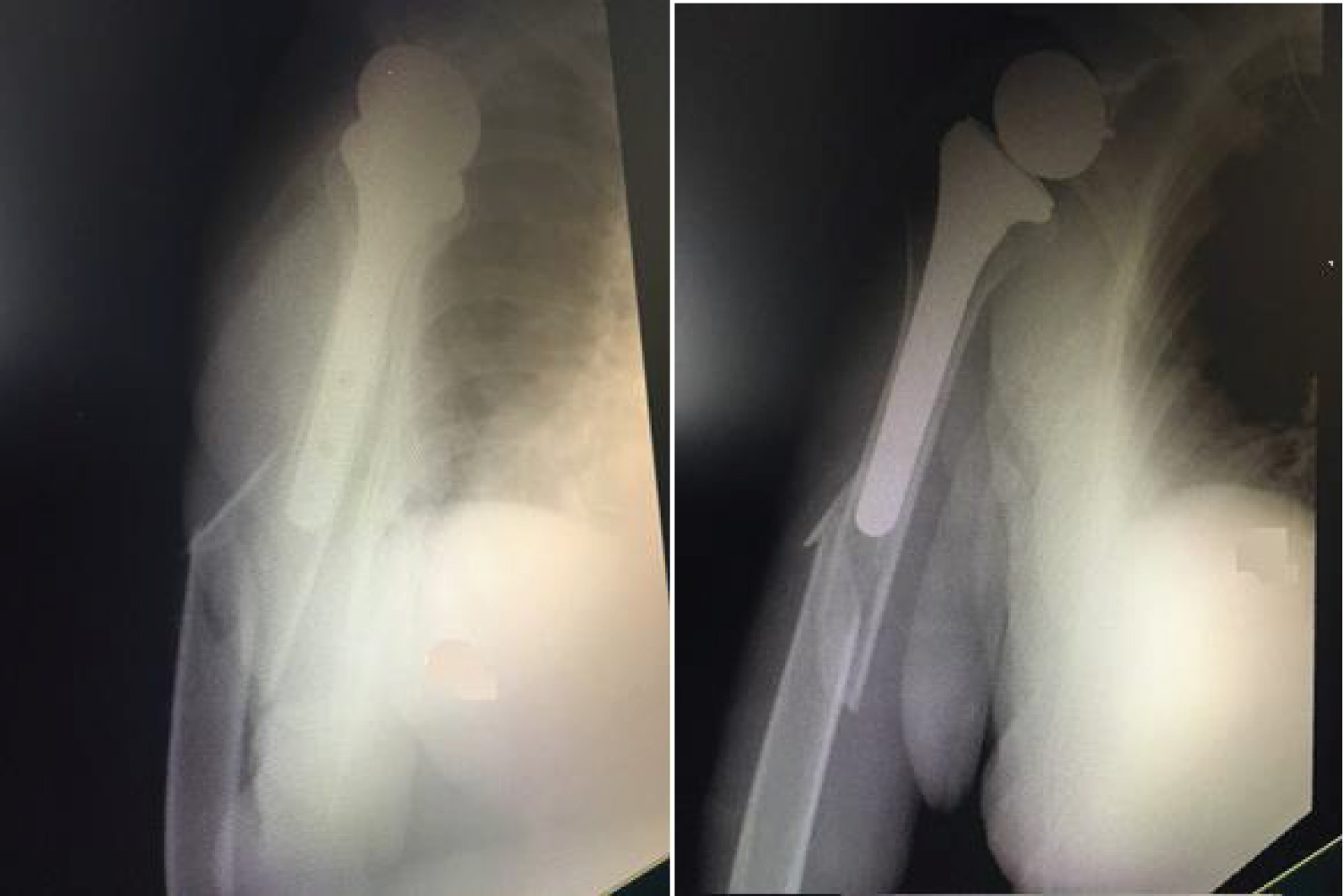
An example of the radiographs made for patient 3, before the fracture, at the time of the fracture, immediately postoperative and at bone union is shown in Figure 3, Figure 4, Figure 5 and Figure 6.
The functional outcomes (Constant score, QuickDASH) and radiological outcomes (bone union, displacement) were evaluated by the surgeon until the fracture had healed. Bone union was defined as the presence of at least three continuous cortices on two orthogonal radiographic views. The patient's autonomy level and overall satisfaction level were collected on medical files. One examiner reviewed the three patients treated at Princess Grace Hospital to evaluate range of motion and the Constant and QuickDASH scores. For the patients treated at the Chambéry and Saint Etienne hospitals, this information was reported by the surgeon who had operated on the patients.
