Short Segment vs. Long Segment Posterior Spinal Fixation of Unstable Thoracolumbar Burst Fractures: A Retrospective Cohort Study
Abstract
Background: Fractures of the thoracolumbar (TL) vertebrae are common. Optimal surgical management aims to enhance movement and provide long-term stability. Short segment posterior spinal fixation (SSPSF) provides better movement, has less economic burden, but superiority over long segment posterior spinal fixation (LSPSF) remains uncertain. The aim of this study was to report the difference between SSPSF versus LSPSF with regards to loss of correction measured with Cobb's angle in patients with single level unstable burst TL vertebral fractures.
Methods: This was a retrospective cohort study including patients who presented between August 2012 to July 2015 at King Saud Medical City, Saudi Arabia- a level I trauma centre. Cobb's angles were measured by two independent assessors immediately post-operative and at one-year follow up. The differences in Cobb's angles were compared for all included patients, and in subgroups of patients that underwent fusion and in the subgroup of patients that underwent LSPSF only.
Results: There were 39 patients included with a burst type fracture and completed 1-year follow-up. Ten patients underwent SSPSF and 29 underwent LSPSF. The mean age was 35 (SD 15.7) years, the most common mechanism of injury was a motor vehicle crash (32; 85.1%) and the L1 (20; 51.3%) was the most commonly injured vertebra. Among patients who underwent SSPSF, Cobb's angles were significantly higher immediately post-surgery (9.0 vs. 0.35 degrees; p < 0.001) and at 1-year after surgery (16.5 vs. 3.46 degrees; p < 0.001). Change in Cobb's angle at 1-year follow-up was 7.5 (SD 3.6) degrees among SSPSF group, compared to 3.1 (SD 4.8) degrees in the LSPSF group (p < 0.001). The differences persisted when patients who underwent SSPF were compared to those that underwent LSPSF without fusion. Among patients who underwent LSPSF, no differences were observed between those who underwent fusion versus those that did not.
Conclusion: LSPSF appeared superior to SSPSF for maintaining Cobb's angle at 1-year post-surgery. Further research on parameters describing clinical and patient reported outcomes following different fixation modalities are needed to determine the most appropriate surgical technique.
Keywords
Wounds and injuries, Thoracolumbar spine, Posterior spinal fixation, Spinal fusion
Introduction
Traumatic vertebral injuries are major causes of morbidity in Saudi Arabia with the leading mechanism being motor vehicle collisions (MVC) [1,2]. The thoracolumbar (TL) junction (T11-L2) is the most commonly injured segment in the vertebral column as it is subjected to biomechanical stresses linked to its location in a transitional zone between a relatively rigid thoracic spine that is connected with the rib cage and the more mobile and dynamic lumbar spine [3,4]. The first lumbar vertebra (L1) is the most commonly injured and a burst type injury is the most common morphology [5].
Several classification systems are available in literature for vertebral fractures [6,7]. Burst fractures are a result of failure of anterior and middle columns and considered either AO type 3 (incomplete) or AO type 4 (complete) [6]. McAfee, et al. classified burst fractures to a stable form- where the posterior column is intact and can be treated conservatively, and an unstable form; where the posterior column is disrupted and surgical treatment is necessary [7]. Integrity of the posterior ligamentous complex (PLC) is crucial for spinal stability and when disrupted, deformity and failure of conservative treatment can occur, which can be assessed by short-tau inversion-recovery (STIR) sequences on MRI in the acute setting following injury [8].
There exists controversy regarding the indications for surgical treatment. Apart from neurological injury being an absolute indication for surgery, some of the other commonly used indications are more than 20° to 30° angle of kyphotic deformity, more than 50% loss of vertebral body height, and more than 40% to 50% canal narrowing [9]. Among patients managed surgically, preservation of motion segments is a basic principle in spinal surgery for the management of burst fractures [10,11]. Short segment fixation (one vertebra above and one below) was found to be successful in some studies in order to preserve more motion that can be decreased with longer segments fixation with no difference in outcome and with less cost, and intra-operative bleeding [12-15]. Other studies showed that long segment instrumentation has more favourable outcomes compared to short segment fusion in terms of radiographic and clinical outcomes [16,17].
