Robotic Arm Assisted Total Knee Arthroplasty in Patients with Flexible versus Fixed Deformities
Abstract
Introduction: A total knee arthroplasty aims to achieve a stable, well aligned, and balanced knee through range of motion. Arthritic knees with rigid alignment can be challenging to balance reliably by both measured resection and gap balancing techniques. Titration of soft tissue releases can be difficult to reproducibly assess, resulting in over- or under-releases. The robotic arm platform has recently introduced a novel concept of knee balancing by implant manipulation.
Materials and methods: We illustrate the use of robotic arm technology to address flexible deformities and present a "skim cut protocol" to correct rigid deformities. The protocol proposes a preliminary proximal tibia cut, as well as distal femur and posterior femur cuts for a component one size larger than the planned implant. The knee is then balanced as in flexible deformities and final cuts are made to achieve normal alignment.
Conclusion: The skim cut protocol effectively restores alignment of rigid knees while minimizing soft tissue releases.
Keywords
Robotic arm total knee arthroplasty, Rigid knee deformity, Fixed varus knee, Fixed valgus knee
Introduction
Total knee arthroplasty is often the treatment of choice for patients with end stage arthritis of the knee. Surgical execution of a knee replacement follows several principles, with the two general workflows based on bone resection or gap balancing [1]. Over the years, navigation and patient specific instrumentation have evolved as options for the implementation of the procedure [2,3]. More recently, robotic arm assisted knee replacement was introduced with a novel concept of implant manipulation to achieve balanced gaps throughout range of motion [4,5].
Regardless of the method used to execute a total knee arthroplasty, the ultimate goal is to achieve a knee that is anatomically aligned relative to the mechanical axis, stable throughout range of motion, and well balanced [4]. These goals are applicable in all situations, regardless of the deformity being addressed, and whether it is fixed or flexible.