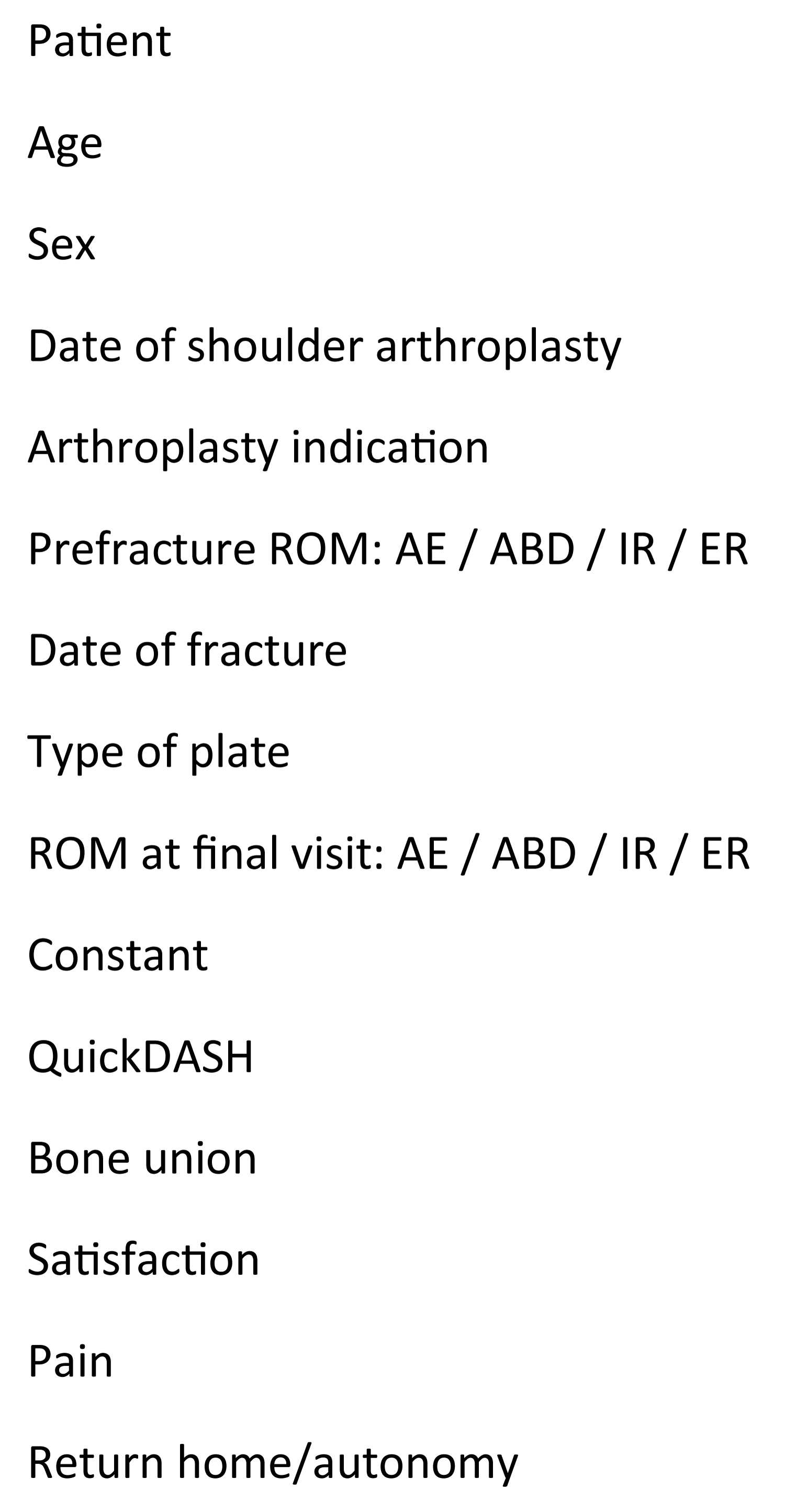
The data collection sheet is shown in Figure 7.
