Optimizing Fixation: Flexible Nailing for Pediatric Distal Tibial Fractures
Abstract
Background: Pediatric tibial shaft fractures are among the most common long bone fractures in children, with distal tibial fractures presenting unique challenges due to anatomical and biomechanical characteristics. While conservative treatments are preferred for midshaft fractures, distal tibial fractures may require surgical stabilization. Flexible intramedullary nailing is a viable option, however it may demand specific modifications to optimize fixation and reduce complications. This technique paper describes a modified flexible intramedullary nailing technique for pediatric distal tibial fractures aimed to improve fracture stability, minimize loss of reduction, and enhance post-operative outcomes.
Methods: The technique involves the use of two C-shaped titanium or stainless steel nails, with specific modification tailored for the distal tibial fractures. This includes increasing the curvature of the nail tip to up to 40 degrees to enhance stability at fracture site. Key surgical steps such as nail selection based on patient age and weight and postoperative protocols including early mobilization and weight bearing progression are also outlined.
Results: The described technique provides a reproducible and minimally invasive approach to managing pediatric distal tibial fractures. Compared to other fixation methods such as plating, flexible nailing preserves periosteal blood supply, minimizes soft tissue disruption, and allows for dynamic fracture stabilization. Literature review suggests that flexible nailing has positive healing outcomes, reduced risk of malunion, and lower rates of physical injury. Studies have reported that there is an average healing time of 9 weeks with minimal complications.
Conclusion: Flexible intramedullary nailing is an effective and reliable technique for managing pediatric distal tibial fractures when modified appropriately. By optimizing nail curvature, placement, and reduction strategies, this method helps with stable fixation and preserving the bone. The technique is a practical alternative to more invasive fixation methods and promotes improved long-term outcomes in pediatric patients.
Keywords
Pediatric tibial fractures, Distal tibial fractures, Flexible intramedullary nailing, Modified nailing technique, Fracture stabilization, Surgical technique, Fracture reduction
Introduction
Pediatric tibial shaft fractures are the third most common diaphyseal fracture in children, following forearm and femur fractures. These injuries typically result from high-energy trauma, such as motor vehicle accidents and sports-related incidents, with 30% presenting alongside fibular fractures [1]. Unlike adults, pediatric bones have significant growth potential and remodeling capacity, allowing slight misalignments to correct over time. Therefore, uncomplicated midshaft fractures are frequently managed conservatively with closed reduction and casting [2,3].
Uncomplicated middle third tibial shaft fractures can be reduced to acceptable alignments-less than 5° varus or valgus, 10° anterior or posterior angulation, 10° rotational deformity, and 1 cm of shortening in children under 8 years [4]. However, distal third tibial fractures present unique challenges often requiring surgical intervention, such as flexible intramedullary nailing.
This technique, employing two C-shaped nails into the intramedullary canal, has demonstrated efficacy but presents distinct challenges in distal third fractures due to anatomical and biomechanical factors. Distal tibial metaphyseal fractures, although rare accounting for 0.35-0.45% of pediatric fractures [5], are prone to complications including loss of reduction, malunion, and ankle dysfunction. Achieving stable fixation near the distal end often requires modifications to traditional flexible nail constructs to improve stability and reduce complications.
This study aims to identify modifications to the flexible intramedullary nailing technique that enhance fixation and minimize postoperative complications in pediatric distal tibial fractures. By refining this method, we seek to provide a reproducible and effective construct for treating these challenging injuries, ensuring better long-term outcomes for pediatric patients.
Description of the Method
Indications
Operative fixation is indicated for unstable distal tibia fractures, including those with unacceptable reduction, open fractures, significant shortening, displacement, or angulation of distal fragment exceeding 10 degrees varus with an intact fibula [4] (Figure 1).
Positioning
Under general anesthesia, patient is positioned supine on the operative table with padding to protect bony prominences. A non-sterile tourniquet may be placed for potential intraoperative needs.
Operative Technique
First, fluoroscopy is utilized to identify the fracture site. The mobility of the distal fragment is assessed and a provisional reduction is attempted (Figure 2).