While a significant component of malalignment can be corrected in deformed knees once bony cuts are made and osteophytes are removed, fixed deformities tend to be more challenging [6,7]. They may require more aggressive soft tissue releases, which are often difficult to titrate to the extent needed. The robotic arm total knee application is primarily based on the premise of knee gap balancing via implant manipulation, with soft tissue releases implemented when implant manipulation fails to equalize gaps [8]. Knee alignment needs to be attained prior to final bony resections. In correctable deformities, this is achievable, while in fixed ones, it is sometimes not.
In this paper, we describe the use of robotic arm assisted total knee replacement to accomplish the above goals. The workflow for flexible deformities will be reviewed, followed by the introduction of an alternative workflow for knees with fixed deformities. Illustrative examples will be discussed for each deformity.
Materials and Methods
This work has been approved by the Institutional Review Board at our hospital.
Workflow for all knees
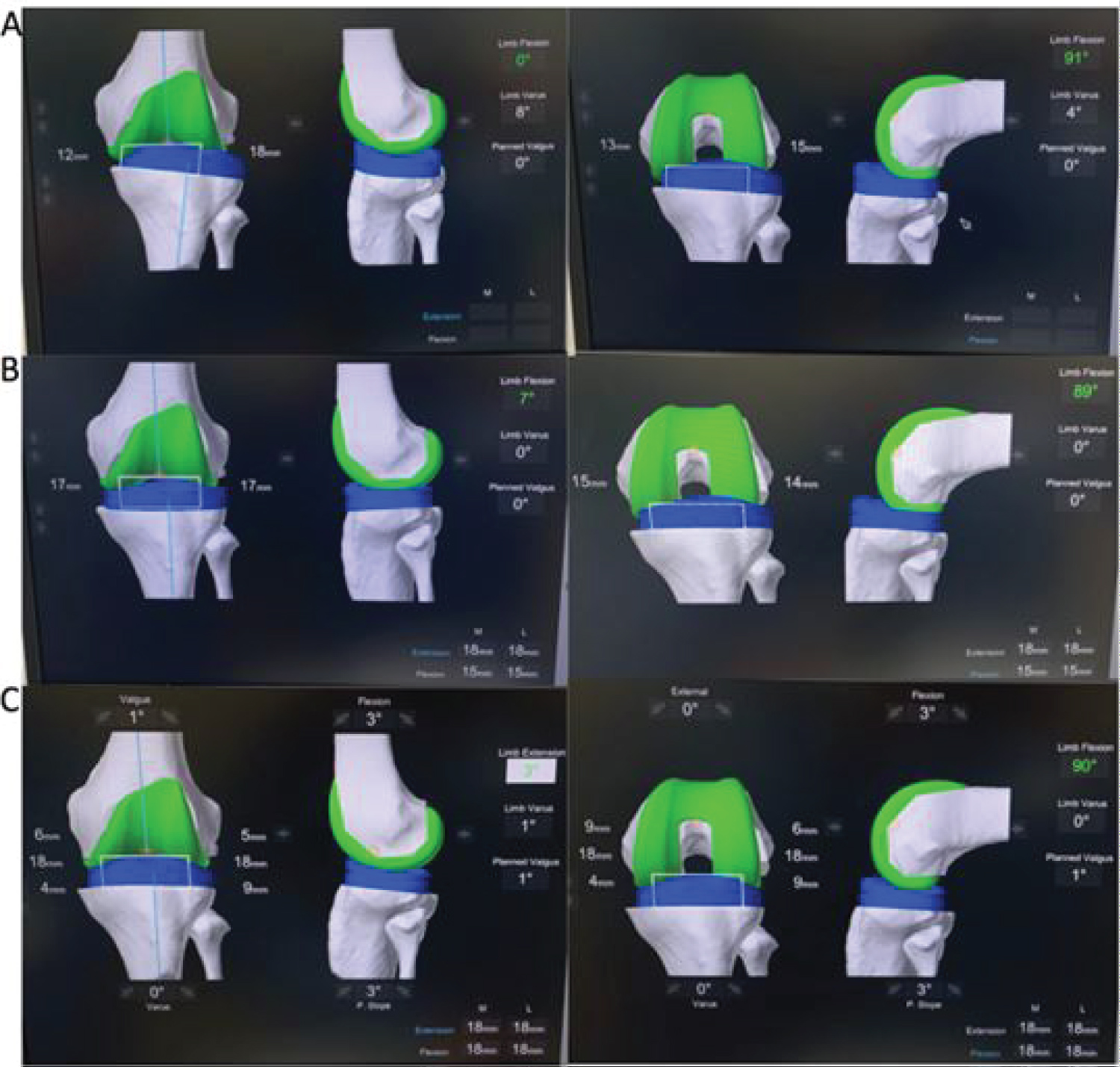
The robotic arm assisted total knee replacement application requires a preoperative CT scan for segmentation of the patient's anatomy and mechanical axis. The landmarks are verified on the scan and a preliminary resection plan is generated (Supplemental Figure S1). In the operating room, trackers are placed in the tibia and femur; the hip center, medial and lateral malleoli, distal femur, and proximal tibia are all registered to match the patient's anatomy to the CT plan. The software then enters the dynamic balancing page to allow for gap balancing (Figure 1). The flow up to this point applies to all types of knee deformities, fixed or flexible.
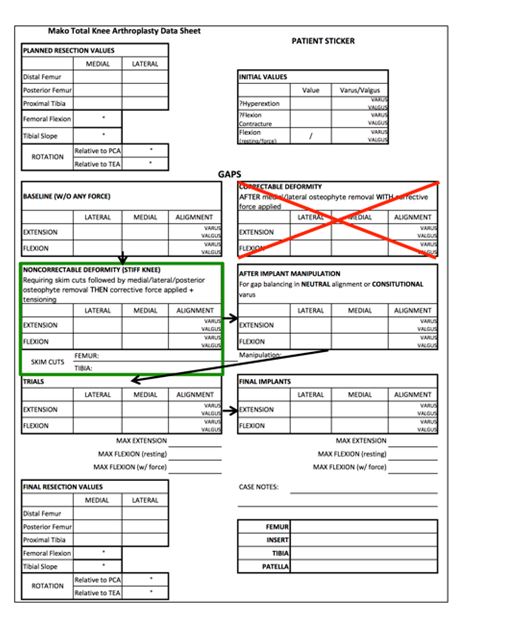
A planning sheet is used throughout the procedure to describe the workflow as the plan is executed (Supplemental Figure S2). The initial alignment, gaps, and bone resection values are all noted at the beginning of the case.