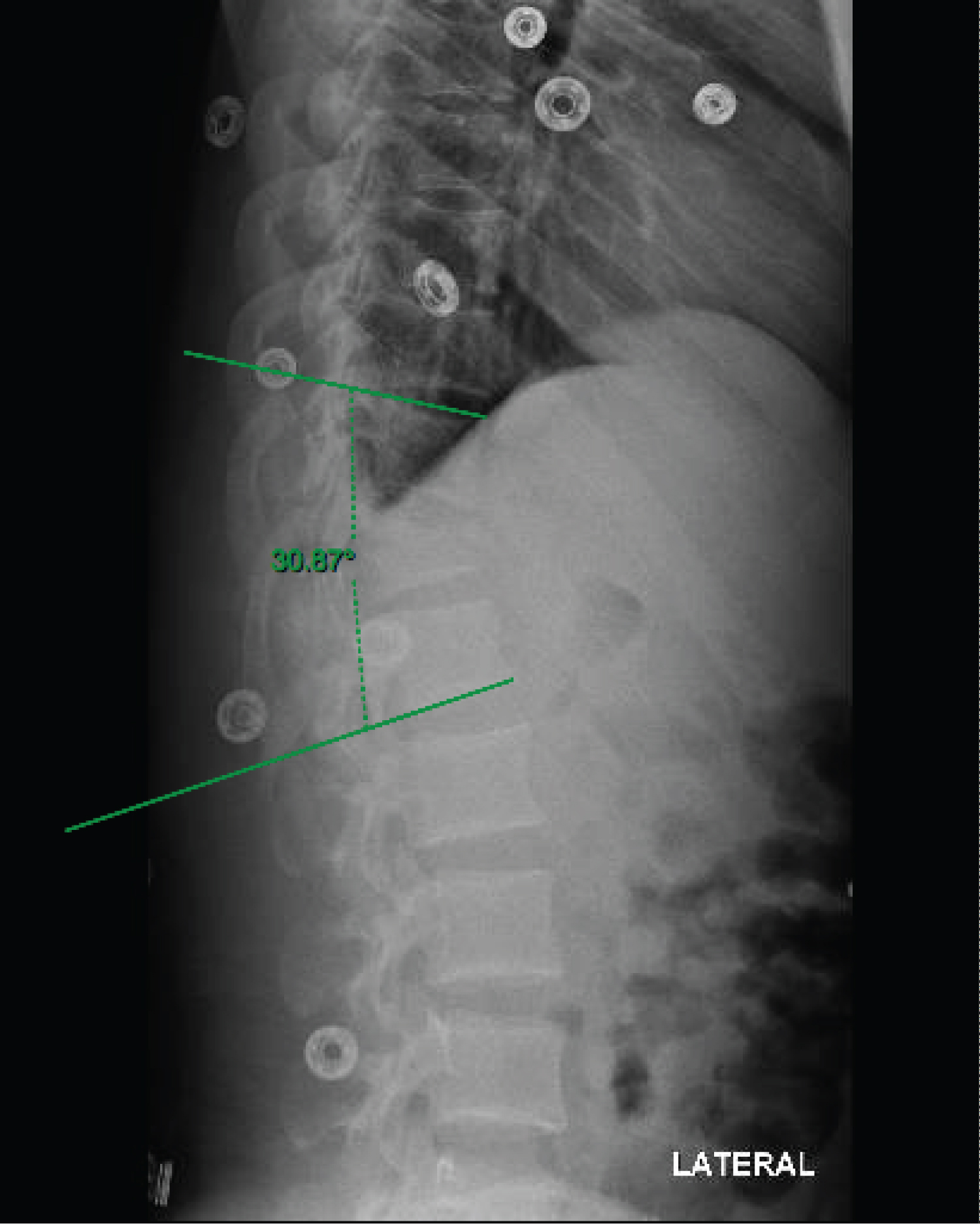
Post-operative Cobb's angle is a useful indicator of satisfactory alignment [18]. Measuring the Cobb's angle from the upper end plate of the vertebra above the fractured level and lower end plate of vertebra below has good inter observer agreement (Figure 1) [19]. The aim of this study was to assess the standing radiographic outcome measurement using sagittal Cobb's angle in patients with thoracolumbar burst fracture AO type A3 and A4 treated with a short segment posterior spinal fixation (SSPSF) compared to long segment posterior spinal fixation (LSPSF).
