Possible Technical Advantages of Single-Portal Knee Arthroscopy
Abstract
Purpose: In knee arthroscopy, two portals were traditionally used to perform surgery. In the last decade, the novel technique of single-portal knee arthroscopy has been investigated with promising results. This randomized control trial comparing single-portal to double-portal knee arthroscopy reports surgical time as the primary outcome. Secondly, post-operative knee function for up to 12 months is measured using a validated questionnaire. Third, post-operative pain scores and medication use are also reported.
Methods: All participants were selected from the Orthopaedic Sports Medicine Clinic's patient population. Participants were assigned to either Group 1 (single-portal; experimental) or Group 2 (two-portal; control) using a block randomization scheme (block size of 10). The same surgeon (J.H.) performed all surgeries. For the single-portal technique, a Parallel Portal Cannula (Stryker Endoscopy) was utilized. Surgical time was recorded and compared between groups. International Knee Documentation Committee (IKDC) forms were used pre-operatively to gather patient information. At 1, 3, 6, and 12 months post-operatively, IKDC forms were used to measure knee function. On the first and fourth day post-operatively, patients reported their pain score and medication use by telephone. In the first 14 days post-operatively, patients also maintained a log of daily pain scores and medication use.
Results: Pre-operative physical function differed significantly between the two groups. Average surgical time for single-portal knee arthroscopy was not statistically different when compared to double-portal knee arthroscopy. No patients required conversion from single-portal to double-portal technique. IKDC knee function increased over 12 months postoperatively for all patients but did not differ between the two treatment groups. Self-reported pain scores, overall medication use, and narcotic medication use decreased significantly postoperatively for all patients but did not differ between the two treatment groups. Adjusting for pre-operative physical function did not alter the results.
Conclusion: Single-portal knee arthroscopy has possible technical advantages for meniscus and articular cartilage pathology that requires minimal surgical instrumentation.
Keywords
Knee arthroscopy, Meniscus, Articular cartilage, Single portal
Level of Evidence: Level IV
Trial registration: CTG, NCT02648971. Registered 15 December 2015,
https://clinicaltrials.gov/ct2/show/study/NCT02648971
Introduction
Arthroscopy revolutionized orthopaedic surgery in the 20th century by offering a minimally invasive alternative to open surgical techniques [1]. Currently, two or three portals are used in knee arthroscopy: One to permit the passage of an arthroscope for visualization of the knee joint and others to pass the instruments used for surgical correction. Classically, three portals were used until the benefit of less invasive, two-portal knee arthroscopy was demonstrated [2]. The relationship between fewer portals and improved outcomes reinforced a modern tenet of surgery: The less invasive, the better [3].
As a result, a new single-portal technique for knee arthroscopy was developed in 2013 and updated with new devices two years later [4,5]. Later, in a prospective, non-randomized study comparing single-portal with double-portal knee arthroscopy, the single-portal group self-reported decreased pain and increased function post-operatively. However, it must be noted that objective data, namely surgical time, was not reported. Additionally, the patients' functional outcomes were neither measured with a validated questionnaire nor past three months post-operatively.
The current prospective, double-blind, randomized clinical trial primarily reports surgical time of single-portal knee arthroscopy in comparison to double-portal knee arthroscopy. The secondary outcome of knee function after single-portal arthroscopy is measured by validated questionnaires (International Knee Documentation Committee forms) for up to 12 months post-operatively. Tertiary outcomes include patients' self-reported postoperative pain, overall medication use, and narcotic medication use. It was hypothesized that patients who underwent single-portal knee arthroscopy would show post-operative improvement in all metrics without increased surgical time.
Methods
Study design
The local International Review Board approved this study, and all participants provided informed consent. The study was designed as a double-blind, randomized clinical trial: Before the study was terminated due to low enrollment, a total of 36 patients were recruited with 18 patients undergoing single-portal knee arthroscopy and 18 undergoing double-portal knee arthroscopy. All patients were pre-operatively seen and screened by the lead surgeon (J.H.). Participants were assigned to either surgical technique using a block randomization scheme (block size of 10). A randomization website was used to determine each participant's assignment before surgery. The website documented the name of the person who logged on to perform the randomization and the date and time of the log in; the website also documented the patient's name, medical record number, and study treatment allocation. One day prior to surgery, the surgeon logged onto the randomization website to uncover the patient's assigned group. The patient's assignment was then forwarded to the operating room staff so that all members of the surgical team were prepared for a knee arthroscopy with the particular technique. One surgeon (J.H.) performed all surgeries. At the outset of the study, the surgeon had been performing knee arthroscopy as a fellowship-trained surgeon for 3 years. Additionally, the surgeon trained for the new technique in an industry-sponsored session; a device representative was also present in the room for all single-portal surgeries.