Workflow for flexible deformities
After registration, the software determines baseline varus/valgus alignment of the knee in extension and flexion (Figure 1A). The alignment is then corrected by manual stress (correctable deformity) in extension and flexion (Figure 1B). Pose captures in the desired (often neutral) alignment are then obtained and the implants are manipulated to create balanced and equal gaps in extension and flexion (Figure 1C). The execution of the balanced plan allows for placement of a total knee that matches the patient's anatomy with equal gaps medially and laterally throughout range of motion. This flow is illustrated in the planning sheet (Supplemental Figure S3).
Workflow for fixed deformities
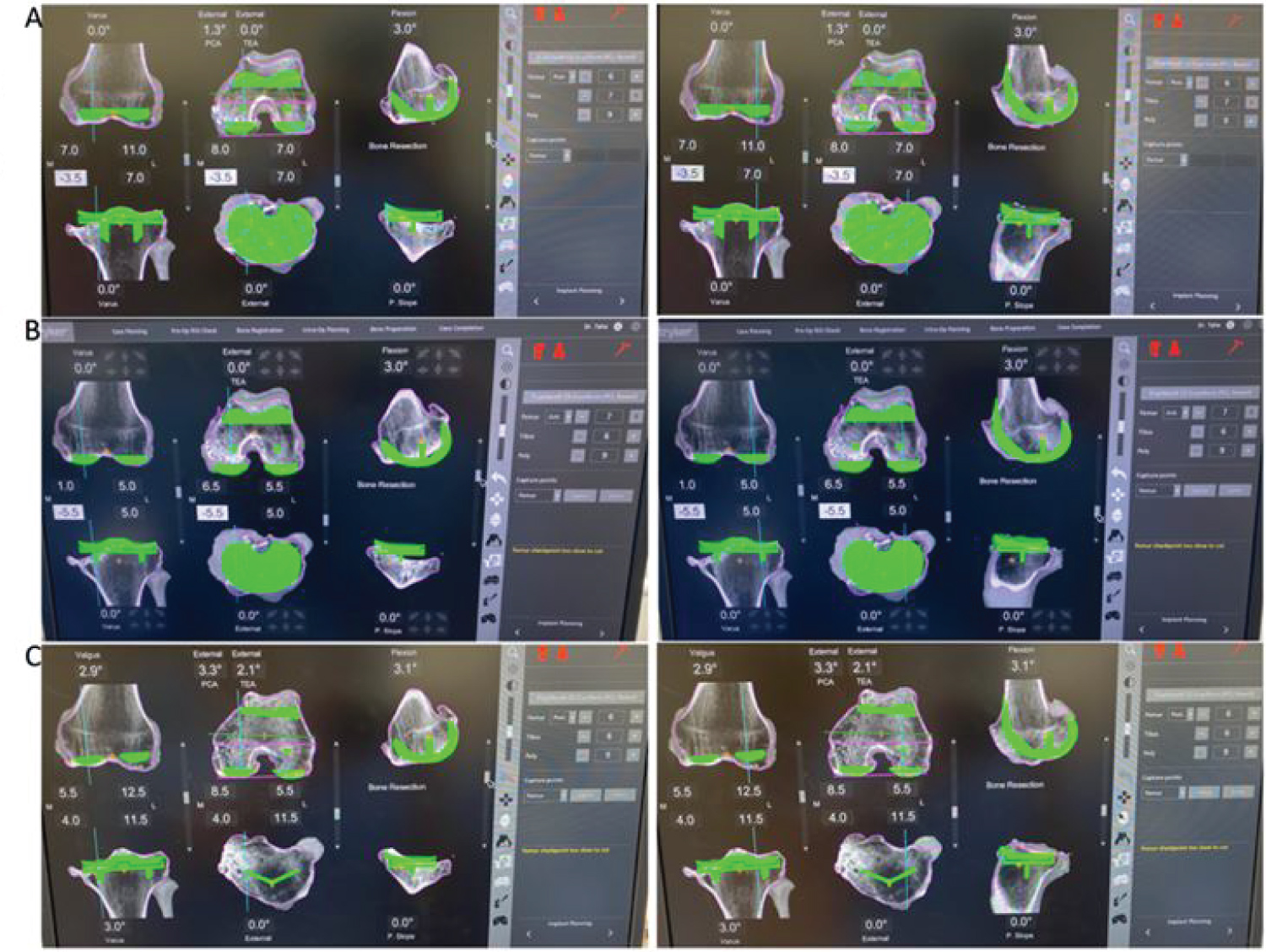
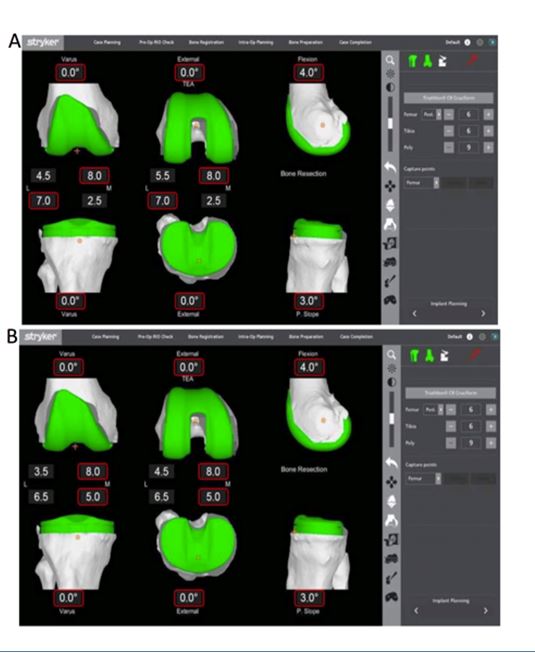
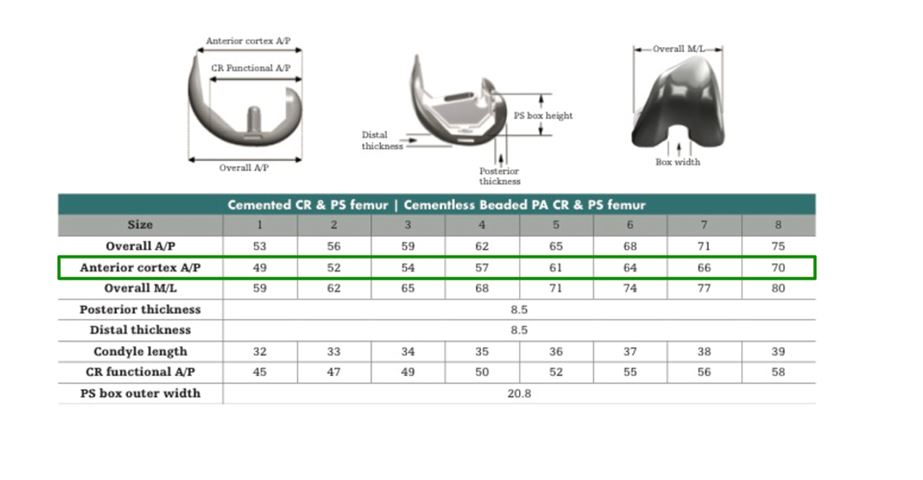
If the deformity is non-correctable, meaning neutral alignment cannot be achieved with manual stress prior to bone resection, a skim cut approach is followed. This protocol starts with three cuts: The distal femur, the posterior femur and the proximal tibia. Using an anterior referencing platform (Figure 2), the femur is anchored anteriorly and upsized one size to under-resect the posterior femur. This change allows a posterior skim cut. The dimensions of the Triathlon femoral component are shown in Supplemental Figure S4, illustrating how much less bone is resected when the femur is upsized. The femur is also distalized to remove 5 mm from the low side, accounting for a distal skim cut (Figure 2B). The tibia is moved proximally until only 5 mm are resected from the high side (Figure 2B). This change allows for a tibial skim cut. The robotic arm is then used to make the above three skim cuts.
Once the cuts are made, accessible osteophytes are removed to allow for more accurate joint balancing. At this point, the knee deformity becomes correctable. The femur is again anchored anteriorly and reverted to the original planned size (Figure 2C). The femur and tibia are moved back to the original plan (Figure 2A).
It is critical then to balance the knee with a tensioner in place while the alignment is corrected in order to avoid excessive resections. Pose captures are obtained with the knee in neutral alignment and tensioned in extension and flexion, essentially as in the flexible deformity flow. Implants are manipulated to achieve equal gaps (Figure 2C) and the final cuts are made and the trial implants are placed. This flow is illustrated by the planning sheet in Supplemental Figure S5.
Neutral alignment (or close to so) should always be attained prior to pose captures in extension. Neutral alignment may be less critical or possibly non-achievable in flexion. In these cases, a capture can be obtained in varus or valgus, but the gaps should still be balanced appropriately.