Materials and Methods
This was a retrospective cohort study conducted among patients who presented during the period from August 2012 to July 2015 at King Saud Medical City (KSMC). KSMC is a major trauma centre and a tertiary centre in the capital of Saudi Arabia, Riyadh. It provides emergency healthcare to all individuals with no exception and has the largest orthopaedic department in Saudi Arabia with regards to bed capacity.
Patients
The inclusion criteria were: (1) Adult patients with a (2) Single level unstable thoracolumbar junction burst fractures involving T11-L2 segment (3) Treated with short segment transpedicular posterior spinal fixation or long segment transpedicular posterior spinal fixation. Short segment posterior spinal fixation (SSPSF) is defined as transpedicular fixation that involves one vertebra above and one vertebra below. Long segment posterior spinal fixation (LSPSF) is defined as fixation that involves two vertebras above and two vertebras below the fracture. Unstable burst fracture is defined as AO type A3 or Type A4 [6] with associated PLC injury, decrease in vertebral height of more than 50%, canal narrowing more than 50%, neurological involvement, or sagittal junctional Cobb's angle of more than 20 degrees. Excluded cases were patients who had fragility low mechanism of injury burst fractures, documented to have osteopenia or osteoporosis, patients with adjacent spinal injuries and those who had departed Saudi Arabia within one year of surgery.
Data Collection and Statistical Analysis
Data were extracted using an explicit chart review and included age in years as a continuous variable, sex as a binary variable, mechanism of injury, level and type of fracture. The Cobb's angle in degrees on standing lateral X-ray was calculated using immediate post-operative and one-year follow-up as a continuous variable. The Cobb's angle was measured by the method of measuring the angle from the upper endplate of the vertebra above and the lower endplate of the vertebra below the fracture site (Figure 1). It was measured by 2 independent reviewers and inter-rater agreement reported using weighted kappa scores (with 95% confidence intervals) and p-values calculated using Pitman's test of difference in variance. The mean of the measurements of the two assessors was reported for each patient. Outcome measures were the difference, and change in sagittal Cobb's angle immediately post-operatively, and at one-year follow-up between the SSPSF and LSPSF groups. In addition, we compared immediately post-operative and one-year Cobb's angles for the subgroups of (1) Patients who underwent LSPSF without fusion to those with fusion and (2) Patients who underwent LSPSF without fusion to SSPSF.