Results
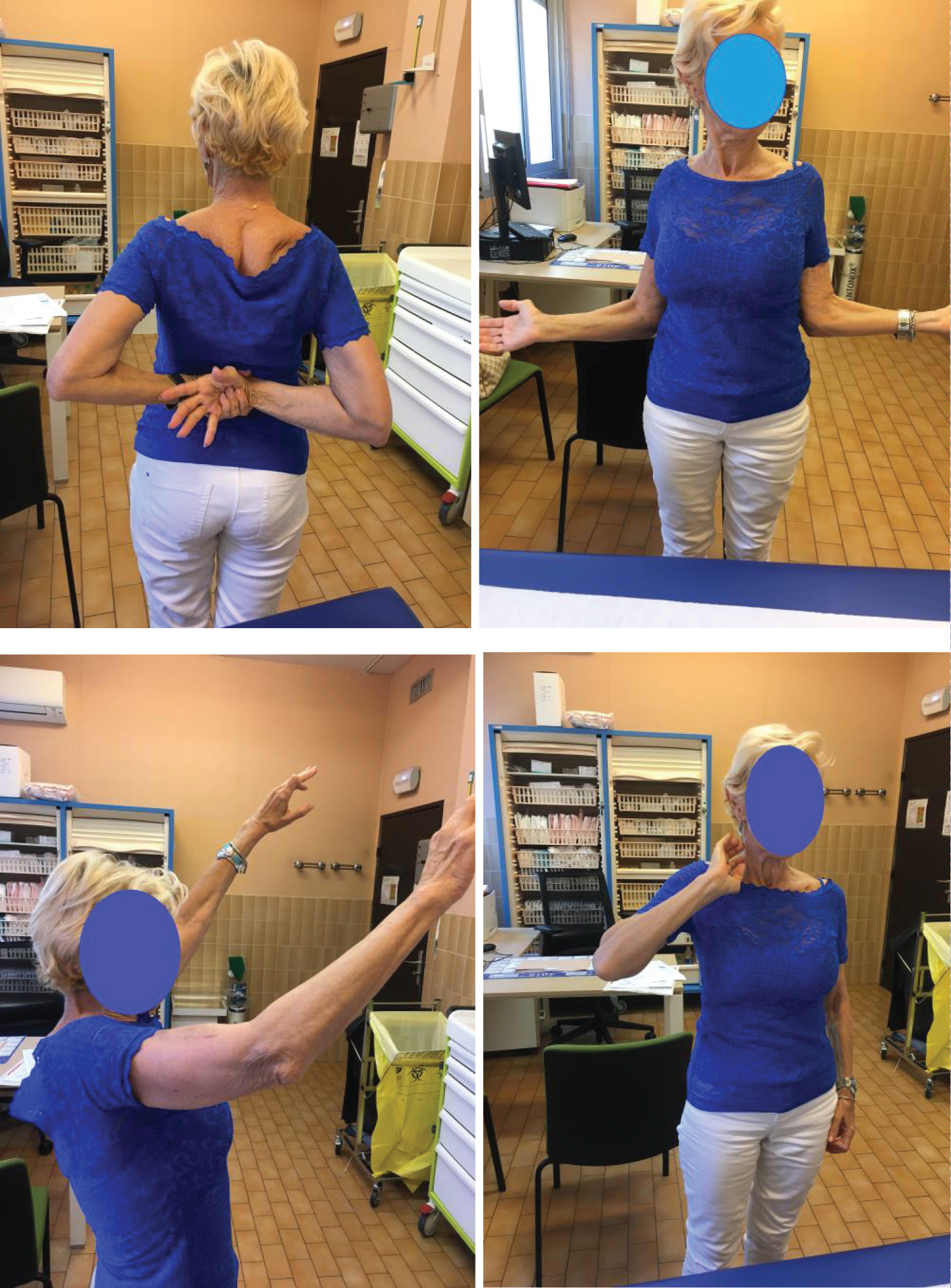
There were no intraoperative or postoperative complications. The mean duration of the surgery was 50 minutes. Of the five treated fractures (four stage C and 1 stage B2 in the Worland classification), one had healed after 2 months and four after 3 months. None of the patients required reoperation. The patients' quality of life was similar to what it was before the fracture: Mean Constant score of 51 (32-60), weighted Constant score of 79 (64-85) and mean QuickDASH of 42 (18-38). There were no infections as of the 6-month follow-up visit. Four patients had regained the same range of motion as before the fracture; no data was available for the fifth patient who suffered the periprosthetic fracture early after the arthroplasty. The range of motion in patient 3 (reversed arthroplasty) at 3 months' post-fracture is shown in Figure 8.
All five patients were able to return home: three immediately upon being discharged from the hospital and two after a stay at a rehabilitation facility (including a 100-year-old patient).
The postoperative data are shown in Table 2.