In the section below, we present four cases to illustrate the concepts above. Case 1: Correctable varus deformity. Case 2: Correctable valgus deformity. Case 3: Non-correctable varus deformity. Case 4: Non-correctable valgus deformity. Cases 1 and 2 use the routine workflow. Cases 3 and 4 use the skim cut protocol. We also show a case with windswept knees with fixed deformities.
Results
Case 1 (Flexible varus deformity)
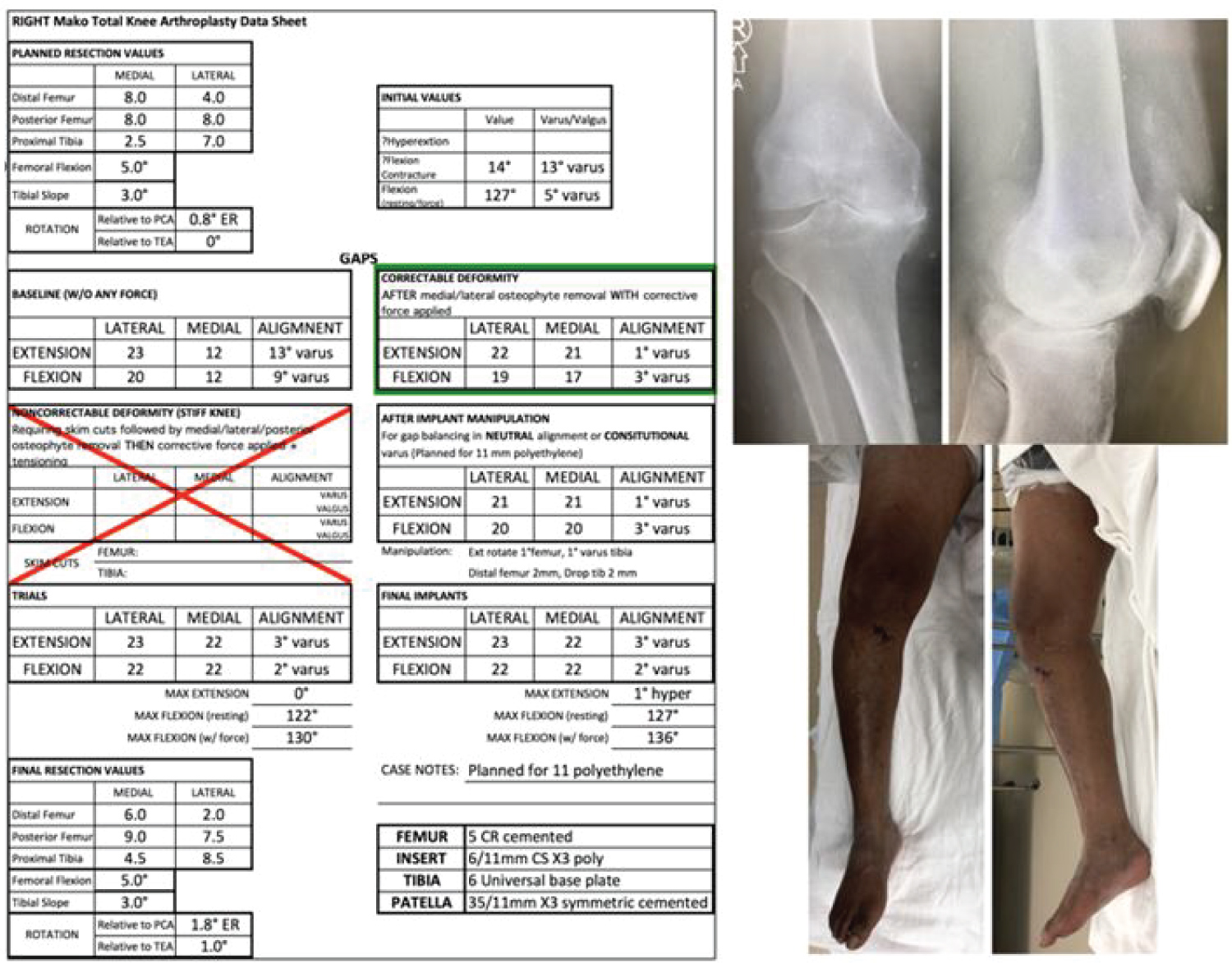
The patient is a 63-year-old male with tri-compartmental arthritis most significant in the medial compartment. His X-rays, clinical images, and planning sheet are shown in Figure 3. He started with a 14-degree flexion contracture and 13 degrees of varus in extension and 9 degrees of varus at 90 degrees of flexion. His deformity, despite being severe, was correctable by manual stress to 1 degree of varus in extension and 3 degrees of varus in flexion (Figure 3, box highlighted in green). The knee pose captures were obtained while the knee was in the above alignment. Implants were then manipulated to obtain gaps of 21 mm in extension (to account for a significant flexion contracture and an 11 mm polyethylene). In flexion, the gaps were balanced to 20 mm (for an 11 mm polyethylene). Cuts made with the robotic arm and final implant placement resulted in a knee well balanced in flexion and extension and eliminated his flexion contracture. There were no soft tissue releases done in this patient besides the release necessary for exposure. His clinical 3-month pictures are shown in Figure 4, as well as his postoperative images at the same time point.