All participants were selected from the Wake Forest Orthopaedic Sports Medicine Clinic's patient population. Inclusion criteria specified men and/or women between ages 21 and 60 who are undergoing a primary knee arthroscopy procedure for meniscus or articular cartilage pathology. Exclusion criteria specified patients with previous reconstructive procedures, lateral retinacular release, microfracture, active knee infection or sepsis at the time of surgery, ligamentous instability, advanced degenerative or inflammatory arthritis, cancer, pregnancy, BMI > 40, or any other condition that may interfere with recovery from knee arthroscopy. Patients receiving Workers' Compensation were also excluded.
Surgical technique
For the standard two-portal knee arthroscopy, the lateral viewing portal was established followed by placement of a medial portal under direct visual inspection. Standard diagnostic arthroscopy was then performed followed by chondroplasty or meniscectomy with motorized shaver (Smith and Nephew) and meniscal punches.
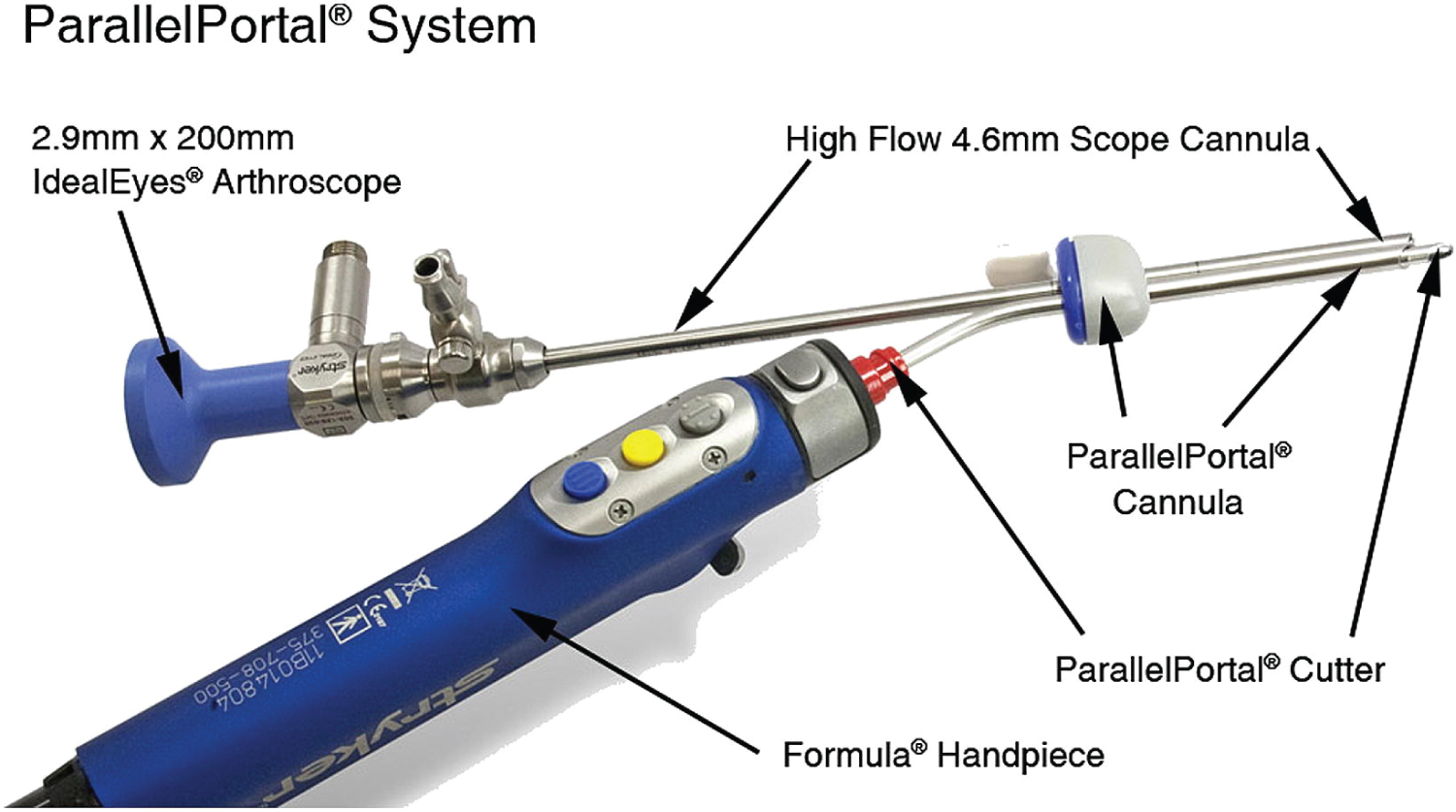
If the patient was randomized to the single-portal technique, a single medial portal was established in every case. A Parallel Portal Cannula (Stryker Endoscopy) was utilized, which functions as a "double-barrel" system for entry into the joint. Using this cannula both the camera and the instruments such as shaver and meniscal punch could be inserted into the knee through the same portal (Figure 1). The shavers have a pre-bend which allows separation of the surgeon's hands and freedom of movement during the procedure.