The outcome variables were assessed using the difference between the two means. Statistical significance between two means was assessed using Student's t-test. All statistical analyses were conducted using SAS® University Edition software (version 9; SAS institute, Inc, Cary, NC). A p-value of < 0.05 was defined as statistically significant. The study was reviewed and approved by the KSMC central institutional review board (Project reference H1RI-13-Dec17-01).
Results
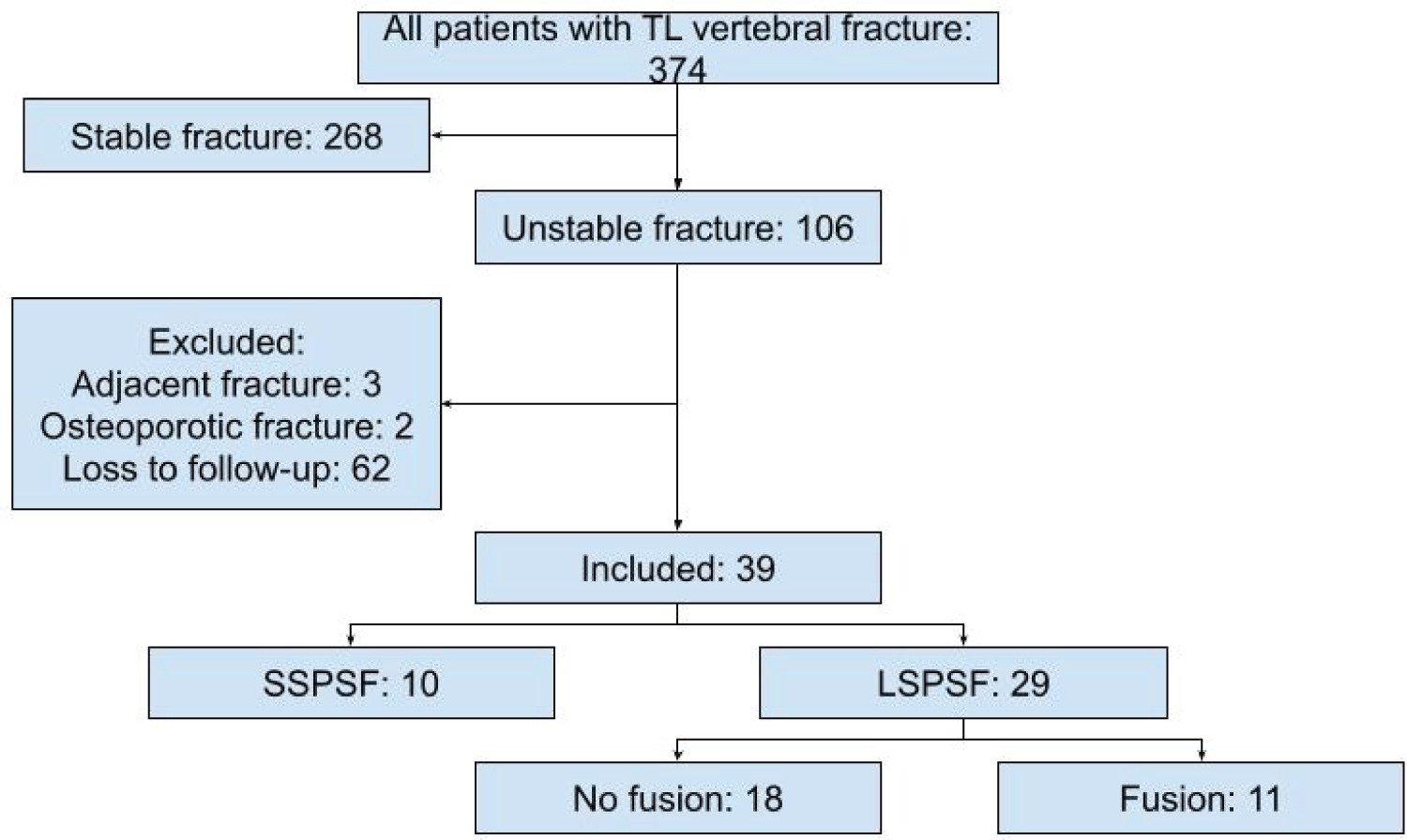
Total of 374 adult patients with TL fractures were identified. Of these, 106 (28.3%) had unstable burst TL fracture, three patients were excluded for having an adjacent vertebral fracture and two patients were excluded for having osteoporotic fractures. Sixty-two patients did not have data on one-year follow-up as they were expatriate workers who returned to home countries after treatment. There were 39 patients with single level unstable thoracolumbar burst fractures who underwent posterior spinal fixation and fulfilled the inclusion criteria. The average age of included patients was 35 (SD 15.7) years, and most (n = 29) were male. Of the total cohort, 10 patients underwent short segment posterior spinal fixation (SSPSF) and 29 patients underwent long segment posterior spinal fixation (LSPSF). There were 21 AO type A4 fractures of all patients, 17 (80.95%) underwent LSPSF, 4 (19.05%) underwent SSPSF. There were 18 AO type A3 fractures of all cases, 12 (66.67%) underwent LSPSF, 6 (33.33%) cases underwent SSPSF (Table 1 and Figure 2).
Assessment of post-operative Cobb's angles had substantial inter-rater agreement with Cohen's kappa of 0.69 (95% CI: 0.58-0.80) and Pitman's test of difference in variance p = 0.19. Assessment of Cobb's angles at 1 year post surgery also had substantial inter-rater agreement with Cohen's kappa of 0.78 (95% CI: 0.71-0.85) and Pitman's test of difference in variance p = 0.76. The mean Cobb's angle immediately post-operatively of patients who underwent SSPSF was 9.00 (SD: 4.81) degrees, compared to 0.35 (SD: 6.88) degrees in patients who underwent LSPSF with a statistically significant difference (p < 0.001). At one-year post surgery, the mean Cobb's angle was 16.5 (SD: 5.63) degrees after SSPSF and 3.46 (SD: 8.01) degrees after LSPSF with a statistically significant difference (p < 0.001). The average Change of Cobb's angle between patients who underwent SSPSF and LSPSF was 7.5 (SD 3.64) degrees and 3.11 (SD 4.77) degrees respectively (p < 0.001; Table 2).