Case 2 (Flexible valgus deformity)
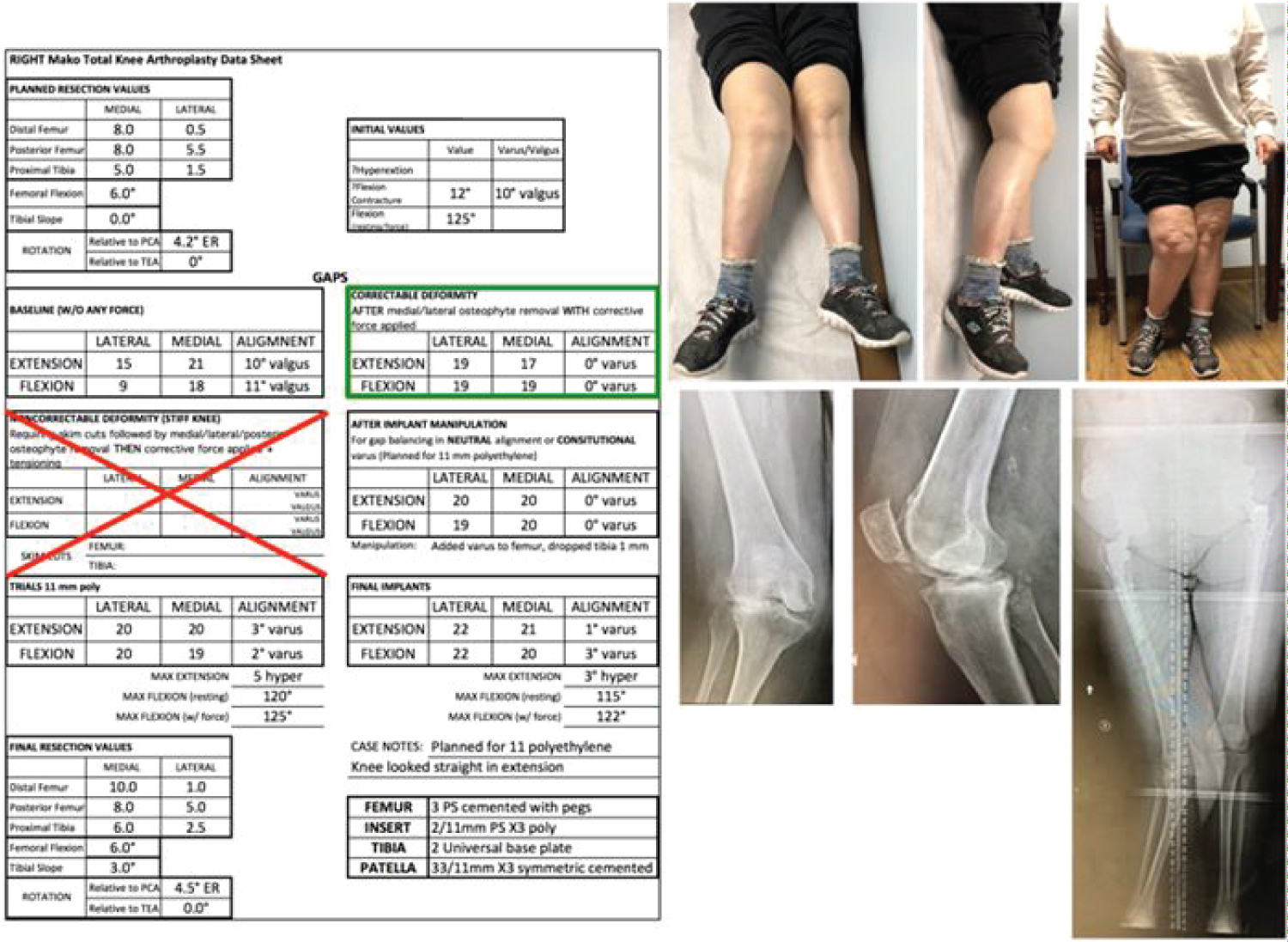
The patient is a 54-year-old female with tri-compartmental knee arthritis, most significant in the lateral compartment of the knee. Her X-rays, clinical images and planning sheet are shown in Figure 5. She started with a 12-degree flexion contracture and 10 degrees of valgus in extension and 11 degrees of valgus at 90 degrees of flexion. Her deformity, while severe, was correctable by manual stress to 0 degree of varus in extension and 0 degrees of varus in flexion (Figure 5, box highlighted in green). The knee pose captures were obtained while the knee was in the above alignment. Implants were then manipulated to obtain gaps of 20 mm in extension (to fit an 11 mm polyethylene). In flexion, the gaps were balanced to 19-20 mm (for an 11 mm polyethylene). Cuts made with the robotic arm and final implant placement resulted in a knee well balanced in flexion and extension and eliminated her flexion contracture. Minimal pie crusting of the IT band was needed for final balancing. Her clinical postoperative standing picture is shown in Figure 6, as well as her postoperative images at the same time point.