A tourniquet was typically used for both techniques. Per standard documentation, the surgeon recorded the intra-operative diagnosis and surgical correction performed for each patient. The type of surgery and length of surgery, measured from incision time to closing time, were recorded.
Each patient was sent home with the same standard post-operative instructions. For pain control, patients were instructed to use narcotic pain medication as prescribed (all patients received the same prescription for hydrocodone-acetaminophen unless contraindicated). Patients were instructed to use over-the-counter medications, like acetaminophen, once the pain was manageable. Wound care instructions were given, and all patients were scheduled for follow up 10 days after surgery for a wound check. Those who had a meniscus repair were non-weight-bearing for 4-6 weeks. Others who had a meniscectomy or correction of an articular cartilage defect were permitted to bear weight as tolerated. All patients were given a referral to physical therapy.
Data collection
The International Knee Documentation Committee (IKDC) Forms were used to collect data and include the following: Demographic Information, Current Health Assessment, Knee History Form, Surgical Documentation, Knee Examination, and Subjective Knee Form.
Demographic Information collected data on sex, age, height, weight, race, smoking status, education level, and activity level. The Current Health Assessment is identical to the Short Form-36 except one question about emotional well-being. This form collects data on general health, concurrent medical conditions, physical functioning, social functioning, and emotional well-being.
The Knee History Form records the current injury to the knee, findings on imaging, and previous knee surgeries. Surgical Documentation includes an intra-operative diagnosis and diagrams as well as descriptions of the articular cartilage status, meniscus status, and ligament status. The surgeon also documented the performed surgical corrections here. The Knee Examination form used in this study recorded effusion, crepitus (by compartment), and range of motion as well as motion deficit.
The IKDC Subjective Knee Form was used to evaluate knee function. This form contains 19 questions that require approximately five minutes to complete [6]. It is a reliable and valid knee-specific measure of symptoms, function, and sports activity appropriate for patients with a variety of knee pathology [7,8].
Pain was scored on a visual slider scale from 0, being no pain, to 10, being the worst pain ever experienced. Pain and medication use (overall and narcotic) was self-reported in a diary as well as reported to the study coordinator via phone.
Follow up
The design of the study included six visits: Preoperative, two weeks postoperative, one month postoperative, three months postoperative, six months postoperative, and one year postoperative. At the preoperative visit, patients completed three International Knee Documentation Committee (IKDC) forms: Demographic Information, Current Health Assessment, and Subjective Knee Form. The surgeon completed the Knee History Form. Two weeks postoperative, patients returned for a standard care follow-up; they returned their pain diaries in which they logged daily pain scores as well as daily pain medication use for the first two weeks after surgery. At the one-month and three-month postoperative visits, patients completed the Subjective Knee Form. At the six-month and one-year postoperative visits, patients completed the Subjective Knee Form as well as the Current Health Assessment Form. At every visit, patients received the abbreviated IKDC physical examination in addition to any standard of care examination that was done.
On post-operative days 1 and 4, patients were called and asked to report their pain score, on a scale from 1 to 10 as well as their pain medication use. These calls also functioned to remind patients to complete their daily pain and medicine log for the first two weeks post-operation.
Statistical analysis
Data were analyzed by the Biostatistics, Epidemiology and Research Design (BERD) unit of the Clinical and Translational Science Institute at Wake Forest School of Medicine. A pre-study sample size projection based on data from previous studies [6,7] identified a desired sample size of 50 patients per surgical group to yield 84.7% power to detect a clinically significant difference in IKDC scores with a type I error rate of 5%. Given the observed results and the sample size, this study had poor power to detect a meaningful difference between the groups.
Surgical times were compared using the Student's t-test after examination revealed that the distribution of times was reasonably normal. Baseline characteristics were compared using either a Chi-square test (for categorical variables) or the Student's t-test (for continuous variables). Surgery type was compared using a Fisher's exact test.