Next, nail selection involves choosing either titanium nails for flexibility and rotational stability, or stainless steel nails for added rigidity and children over 45 kg [6,7]. Each nail should be 0.4 times the medullary canal diameter. In children ages 6-8, 2.5 mm nails are recommended, 3 mm for ages 8-10, 3.5 mm for children older than 11, and 4 mm for skeletally immature adolescents. Nail length is determined as 20 mm from the distance between the proximal and distal tibial physis. Given the distal location of the fracture site, a curvature of up to 40° is applied to the distal end of the nail so the apex of the curve reaches the fracture site, aiding in reduction stabilization.
Next, lateral entry point is made with a 2-3 cm longitudinal incision over the anterior compartment musculature between the tibial crest and the fibula head, 10-30 mm distal to the proximal physis. After blunt dissection, fascia splitting anteriorly, and lifting the anterior 6 compartment musculature off the tibia, a drill is utilized under fluoroscopy to enter the cortex anterior to the lateral border of the interosseous membrane attachment site. The modified nail is inserted using an inserter/T-handle with the curved tip perpendicular to the medial cortex (Figure 3). Oscillatory motions facilitate entry into the medullary canal until contact is made with the far cortex. The nail is then advanced by a mallet proximal to the fracture site before addressing the medial nail.
A similar incision is made over the medial tibia, 10-30 mm distal to the proximal physis. After blunt dissection to the bone posterior to the midsection of the medial metaphysis, a drill is utilized under fluoroscopy to create an entry hole between the pes anserine tendons and the medial collateral ligament insertion site. The modified nail is inserted similarly (Figure 4).
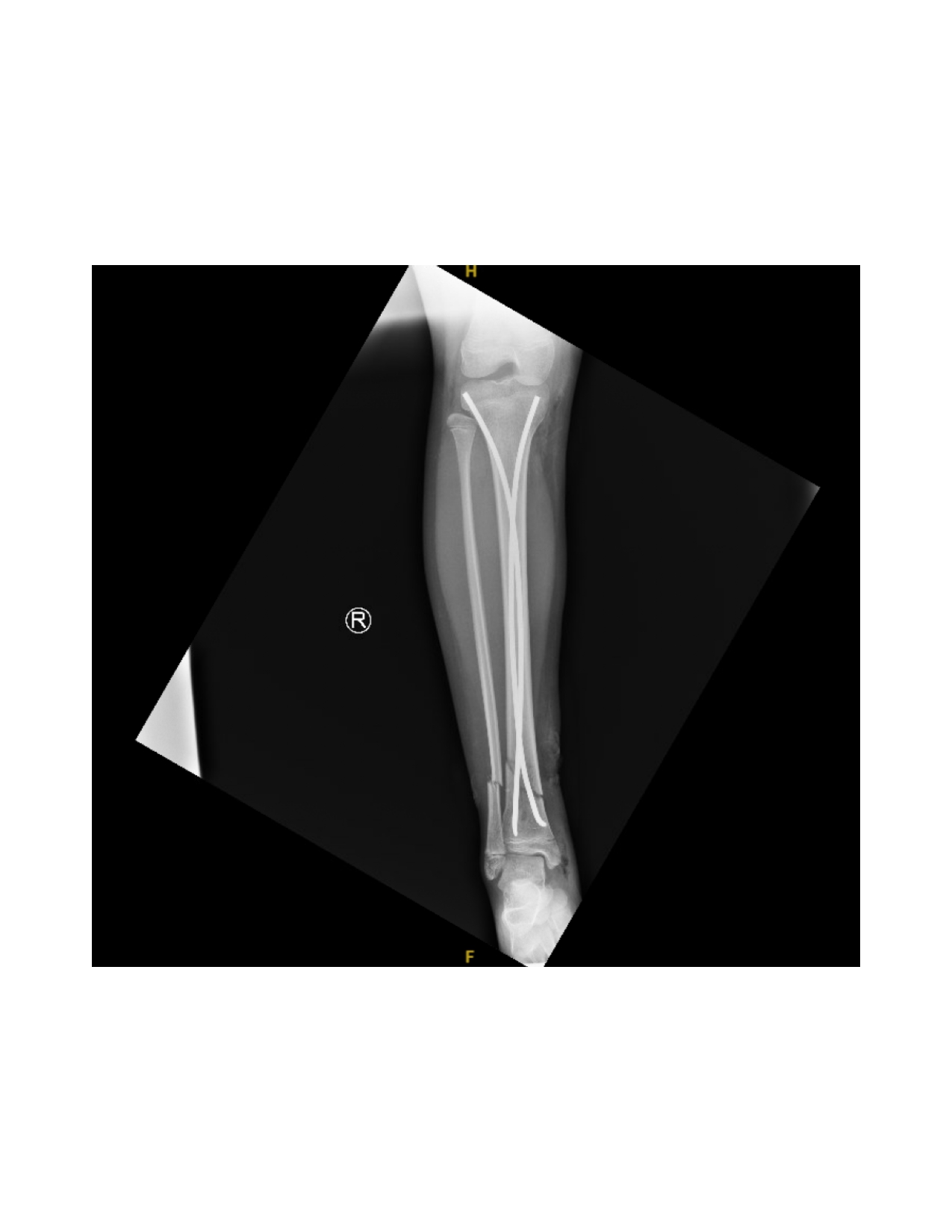
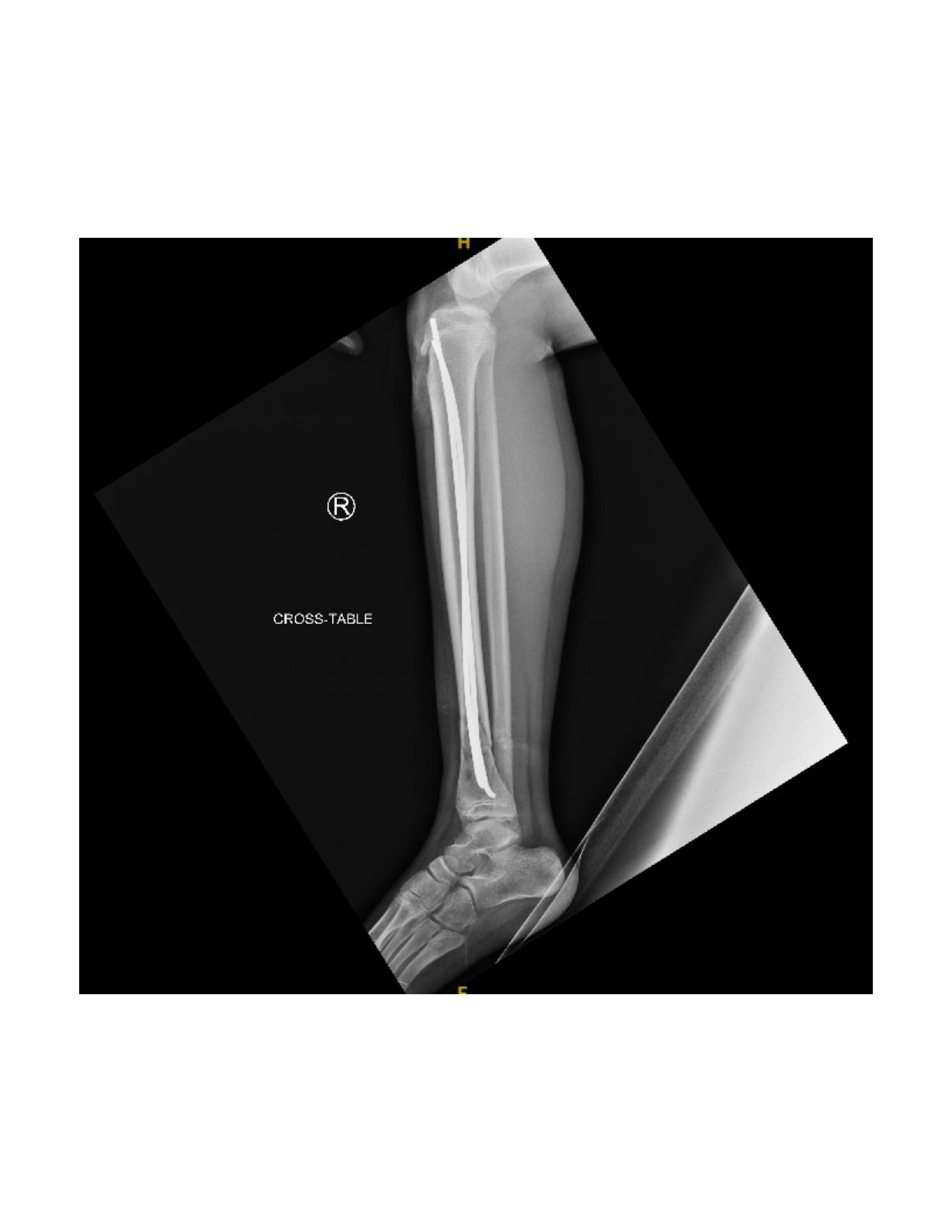
Next, the fracture is manually reduced and both nails are gently advanced past the fracture site by mallet. The curvature of the nails and their tips assists in reducing and stabilizing the fracture, inserted shy of the growth plate. Nail positioning is confirmed by fluoroscopy (Figure 5).