Case 3 (Rigid varus deformity)
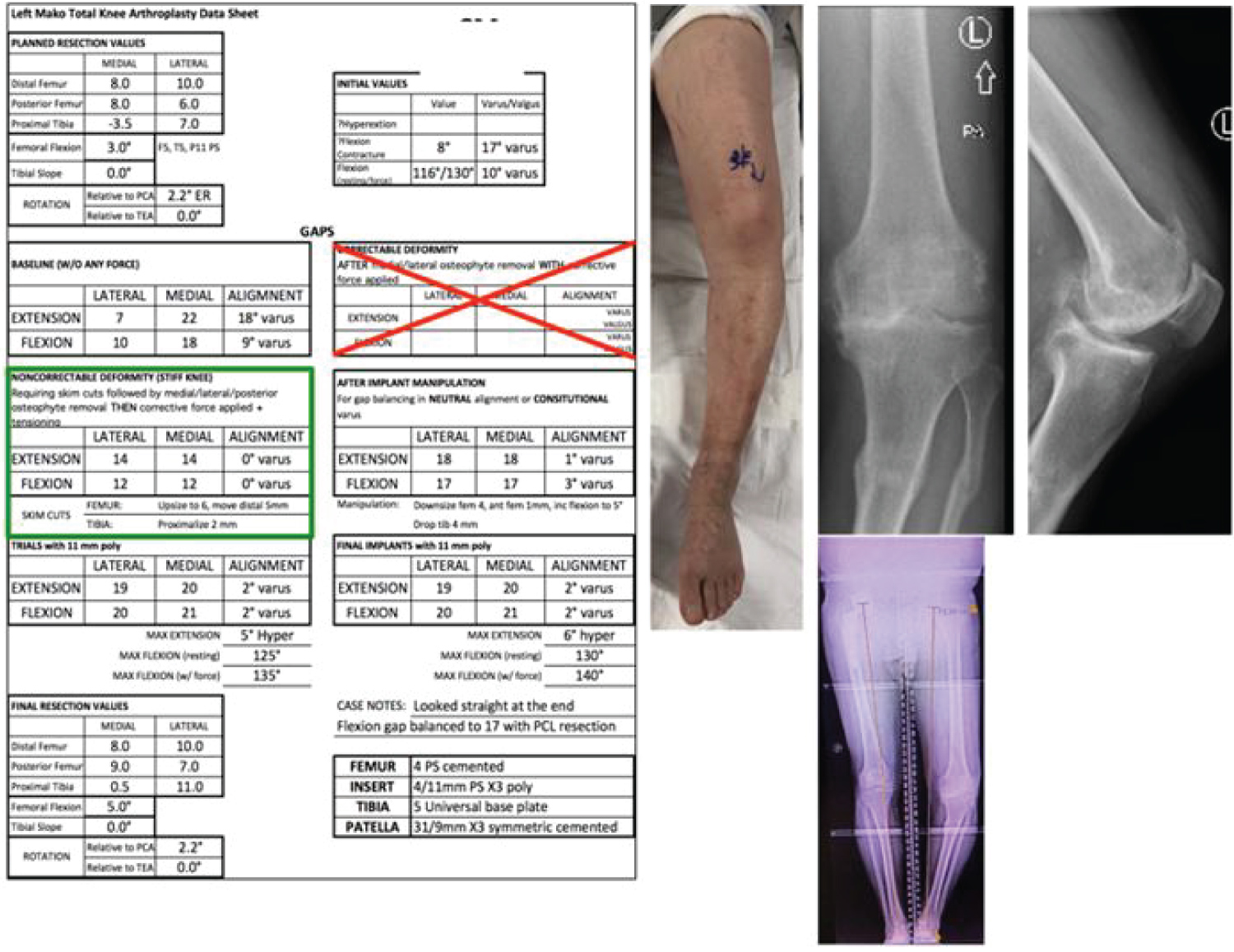
The patient is a 74-year-old male with tri-compartmental knee arthritis most notable in the medial compartment. He is also noted to have a proximal tibia malunion from an old fracture. His X-rays, clinical images, and planning sheet are shown in Figure 7. He started with an 8-degree flexion contracture and 17-18 degrees of varus in extension and 9 degrees of varus in 90 degrees of flexion. His deformity was non-correctable by manual stress, necessitating a skim cut protocol. The femur was anchored anteriorly and upsized to a size 6 component (from a planned size 5). The femur was distalized to resect 5 mm from the lateral side. The tibia was proximalized 2 mm.
Once the skim cuts were completed. Correction to 0 degrees of varus was possible with the tensioning device in extension and flexion (Figure 7-Green box). The femur was downsized back to the planned size 5 and implant manipulation was done to generate 18 mm gaps in extension and 17 mm gaps in flexion. To balance this knee, the femur had to be downsized further to a size 4 implant. The final cuts