The number of reported IKDC scores at 6 months was 8 (single portal) and 5 (double portal); at 12 months 10 (single portal) and 7 (double portal). General linear or logistic regression models with repeated measures were used to compare the IKDC Subjective Knee Form scores, pain scores, and medication use across time. Any baseline variable found to differ significantly between surgical groups was included in these models as a covariate. The possibility of treating day as a continuous variable with regard to the pain scores and medication use diary was considered. Three figures in Appendix B show the actual average pain scores and percentage of medication and narcotic use across time. Based on these figures, there appears to be a quadratic rather than linear relationship with time for at least pain scores and narcotic use. Thus day was included in those models with a quadratic term.
Results
Demographics of the patients who underwent single-portal knee arthroscopy are captured and compared to those who underwent double-portal knee arthroscopy (Table 1). Pre-operative physical function as measured by the Short Form-36 (SF-36) was significantly lower in the single-portal group despite randomization: patients scored nearly 20 points lower on average than those who underwent double-portal knee arthroscopy (p-value = 0.0279). Of the 18 single-portal knee arthroscopies performed, all 18 were non-repairs (e.g. meniscectomy, synovectomy, chondroplasty) while 2 of the 18 double-portal knee arthroscopies were meniscal repairs (p = 0.49). The study had no 'cross-over' patients where a patient randomized to the single-portal technique was found to require a double-portal technique in the operating room.
Average surgical time for single-portal knee arthroscopy was 28.44 ± 7.6 minutes. Average surgical time for double-portal knee arthroscopy was 38.39 ± 10.9. Single-portal knee arthroscopy was performed 9.95 minutes quicker than double-portal knee arthroscopy; this difference was not statistically significant (p = 0.066).
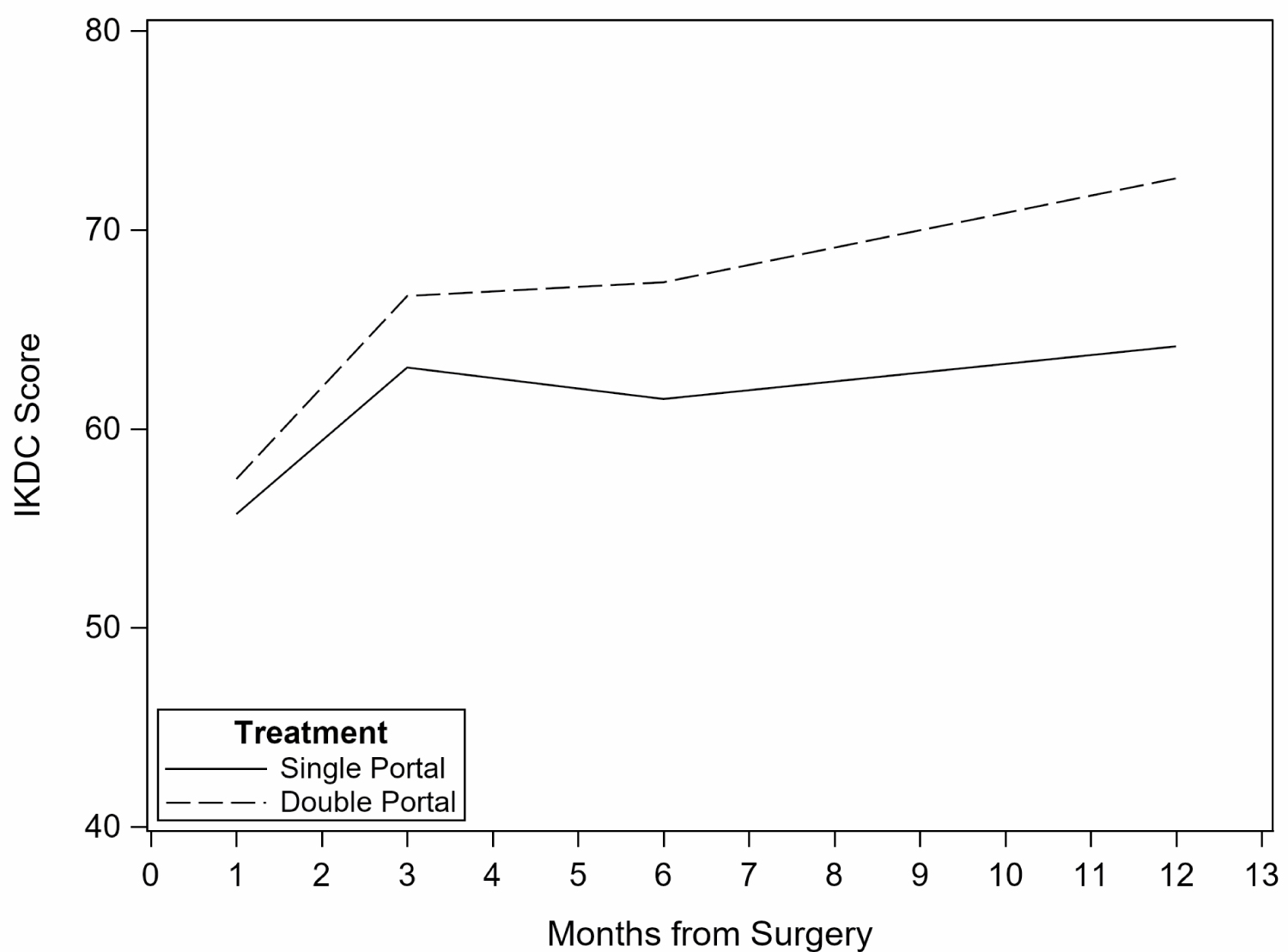
For all patients, knee function, as measured by IKDC scores, improved over time (p = 0.028) (Figure 2). Adjustment for baseline physical function and surgery type did not alter the results. The study was too underpowered to detect a difference between treatment groups.