If displacement occurs after insertion, additional nail contouring may be necessary. To correct valgus angulation, the lateral nail can be rotated 180o medially. For procurvatum angulation, both nail tips are rotated 90o anteriorly without altering the medial and lateral orientations. For recurvatum deformity, both nail tips are directed posteriorly. Once a satisfactory reduction is achieved, the nails are hammered distally, preserving the distal physis (Figure 6).
To complete the procedure, the proximal ends of the nails are trimmed and bent into the cortex for future removal. The lateral side of the tibia has a minimized risk of postoperative skin lesions due to protective padding from overlying muscle mass allowing for a sharp bend, while the medial side bend should be less pronounced as the nail lies just beneath the skin (Figure 7).
The fracture site is then reassessed under fluoroscopy to confirm maintained reduction. (Figure 8 and Figure 9) Wounds are irrigated and closed in two layers, followed by sterile dressing and short leg splint application.
Post-operative care
Following the procedure, the leg should be elevated with active range of motion exercises encouraged. Pain management includes analgesics and/or anti-inflammatories. Adolescent patients may require DVT prophylaxis. Compartment syndrome should be monitored for changes in pain, range of motion of the ankle and great toe, and alterations in sensation. Patients should remain non-weight-bearing, using crutches for mobility. Physical therapy begins immediately without stressing the fracture site. Hospital stay duration may vary depending on individual patient, social factors, and physical therapy clearance. Patients may resume school after discharge with the ability to safely walk with crutches. Weight-bearing may begin 2-4 weeks postoperatively, with full ambulation by 2 months. Outpatient follow-up visits are recommended at 3, 6, and 12 weeks, with nail removal after fracture union is confirmed.
Comparison to Other Methods
O’Brien, et al. [8] detailed a similar flexible nailing technique where a 45° curve is added to the distal tip of the nail and a gentle curve throughout the length of the nail for fracture reduction. While our technique is similar in adding curvature up to 40° to the distal end of the nail, it specifically targets the distal third tibia, aligning the apex of the curve at the fracture site to enhance stabilization. O’Brien reported significant success with his technique in 16 unstable tibial fractures cases of various fracture locations and patterns. While his technique was not applied to distal tibial fractures, O’Brien observed an average healing time of 9 weeks with no knee pain, instability of both the knee and ankle, physical arrest, clinically significant leg length discrepancy, or remanipulation after fracture healing. This supports the role of flexible nail manipulation in facilitating fracture reductions. McGraw-Heinrich, et al. [2] compared elastic nailing and open reduction with plate fixation for pediatric distal third tibial fractures. The study found no significant differences in fracture union time, postoperative immobilization duration, time to full weight-bearing, or malunion rates. However, elastic nailing is less invasive with reduced soft tissue disruption in comparison to plate fixation.
