Reconstruction of the Tibialis Posterior Flexor Retinaculum: Description of Surgical Technique
Abstract
Dislocation of the tibialis posterior tendon is a rare traumatic injury often with a delayed diagnosis. The surgical management of the majority of these injuries is reconstruction of the flexor retinaculum. Non-operative management or missed diagnosis of these injuries leads to chronic pain, posterior tibialis tendon insufficiency, and acquired flat foot deformity. Reconstruction of the flexor retinaculum is not well characterized in the orthopedic literature. The technique described here was used to reconstruct the flexor retinaculum in the setting of an acute tibialis posterior dislocation. The case presented here was a collegiate gymnast with an acute ankle injury while dismounting.
Introduction
Acute dislocation of the tibialis posterior tendon is a rare injury that is poorly characterized in Western literature. These injuries often have a delayed diagnosis due to their rarity and treating clinicians’ unfamiliarity with their presentation and can be misdiagnosed as a sprain in certain settings [1]. The tibialis posterior plays a significant role in plantar flexion and inversion of the foot. The tendon of the tibialis posterior courses behind the medial malleolus in the retromalleolar groove. The flexor retinaculum helps to keep the tendon within the groove as it acutely changes direction towards its insertion in the midfoot. Significant variations in the depth and width of the retromalleolar groove may predispose to dislocation of the posterior tibialis tendon [2,3]. Support can be seen in research that shows evidence that the variations in groove morphology may result in tendon degeneration and impaired healing [4].
The etiology of posterior tibialis tendon dislocation is an inversion and dorsiflexion injury that causes disruption of the flexor retinaculum. Management of this injury can be conservative or operative. Operative management includes repair of the flexor retinaculum or reconstruction, and retromalleolar groove deepening with flexor retinaculum repair or reconstruction [2,3].
Case Presentation, Examination, and Imaging
The case presented here is that of a 20-year-old collegiate gymnast who reported a twisting injury to the left ankle while dismounting. The patient presented three days later with left ankle pain and difficulty with ambulation. On exam, the patient had pain over the posterior medial malleolus and posterior tibialis tendon. The patient also had weakness with eversion and inversion of the ankle. Plain radiographs obtained at the time were unremarkable. An MRI demonstrated partial tearing of the posterior tibialis tendon and medial subluxation of the tendon with a high-grade tear of the flexor retinaculum. Additional findings on the MRI were partial tearing of the superficial and deep deltoid ligament fibers, high-grade tearing of the anterior tibiofibular ligament, and bone contusion of the talus. The decision was made to proceed with flexor retinaculum repair fourteen days after the initial injury.
Surgical Approach and Retinaculum Reconstruction
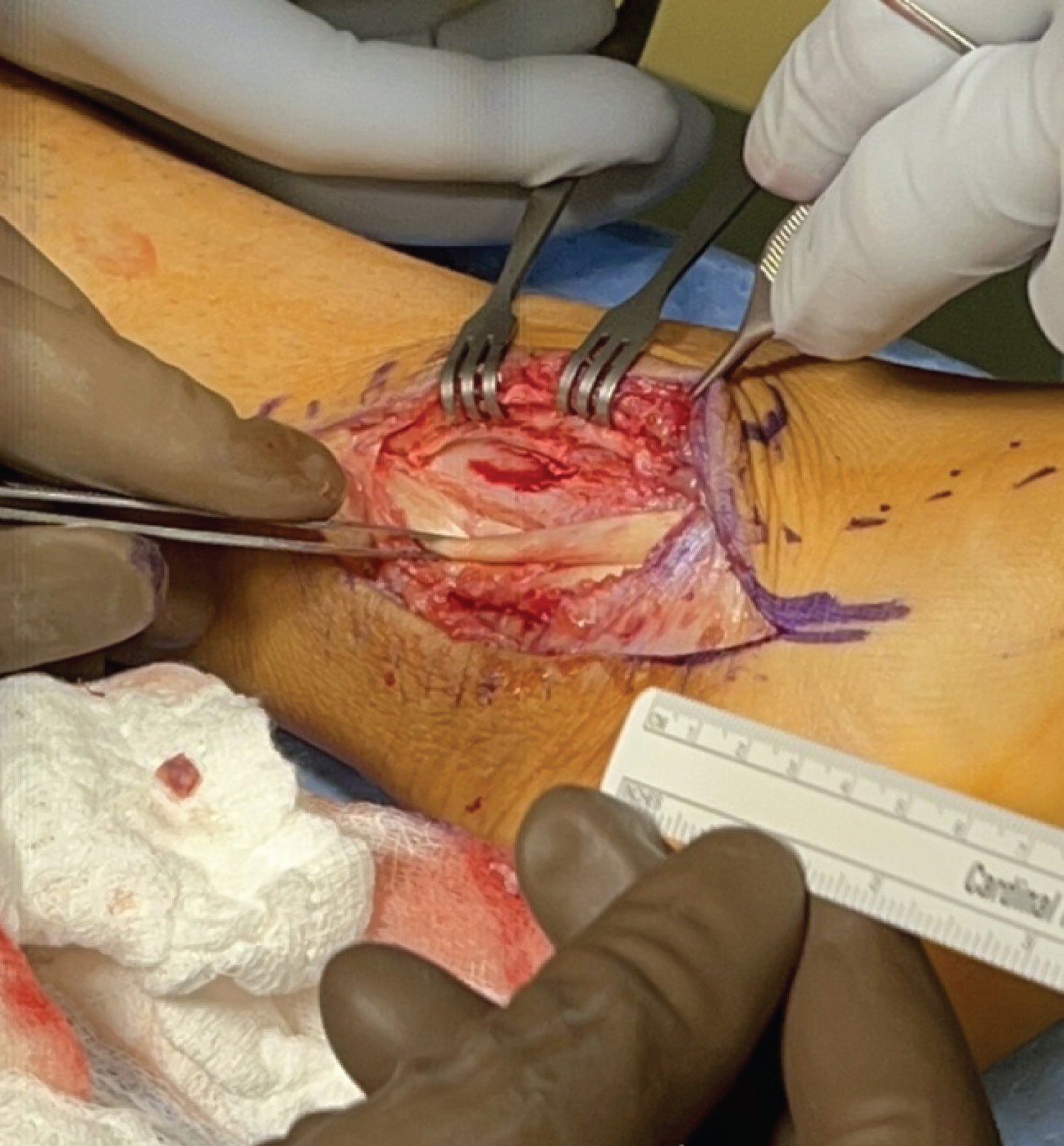
The patient had a regional block performed pre-operatively. He was supine on the operating table with a tourniquet placed on the operative thigh. Intraoperative fluoroscopy was performed to evaluate for medial ankle stability and was found to be stable. A single vertical incision was made over the posterior distal third of the medial malleolus and distal tibia. Dissection was carried down to the superficial retinaculum. Full-thickness anterior and posterior superficial flaps of the retinaculum were made. At this time a defect was palpated in the deep retinaculum through which the posterior tibialis tendon was dislocating anteriorly. The deep retinacular layer was further dissected to reveal the defect’s full extent and to free up anterior and posterior flaps. The remaining anterior retinacular tissue was elevated off the tibia to increase the excursion of the flap (Figure 1).