Out of all cases, 28 (71.8%) underwent posterior spinal fixation without fusion and the rest underwent fusion. Of LSPSF cases, 18 (62.1%) underwent fixation without fusion while all SSPSF cases did not undergo fusion. When we compared LSPSF without fusion, SSPSF cases had higher immediate and 1-year post-operative Cobb's angle, and a greater in Cobb's angle from post-operative values (p < 0.001; Table 2).
When the 18 LSPSF cases (62.1%) who did not undergo fusion were compared to the 11 LSPSF cases (37.9%) who underwent fusion, there were no statistically significant difference in terms of immediate and 1-year post-operative Cobb's angle or change in Cobb's angle between the immediate and 1-year post-operative Cobb's angles (Table 2).
Discussion
In this single centre study from the largest trauma centre in Saudi Arabia, post-operative sagittal Cobb's angles were significantly different between patients who underwent LSPSF compared to SSPSF. Cobb's angles were higher after SSPF at both immediately post operative and at one-year. In addition, the increase in Cobb's angle was higher for patients who underwent SSPSF compared to those that underwent LSPSF. These fundings were consistent when comparing patients who underwent SPSF with those undergoing LSPSF without fusion. Among patients undergoing LSPSF, there were no differences associated with fusion. These results question the equiveillance of SSPSF to LSPSF as reported in some studies and mandates further research towards the choice of surgical technique in unstable burst fractures.
Several studies focusing on the outcome of short segment instrumentation compared with long segment instrumentation were done with variable and conflicting results [12-17]. Our findings were consistent with the results of Waqar, et al. who concluded that long segment fixation had better radiographic Cobb's angle post operatively compared to short segment fixation but they found no statistical significance difference (p = 0.068) [17]. Similarly, Sapakas, et al. found a statistical significant difference when comparing SSPSF to LSPSF in terms of follow up Cobb's angle with favourable measures found in LSPSF group [16]. Panteliadis, et al. compared three modalities for posterior spinal fixation in thoracolumbar burst fractures (1 level above and 1 level below, 2 above and 1 below, and 2 above and 2 below the fracture) and found that better correction maintained in the 2 above and 2 below group compared to the others but with no statistically significant difference [20].
The high loss of correction in the SSPSF group over the 1-year followup was consistent with fiundings of Gelb, et al. who conluded that the the average loss of correction following short segment fixation was similar at 7.5 degrees and advocated for fracture level instrumentation for better correction [12]. However, in a meta-analysis of studies, Aly found no statistically significant differences when short segment fixation compared with long segment fixation regarding the post-operative Cobb's angle but advocated for more randomised controlled trials on the topic [14]. Basaran, et al. also found short segment fixation is suffecient to stabilize spinal fractures with the fractured vertebra included in the fixation [15]. Similarly, Dobran, et al. found no statistically significant difference when he compared short segment with fracture level included with long segment fixation sparing the fracture site in term of correction loss, but the average loss of correction was considerably higher than reported in our study [21]. Su, et al. found that the highest stress concentration was in the posterior third of the vertebral body just anterior to spinal canal in flexion and extension in the thoracolumbar area [22].
Included patients in this study were all type AO type A3, or A4 and could explain the high sagittal Cobb's angle with SSPSF compared LSPSF, with SSPSF being not sufficient enough to maintain the sagittal alignment. Some studies highlighted the importance of augmenting the fractured vertebra with polymethyl methacrylate (PMMA) in adjunct with short segment fixation which resulted in good outcomes in terms of anterior vertebral body height and maintaining of kyphotic angle [23,24]. The previously mentioned studies' data that compared SSPSF to LSPSF were heterogenous with some of the cases had less degree of vertebral body involvement as in anterior wedge fracture or distraction injuries compared to burst injuries [12,14,17]. Kallemeier, et al. studied range of motion of simulated unstable burst fracture on spine models and found that posterior spinal fixation alone resulted in less range of motion in flexion compared to an intact spine with statistically significant difference (p < 0.05), contrary to what was found when they compared anterior corpectomy and strut grafting alone to normal spine models (p = 0.1). They also found that increased ROM was correlated with greater fracture comminution for posterior-only fixation (p < 0.05) [25]. This could explain the importance of vertebral body degree of involvement regarding the stability of posterior spinal fixation and explain the reason why we found that LSPSF had more favorable radiographic parameters than SSPSF.