Discussion
The functional outcomes achieved in our first few patients encourage us to continue this type of treatment for periprosthetic humeral fractures with an existing lockable stem, and to potentially extend the indication for preserving the humeral implant even in more complex fractures.
This novel fracture fixation technique achieved stable diaphysis-implant fixation in these five cases without having to open the joint or change the stem for a revision implant. This technique allows early mobilization of the arm and recovery of the range of motion to prefracture levels. To our knowledge, this type of technique has not been described in the literature before now.
We recommend this technique for Worland B2 and C periprosthetic fractures on Humelock 2 or Humelock Reversed FX-Solutions laboratory locking stems. This stem has 2 locking holes with a center distance that corresponds to the center distance of the dedicated PRCT 2 plate developed by the laboratory for this indication.
The treatment of periprosthetic humeral fractures must take into account the patient's advanced age and potential bone loss in a bone that is often already osteoporotic.
The key point remains determining whether the existing implant is stable. Our analysis of the literature on this subject did not provide a definite conclusion. It is not always easy to estimate the stability of cementless stems when dealing with a periprosthetic fracture before testing the stem's stability in situ. Sometimes the stem moves height-wise or rotation-wise and the stem's instability is discovered on the x-ray. We can then logically consider to change the stem.
When the stem is cemented, and when we see on the x-ray that the fracture has fragmented or even excluded pieces of periprosthetic cement, we can once more predict the unstable nature of the stem.
However, especially in cimentless stem periprosthetic fractures, it is sometimes only the situ testing that allows us to truly test the stem's stability.
The excellent recent literature review on this subject by Gebrelul, et al. [3] puts forth a detailed decision tree depending on the type of fracture but remains fairly subjective when it comes to assessing the stability of the humeral implant on the preoperative images.
We believe that when there is a doubt about the stability of the implant, only intraoperative testing will allow us to decide. If the locking holes were accessible during the osteosynthesis procedure, we passed an arthroscopic hook through the stem's locking holes: if the implant did not move then we considered it stable. If the holes were not accessible, we evaluated the stability by directly mobilizing the stem using small forceps in order to imitate the stress in cranio-caudal translation and in rotation.
Per-operative x-rays must allow us to specify the precise location of the fracture line: if the fracture line passes through the locking holes, then this technique cannot be used. The other contraindications are sinking or rotary disturbance of the stem.
The aim of the treatment is to achieve fast bone union while optimizing functional recovery (pain control and early motion) to limit the loss of autonomy in older patients who suffer this fracture. Surgical treatment must minimize the neurological and infection-related risks, along with implant instability and subsequent joint stiffness.
Risk factors for periprosthetic fractures in the shoulder have been described in the literature: female gender, advanced age, osteoporosis, and rheumatoid arthritis [1,4]. The five patients in our case series were all female, with a mean age of 82, and three had confirmed osteoporosis.
Periprosthetic humeral fractures can be treated either conservatively or surgically by plate fixation (screws around the implant and wire cerclage) or by replacing the existing humeral stem with a longer revision stem that bridges the fracture site. The treatment choice depends on patient- and fracture-related factors (location of fracture and stability of existing implant), which are analyzed using radiographs and CT scans to classify the fracture as described by Worland [5].
The treatment indications are well established in the literature [1,4,6] and indications are summarized in Table 3. In Worland C fractures, we prefer a surgical treatment that consists in an anatomical reduction of the fracture, favoring a short consolidation time according to Campbell [7]. A stable fixation of our assembly allows early rehabilitation, thus limiting the complications that come with immobilization according to Campbell, et al. [7].
One of the biggest problems associated with these fractures is that they occur in older adults with osteoporotic bone. Thus, there is a high risk of delayed union or nonunion: Kurma, et al. [8] showed a mean time of 6 months for conservative treatment and Sewell, et al. [9] reported bone union in 7 months after changing the stem. Campbell described achieving bone union in 2.3 months in patients who received intramedullary fixation (long stem that bridges the fracture and extends more than 3 cortical diameters beyond the fracture site), in 3.5 months in those who underwent conservative treatment and in 8.7 months in those who received a standard stem with a different internal fixation method. We feel that the union time in our case series (3 months) can be attributed to the stable intra-prosthetic and periprosthetic fixation achieved by adding two screws to the plate that went through the locking holes on the existing humeral stem.
The complication rate reported in the literature after surgical treatment is high in some situations:
• Nerve-related complications radial, ulnaire, musculo cutané: 2 of 9 patients for Wright [10], 4 of 21 for Campbell [7] and 2 of 22 patients for Sewell [9].