Pain scores acquired by follow-up telephone calls at Day 4 are significantly lower than at Day 1 for all patients (p = 0.0034). Pain scores differed significantly by surgery type with higher scores at both Day 1 and Day 4 among those with meniscus repair (p = 0.042); however, there is no difference between treatment groups (p = 0.57). Similarly, average pain score in self-reported patient diaries declined in the first 14 days after surgery with no statistically significant difference between groups. Results were not altered by adjustment for pre-operative physical function (Figure 3).
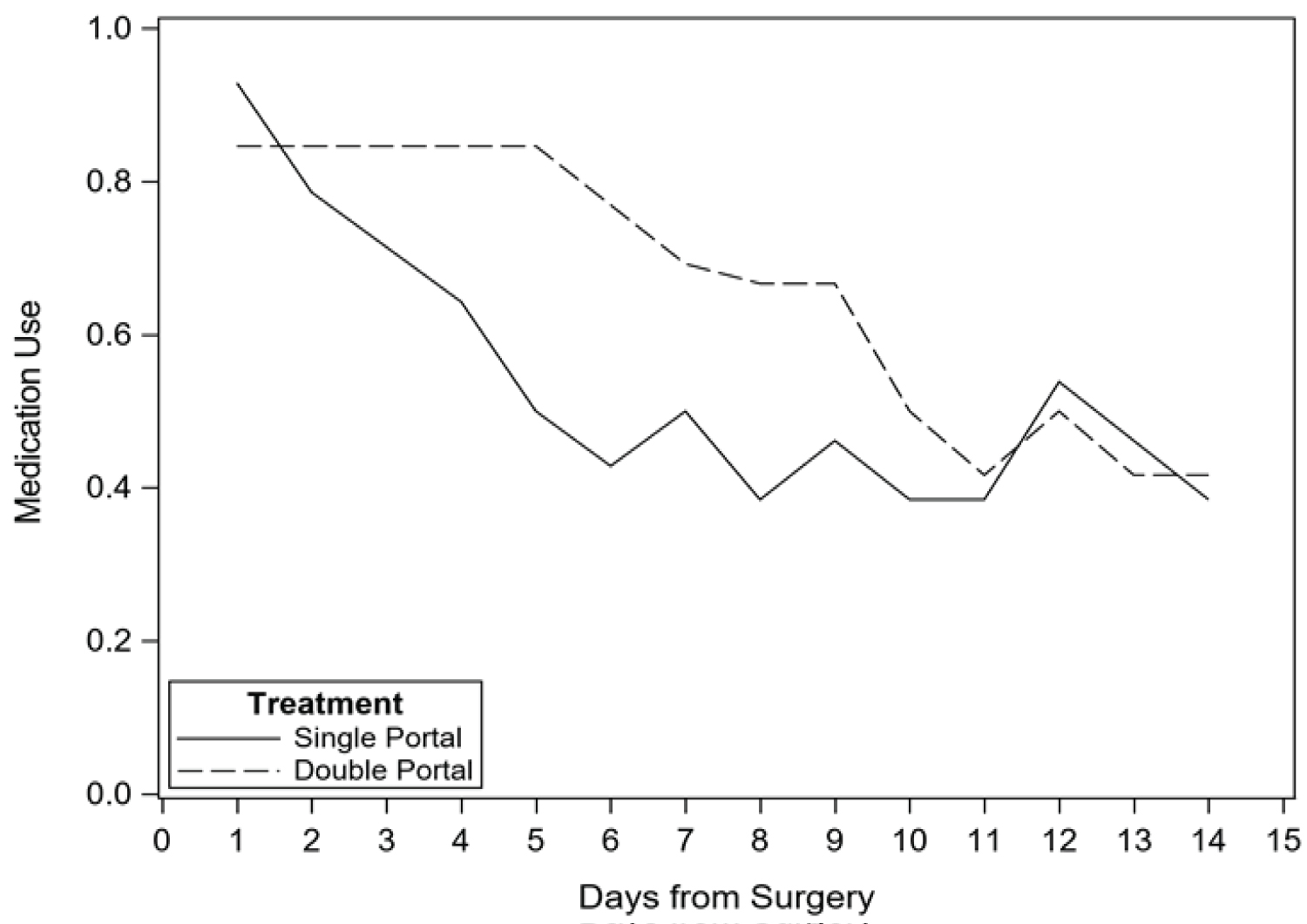
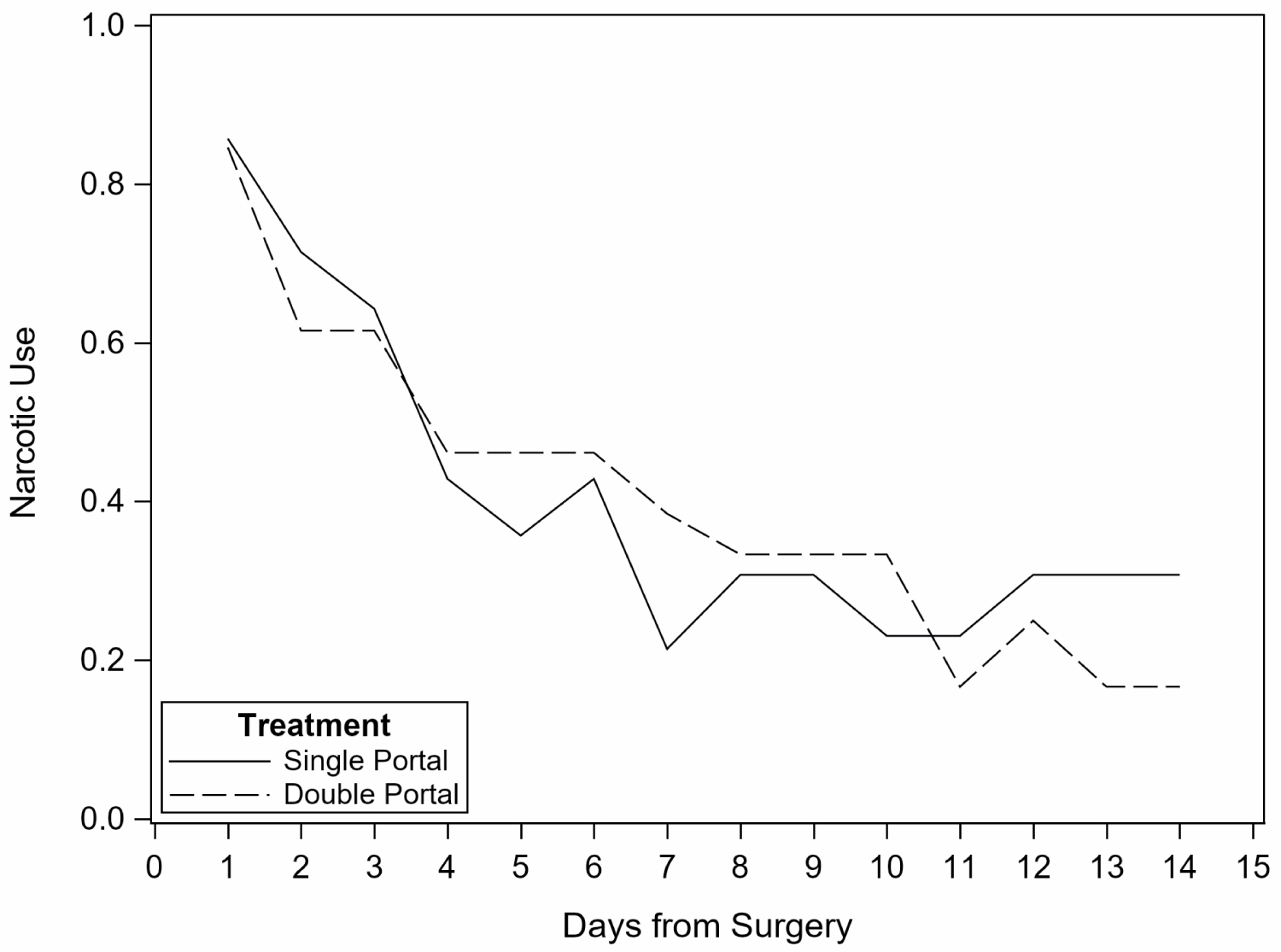
Medication use reported on follow-up telephone calls decreased significantly on Day 4 when compared to Day 1 for all patients (p = 0.0057); however, there was no difference between treatment groups (p = 0.32). Medication use per patient diaries also declined across the first 14 days with no statistically significant difference between groups (Figure 4). In particular, narcotic use also decreased from Day 1 to Day 4 (p = 0.0003) but did not differ between treatment groups (p = 0.42). In the first 14 days after surgery, narcotic use declined as well with no statistically significant difference between groups (Figure 5). Adjustment for pre-operative physical function did not alter the results.