Mina, et al. found that the stiffest construct found in their models where they simulated unstable burst fractures was LSPSF and it provided well distributed stress to the implant while lowering the intervertebral disc stress at the fixed segment [26]. In our study, cases who underwent fusion were all within LSPSF group only, and when they were compared to the LSPSF cases that did not undergo fusion, there were no statistically significant difference as found in multiple studies [9,27-29]. We believe that LSPSF in AO type A3 or A4 has better radiographic outcome compared to SSPF due to the highly compromised vertebral body injury making SSPSF not reliable in maintaining sagittal Cobb's angle on standing films.
There are several limitations in the study being the retrospective design, lack of detailed documentation resulting in exclusion of patients, and loss of follow up found in some cases that caused the relatively small sample size. Future studies should focus on larger sample size, and with SSPSF continuing to be sued, there appears equipoise for randomization to generate a higher level of evidence towards the best operative technique for TL vertebral fractures.
Conclusion
In this cohort study of surgically managed TL vertebral fractures, LSPSF appeared superior to SSPSF in terms of maintaining Cobb's angle at 1-year post-operatively. This difference persisted when patients who underwent fusion were excluded. Future studies should be aimed to evaluate the radiographic and clinical outcomes following fixations modalities with extended follow up.
Statements
Statement of ethics
This study protocol was reviewed and approved by the King Saud Medical City institutional review board (Project reference H1RI-13-Dec17-01).
Consent to participate statement
The requirement to seek informed consent from participants was waived by the ethics committee.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Funding sources
The study was facilitated by the King Saud Medical City (KSMC) - The Alfred International Trauma Program.
Author contributions
Bandar Alrashedan: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Software, Writing-original draft, Writing-review & editing; Mohammad Alawad: Conceptualization, Data curation, Formal analysis, Methodology, Resources, Writing-original draft; Mohammed Alsabieh: Formal analysis, Methodology, Resources, Writing-original draft, Writing-review & editing; Nasser Alenezi: Conceptualization, Data curation, Formal analysis, Investigation, Resources; Saad Surur: Conceptualization, Methodology, Supervision, Validation, Visualization; Biswadev Mitra: Conceptualization, Formal analysis, Supervision, Validation, Visualization.
Data availability statement
Due to the nature of this research, consent was not sought from participants of this study for their data to be shared publicly, so supporting data is not available.
References
- Al Jadid MS (2013) A retrospective study on traumatic spinal cord injury in an inpatient rehabilitation unit in central Saudi Arabia. Saudi Med J 34: 161-165.
- Alawad MO, Alenezi N, Alrashedan BS, et al. (2020) Traumatic spinal injuries in Saudi Arabia: A retrospective single-centre medical record review. BMJ Open 10: e039768.
- Wood KB, Li W, Lebl DS, et al. (2014) Management of thoracolumbar spine fractures. Spine J 14: 145-164.
- El Khoury GY, Whitten CG (1993) Trauma to the upper thoracic spine: Anatomy, biomechanics, and unique imaging features. AJR Am J Roentgenol 160: 95-102.
- Katsuura Y, Osborn JM, Cason GW (2016) The epidemiology of thoracolumbar trauma: A meta-analysis. J Orthop 13: 383-388.
- (2020) AO Spine injury classification systems.
- McAfee PC, Yuan HA, Fredrickson BE, et al. (1983) The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Am 65: 461-473.
- Shen J, Xu L, Zhang B, et al. (2015) Risk factors for the failure of spinal burst fractures treated conservatively according to the thoracolumbar injury classification and severity score (TLICS): A retrospective. PLoS ONE 10: e0135735.
- Hwang JU, Hur JW, Lee JW, et al. (2012) Comparison of posterior fixation alone and supplementation with posterolateral fusion in thoracolumbar burst fractures. J Korean Neurosurg Soc 52: 346-352.
- Yurac R, Marré B, Urzua A, et al. (2006) Residual mobility of instrumented and non-fused segments in thoracolumbar spine fractures. Eur Spine J 15: 864-875.