Six 1.8 mm Q fix anchors were placed in the medial malleolus and distal tibia anterior to the retromalleolar groove (Figure 2).
The two most distal suture anchors were passed through the distal part of the flexor retinaculum. The two proximal suture anchors were passed through the most proximal part of the retinacular flap. The posterior tibialis tendon was then reduced into the retromalleolar groove. 2-0 FiberWires were then placed in a pants-over-vest fashion to help close the remnant of the deep retinacular layer. An additional 4 pairs of independent sutures were passed to close down the remaining central defect in the deep retinaculum. The distal suture anchor sutures were then tied down followed by the proximal suture anchor sutures. The central suture anchors were then passed through the remnants of the elevated deep retinacular tissue and tied down to complete the repair (Figure 3). The wound was then irrigated and closed. The patient was placed in a short leg splint to stay on until his first follow-up.
Post-Operative Rehab
After surgery, the patient was non-weight-bearing in a short leg splint. The patient was transitioned from a splint to a short leg cast at his first post-operative visit two weeks after surgery. He remained non-weight-bearing for the first 4 weeks postoperatively. The patient was transitioned from a cast to a CAM boot four weeks after surgery and started progressive, but limited weight bearing. At four months postoperatively, the patient was started on light exercise including stationary bike, but no landing or impact exercises. At five months postoperatively, the patient started running and starting landing exercises from a pommel horse, but not vault landings.
Discussion
Tibialis posterior tendon dislocation is a rare injury. Surgical management of these injuries is typically recommended to prevent tibialis posterior tendon insufficiency, arch collapse, and subsequent flat foot deformity. Lohrer, et al. published a systematic review of posterior tibial tendon dislocations that included 61 published cases making this case more common than previously thought [5]. Fifty-eight percent of these were sports-related injuries. Fifty-three percent of these cases were initially misdiagnosed. Surgery was performed on 83% of these patients. The techniques used varied from case to case. The review found that 80% of patients had excellent or asymptomatic results with surgical treatment of these injuries.
There is no consensus regarding the optimal surgical management of these injuries. Several techniques have been described including retinacular repair or reconstruction, and retromalleolar groove deepening. Additionally, there is no consensus regarding the optimal timing of surgical management of these issues which is confounded by the often delayed diagnosis. Thorough physical examination and MRI are critical in identifying subluxation or dislocation of the peroneal tendon. MRI is also critical in identifying tears of the tibialis posterior tendon and other concomitant medial ankle pathology.
In this case report, we present a novel technique to reconstruct the flexor retinaculum using suture anchors. This technique prevents the morbidity associated with retromalleolar groove deepening. The repair used suture anchors passed through the remnant retinaculum in a mattress fashion to strengthen the repair. At six months postoperatively, the patient had returned to collegiate athletics.
References
- Alamri WM, Aljeaan R, Almulhim AK, Saleh H (2020) Traumatic dislocation of tibialis posterior tendon: A case report and literature review. Cureus 12: e10885.
- Gkoudina A, Graikos G, Chatziargiriou M, Saloupis P (2021) Posterior tibialis tendon dislocation: Case report and review of literature. Cureus 13: e19301.
- Goucher NR, Coughlin MJ, Kristensen RM (2006) Dislocation of the posterior tibial tendon: A literature review and presentation of two cases. Iowa Orthop J 26: 122-126.
- Oddy MJ, Choraria A, Campbell A, Ali A, Rajesparan K (2023) Tibial retro-malleolar groove morphology in patients with posterior tibialis tendon dysfunction. J Foot Ankle Surg 62: 888-892.
- Lohrer H, Nauck T (2010) Posterior tibial tendon dislocation: A systematic review of the literature and presentation of a case. Br J Sports Med 44: 398-406.
Corresponding Author
Matthew H Adsit, MD, Department of Orthopedic Surgery, Virginia Commonwealth University, 1200 E. Broad Street, 9th Floor, Box 980153, Richmond, VA 23298-0153, USA.
Copyright
© 2023 Adsit MH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.