Ramalingram, et al. [9] assessed outcomes for displaced adolescent distal third tibia fractures, comparing surgical treatments (intramedullary nails, plate and screws, flexible nails, or percutaneous wires) to nonsurgical treatment (casting without sedation or manipulation and closed reduction/casting with reduction under sedation). They found a 3.8 times higher risk of persistent misalignment in the nonsurgical group compared to the surgical treatment group. Additionally, there was a significant increase in sagittal and coronal plane alignment within the nonsurgical treatment groups. These results highlight the advantage of surgical intervention in achieving and maintaining proper alignment in complex fractures.
Benes, et al. [10] evaluated the effectiveness of elastic flexible nailing for pediatric lower extremity diametaphyseal fractures. Using the Flynn titanium elastic nails (TENs) outcome scale, 63.4% of patients with distal or proximal third shaft fractures achieved excellent results, 33.3% had satisfactory results, and only 3% experienced poor outcomes. These findings support the reliability and success of flexible nailing as a treatment option for distal third tibial fractures.
Ultimately, with a wide variety of treatment options for distal third tibial fractures, treatment selection is influenced by the surgeon’s preference, fracture characteristics and patient-specific factors. However, flexible nailing shows to be a reliable and viable option for managing these complex fractures.
Summary
While pediatric midshaft tibial fractures can tolerate slight malalignment due to remodeling potential, distal tibial fractures present a different challenge. Achieving and maintaining an optimal reduction at the distal fracture site is critical to avoid complications such as loss of reduction, malunion, and interference with the ankle joint. In cases where distal tibial shaft fractures are difficult to stabilize, adjusting the positioning and manipulation of the distal ends of flexible intramedullary nails offers a reliable technique. This approach offers a reproducible and effective solution for treating distal tibial fractures in pediatric patients, with the potential to minimize complications and improve long-term outcomes.
Disclosures
No authors have any financial disclosures.
Conflict of Interest to Disclose
No.
References
- Lascombes P (2010) Tibial fracture. In: Lascombes eds. Flexible intramedullary nailing in children. Berlin, Heidelberg: Springer 231-251.
- McGraw Heinrich JA, Ezeokoli EU, MItchell P, et al. (2022) Pediatric distal third tibial shaft fractures: A comparison of surgical fixation methods and incidence of concomitant physeal fractures. J Pediatr Orthopaedics 32: 393-400.
- Shannak AO (1988) Tibial fractures in children: Follow-up study. J Pediatr Orthopedics 8: 306-310.
- Ho CA (2016) Tibia shaft fractures in adolescents: How and when can they be managed successfully with cast treatment? J Pediatr Orthopedics 36: S15-S18.
- Cravino M, Canavese F, De Rosa V, et al. (2014) Outcome of displaced distal tibial metaphyseal fractures in children between 6 and 15 years of age treated by elastic stable intramedullary nails. Eur J Orthop Surg Traumatol 24: 1603-1608.
- Mahar AT, Lee SS, Lalonde FD, et al. (2004) Biomechanical comparison of stainless steel and titanium nails for fixation of simulated femoral fractures. J Pediatr Orthopedics 24: 638-641.
- Frumberg DB, Van Lanen Wanek DJ, Jauregui JJ, et al. (2018) Can flexible intramedullary nails provide proper fixation of long bone fractures in patients weighing over 100 pounds? J Orthopaedics Trauma and Rehabilitation 26: 13-19.
- O'Brien T, Weisman DS, Ronchetti, P, et al. (2004) Flexible titanium nailing for the treatment of the unstable pediatric tibial fracture. J Pediatr Orthopedics 24: 601-609.
- Ramalingam W, Carry P, Brazell C, et al. (2022) Outcomes of displaced adolescent distal third tibia fractures: Can we do better? J Pediatr Orthopedics 31: e147-e153.
- Benes G, Schmerler J, Harris AB, et al. (2024) Flexible nailing: Pushing the indications for diametaphyseal lower-extremity fractures. Medicine 103: e37417.
Corresponding Author
Judy-Mae Lima, Department of Orthopaedic Surgery, Rutgers New Jersey Medical School, 185 S Orange Ave, Newark, New Jersey, 07103, USA.
Copyright
© 2025 Lima JM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.