- Wei FX, Liu SY, Liang CX, et al. (2010) Transpedicular fixation in management of thoracolumbar burst fractures: Monosegmental fixation versus short-segment instrumentation. Spine 35: E714-E720.
- Gelb D, Ludwig S, Karp JE, et al. (2010) Successful treatment of thoracolumbar fractures with short-segment pedicle instrumentation. J Spinal Disord Tech 23: 293-301.
- Parker JW, Lane JR, Karaikovic EE, et al. (2000) Successful short-segment instrumentation and fusion for thoracolumbar spine fractures: A consecutive 4 1/2 -year series. Spine 25: 1157-1170.
- Aly TA (2017) Short segment versus long segment pedicle screws fixation in management of thoracolumbar burst fractures: Meta-analysis. Asian Spine J 11: 150-160.
- Basaran R, Efendioglu M, Kaksi M, et al. (2019) Finite element analysis of short- versus long-segment posterior fixation for thoracolumbar burst fracture. World Neurosurg 128: e1109-e1117.
- Sapkas G, Kateros K, Papadakis SA, et al. (2010) Treatment of unstable thoracolumbar burst fractures by indirect reduction and posterior stabilization: short-segment versus long-segment stabilization. Open Orthop J 4: 7-13.
- Waqar M, Van Popta D, Barone DG, et al. (2017) Short versus long-segment posterior fixation in the treatment of thoracolumbar junction fractures: A comparison of outcomes. Br J Neurosurg 31: 54-57.
- Cobb J (1948) Outline for the study of scoliosis. Instr Course Lect AAOS 5: 261-275.
- Kuklo TR, Polly DW, Owens BD, et al. (2001) Measurement of thoracic and lumbar fracture kyphosis: Evaluation of intraobserver, interobserver, and technique variability. Spine 26: 61-65.
- Panteliadis P, Musbahi O, Muthian S, et al. (2018) A comparison of three different methods of fixation in the management of thoracolumbar fractures. Int J Spine Surg 12: 1-7.
- Dobran M, Nasi D, Brunozzi D, et al. (2016) Treatment of unstable thoracolumbar junction fractures: Short-segment pedicle fixation with inclusion of the fracture level versus long-segment instrumentation. Acta Neurochir 158: 1883-1889.
- Su Q, Li C, Li Y, et al. (2020) Analysis and improvement of the three-column spinal theory. BMC Musculoskelet Disord 21: 537.
- Cho DY, Lee WY, Sheu PC, et al. (2003) Treatment of thoracolumbar burst fractures with polymethyl methacrylate vertebroplasty and short-segment pedicle screw fixation. Neurosurgery 53: 1354-1360.
- Acosta FL, Aryan HE, Taylor WR, et al. (2005) Kyphoplasty-augmented short-segment pedicle screw fixation of traumatic lumbar burst fractures: Initial clinical experience and literature review. Neurosurg Focus 18: e9.
- Kallemeier PM, Beaubien BP, Buttermann GR, et al. (2008) In vitro analysis of anterior and posterior fixation in an experimental unstable burst fracture model. J Spinal Disord Tech 21: 216-224.
- Alizadeh M, Abdul Kadir MR (2018) Biomechanical evaluation of segmental pedicle screw fixation in thoracolumbar fracture: a finite element study. Orthopedics and Rheumatology Open Access Journal 12.
- Dai LY, Jiang LS, Jiang SD (2009) Posterior short-segment fixation with or without fusion for thoracolumbar burst fractures: A five to seven-year prospective randomized study. J Bone Joint Surg Am 91: 1033-1041.
- Jindal N, Sankhala SS, Bachhal V (2012) The role of fusion in the management of burst fractures of the thoracolumbar spine treated by short segment pedicle screw fixation: A prospective randomised trial. J Bone Joint Surg Br 94: 1126-1134.
- Chou PH, Ma HL, Wang ST, et al. (2014) Fusion may not be a necessary procedure for surgically treated burst fractures of the thoracolumbar and lumbar spines. J Bone Joint Surg Am 96: 1724-1731.
Corresponding Author
Biswadev Mitra, School of Public Health & Preventive Medicine, Monash University, 553 St. Kilda Rd, Melbourne, Victoria 3004, Australia, Tel: +61-39076-2699
Copyright
© 2022 Alrashedan BS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.