Zero patients had serious adverse events (infection, blood loss, cardiorespiratory arrest, or death) related to the surgery. A total of 8 patients had post-operative concerns: 5 were in Group 1 and 3 were in Group 2. In Group 1, all concerns were related to persistent pain which required local injection for relief at post-operative follow-up. In Group 2, 1 patient had drainage from the incision without a diagnosed infection, 1 patient had calf swelling without a deep vein thrombosis, and 1 had persistent post-operative pain requiring a local injection.
Discussion
This randomized clinical trial is only the second to prospectively investigate single-portal knee arthroscopy; it is the first to compare surgical time to the double-portal technique. It is also the first to use IKDC forms in order to standardize data collection with a validated questionnaire [6-8]. Finally, follow-up for one year offered more longitudinal data on this new surgical procedure.
The novel single-portal arthroscopic technique does not lengthen operating time, which is a known predictor of postoperative pain and is associated with an increased risk of adverse events, including readmission [9-12]. Depending on the surgery, a certain threshold number of cases and/or years of experience is necessary before consistently acceptable outcomes are achieved [13]. For knee arthroscopy, 40% of resident physicians achieved competency after a median of 16 procedures [14]. Thus, the intra-operative time for single-portal surgery in this study can likely be attributed to the lead surgeon's overall arthroscopic experience and dedicated training in this technique, as well as the absence of surgical residents participating in the experimental single-portal surgery.
The surgeon employed the single-portal technique without significant technical limitations as evidenced by the absence of cross over to a double-portal approach. A single medial port was established each time for consistency though lateral or suprapatellar entry is possible as well. From the medial port, the medial and lateral compartments as well as the patellofemoral joint were easily accessed and fully examined [5]. None of the patients in the single-portal group required multi-step instrumentation, such as stabilization of an osteochondral lesion with pins or meniscal repair with sutures; either of these scenarios would likely require an additional portal for further instrumentation. Thus, there were no cross-over patients in this study. In the future, selecting cases that are anticipated to require minimal instrumentation will be critical to reducing intra-operative conversion of technique; however, the technique is easily converted to a double-portal technique if further instrumentation is deemed necessary by the surgeon [4].
The technical difficulties of the single-portal technique largely stem from insertion of the scope and the instrument through the same portal. Unlike the double-portal technique where both enter through different portals and can be used 90 degrees to one another, the single-portal technique requires the scope and the instrument to be used in line at 0 degrees. Additionally, given that both the scope and the instrument(s) are close to one another, the scope hand exterior to the joint can impede the instrument hand. The shavers have a pre-bend which allows separation of the surgeon's hands and freedom of movement to better achieve arthroscopic triangulation [5]. Lastly, the instrument can easily cross over the scope, so it is important to keep both the scope and the instrument parallel to avoid this.
The number of portals has been shown to impact post-operative function: knee arthroscopy with two portals produced greater and quicker recovery of physical function for patients when compared to three portals [2]. In this study, while comparison of physical function between double-portal and single-portal techniques is limited by statistical power, the significant recovery of physical function up to twelve months after single-portal surgery confirms that the novel technique produces the expected functional benefit of knee arthroscopy.
In a prior prospective study, number of portals was also correlated to post-operative pain: patients who underwent single-portal knee arthroscopy reported less post-operative pain and were less likely to use narcotics for pain relief compared to patients who underwent double-portal knee arthroscopy [15]. The single-portal group also reported less swelling one month after surgery and less portal scarring and tenderness three months after surgery [15]. Such findings are consistent with research that found fibrous scars in the infrapatellar fat pad are accentuated at the portal [16]. In this study, although patients in the single-portal group reported significantly less pain and used less analgesic medication over time post-operatively, the lack of significant difference from the double-portal group challenges the relationship between fewer portals and decreased pain. Underlying knee pathology and subsequent surgical treatment primarily determine post-operative pain; however, there is no significant difference in surgery types between groups. Other factors unmeasured here, including pre-operative resilience and patient expectations, also contribute to post-operative pain and might be further elucidative [17,18].