• Instability: three dislocations reported by Sewell [9].
• Infection: 1 for Sewell [9], 1 for Kumar [8], 1 for Campbell [7].
• Capsulitis: 1 for Campbell [7].
• The other potential complications are unraveling of the materials and non-union.
The consequences of this type of fracture on shoulder joint motion can be significant: loss of mobility is responsible for 9 of the 16 patients being dissatisfied in the Kumar [8] study and 6 of the 9 patients in the Wright study [10].
Our literature review is summarized in Table 4. The fact that the joint is not opened, and the existing stable stem is preserved, while ensuring stable fixation of the fracture, allows the patients to start rehabilitation early on, thus preventing joint stiffness.
The advantages and disadvantages of the available surgical treatments are listed in Table 5.
The main limitation of our study is, of course, its small sample size; because the prevalence of this fracture is low, there are few studies on this topic and the statistical power is low. The data-collecting by the surgeons of the two cases underwent surgery in the other hospital is another bias.
Conclusion
Our analysis of the first five cases of periprosthetic fracture on lockable humeral stems shows that the fracture and existing implant can be stabilized in a reliable manner.
A specially designed fixation plate that uses the locking holes of the existing stem provides a stable fracture construct that allows early rehabilitation while ensuring optimal cohesion between the diaphysis and the implant.
The good outcomes in these five cases encourage us to continue treating periprosthetic fractures on locking humeral stems with this technique, whenever possible. As we gain experience with additional cases, it may be possible to treat more complex periprosthetic fractures without having to open the glenohumeral joint to change the stem.
We are collecting data from all the cases in which this technique is used in France. Further prospective studies with large number of cases should be performed to confirm our results.
Ethical Statements
Human and animal rights
The authors declare that the work described has been carried out in accordance with the Declaration of Helsinki of the World Medical Association revised in 2013 for experiments involving humans as well as in accordance with the EU Directive 2010/63/EU for animal experiments.
Informed consent and patient details
The authors declare that this report does not contain any personal information that could lead to the identification of the patient(s) and/or volunteers.
Disclosure of interest
The authors declare the following financial or personal relationships that could be viewed as influencing the work reported in this paper:
Damien BERTRAND: This author, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
Tristan LASCAR: Receive royalties from FX solutions.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contributions
All authors attest that they meet the current International Committee of Medical Journal Editors (ICMJE) criteria for Authorship.
References
- Steinmann SP, Cheung EV (2008) Treatment of periprosthetic humerus fractures associated with shoulder arthroplasty. J Am Acad Orthop Surg 16: 199-207.
- Seybold D, Citak M, Königshausen M, et al. (2011) Combining of small fragment screws and large fragment plates for open reduction and internal fixation of periprosthetic humeral fractures. Int J Shoulder Surg 5: 105-107.
- Gebrelul A, Green A, Schacherer T, et al. (2018) Periprosthetic humerus fractures: Classification, management, and review of the literature. Ann Join 3: 49.
- McDonough EB, Crosby LA (2005) Periprosthetic fractures of the humerus. Am J Orthop Belle Mead NJ 34: 586-591.
- Worland RL, Kim DY, Arredondo J (1999) Periprosthetic humeral fractures: Management and classification. J Shoulder Elbow Surg 8: 590-594.
- Mineo GV, Accetta R, Franceschini M (2013) Management of shoulder periprosthetic fractures: Our institutional experience and review of the literature. Injury 44: S82-S85.
- Campbell JT, Moore RS, Iannotti JP, et al. (1998) Periprosthetic humeral fractures: Mechanisms of fracture and treatment options. J Shoulder Elbow Surg 7: 406-413.
- Kumar S, Sperling JW, Haidukewych GH, et al. (2004) Periprosthetic humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am 86: 680-689.
- Sewell MD, Kang SN, Al-Hadithy N, et al. (2012) Management of peri-prosthetic fracture of the humerus with severe bone loss and loosening of the humeral component after total shoulder replacement. J Bone Joint Surg Br 94: 1382-1389.
- Wright TW, Cofield RH (1995) Humeral fractures after shoulder arthroplasty. J Bone Joint Surg Am 77: 1340-1346.
Corresponding Author
Damien Bertrand, Medecine Doctor, Centre Hospitalier Princesse Grace 1 Avenue Pasteur 98000, Monaco, Tel: 0687453534.
Copyright
© 2021 BERTRAND D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.