This study was designed as a randomized clinical trial but was significantly limited by a small sample size; thus, the study was terminated by Stryker after three years of limited enrollment. The high dropout rate of a small number of patients over the course of the study compromises the reliability of the comparative results. A randomized clinical trial with adequate patient enrollment that compares single-portal to double-portal knee arthroscopy may offer a more reliable comparison between the two techniques.
In conclusion, single-portal knee arthroscopy benefits patients post-operatively without increasing intra-operative surgical time. Based on this data, single-portal knee arthroscopy has possible technical advantages for meniscus and articular cartilage pathology that requires minimal surgical instrumentation.
Declarations
Funding
This study was funded by Stryker Corporation.
Conflicts of interest
The authors confirm that they have no conflicts of interest, financial or otherwise.
Availability of data and material
Available.
Authors' contributions
All named authors contributed significantly to underlying research and drafting of this manuscript.
Acknowledgements
We thank Joni Evans and Tim Craven of Wake Forest Baptist Medical Center Clinical and Translational Science Institute for their assistance with statistical analysis.
References
- Simpson DA, Thomas NP, Aichroth PM (1986) Open and closed meniscectomy. A comparative analysis. J Bone Joint Surg Br 68: 301-304.
- Stetson WB, Templin K (2002) Two- versus three-portal technique for routine knee arthroscopy. Am J Sports Med 30: 108-111.
- Mohiuddin K, Swanson SJ (2013) Maximizing the benefit of minimally invasive surgery. J Surg Oncol 108: 315-319.
- Cooper DE, Fouts B (2016) Single Portal Knee Arthroscopy: 2015 Technique Update. Arthroscopy Techniques 5: e17-e22.
- Cooper DE, Fouts B (2013) Single-portal arthroscopy: Report of a new technique. Arthroscopy Techniques 2: e265-e269.
- Van de Graaf V, Wolterbeek N, Scholtes VA, et al. (2014) Reliability and validity of the IKDC, KOOS, and WOMAC for Patients with Meniscal Injuries. Am J Sports Med 42: 1408-1416.
- Irrgang JJ, Anderson AF, Boland AL, et al. (2001) Development and validation of the international knee documentation committee subjective knee form. Am J Sports Med 29: 600-613.
- Crawford K, Briggs KK, Rodkey WG, et al. (2007) Reliability, validity, and responsiveness of the IKDC score for meniscus injuries of the knee. Arthroscopy 23: 839-844.
- Dahmani S, Dupont H, Mantz J, et al. (2001) Predictive factors of early morphine requirements in the post-anaesthesia care unit (PACU). Br J Anaesth 87: 385-389.
- Gagliese L, Gauthier LR, Macpherson AK, et al. (2008) Correlates of postoperative pain and intravenous patient-controlled analgesia use in younger and older surgical patients. Pain Med 9: 299-314.
- Gowd AK, Liu JN, Bohl DD, et al. (2019) Operative time as an independent and modifiable risk factor for short-term complications after knee arthroscopy. Arthroscopy 35: 2089-2098.
- Hartwell MJ, Morgan AM, Johnson DJ, et al. (2020) Risk factors for 30-day readmission following knee arthroscopy. J Knee Surg 33: 1109-1115.
- Hopper AN, Jamison MH, Lewis WG (2007) Learning curves in surgical practice. Postgrad Med J 83: 777-779.
- Hodgins JL, Veillette C, Biau D, et al. (2014) The knee arthroscopy learning curve: Quantitative assessment of surgical skills. Arthroscopy 30: 613-621.
- Cooper DE (2016) Single-portal versus two-portal knee arthroscopy: First clinical experience with a new surgical technique. Orthopedics 39: e36-e42.
- Tang G, Niitsu M, Ikeda K, et al. (2000) Fibrous scar in the infrapatellar fat pad after arthroscopy: MR imaging. Radiat Med 18: 1-5.
- Shaha JS, Shaha SH, Bottoni CR, et al. (2017) Preoperative resilience strongest predictor of postoperative outcome following an arthroscopic bankart repair. Orthop J Sports Med 5: 2325967117S00113.
- Waljee J, McGlinn EP, Sears ED, et al. (2014) Patient expectations and patient-reported outcomes in surgery: A systematic review. Surgery 155: 799-808.
Corresponding Author
Dr. Pallavi Juneja, MD, New York-Presbyterian Columbia University Irving Medical Center, 630 W 168th Street, New York, NY 10032, USA.
Copyright
© 2021 Juneja P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.