were made with the robotic arm and final implant placement resulted in a knee well balanced in flexion and extension and eliminated his flexion contracture. The only release done was that needed for exposure medially. His clinical follow-up pictures are shown in Figure 8, as well as his postoperative images at the same time point.
Case 4 (Rigid valgus deformity)
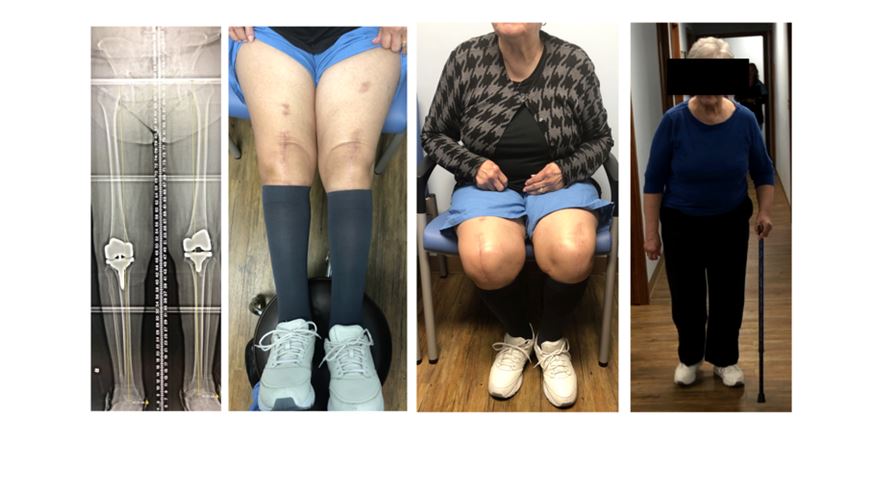
The patient is an 86-year-old female with tri-compartmental knee arthritis most notable in the lateral compartment. Her X-rays, clinical images, and planning sheet are shown in Figure 9. She started with a 15-degree flexion contracture and 17 degrees of valgus in extension and 7 degrees of valgus in 90 degrees of flexion. Her deformity was non-correctable by manual stress, necessitating a skim cut protocol. The femur was anchored anteriorly and upsized to a size 2 component. While we typically distalize the femur and proximalize the tibia for skim cuts, we adjusted the implants in this case to resect 1 mm from the lateral distal femur (because of significant wear) and made the tibial cut as planned because there was only 3.5 mm resection on the lateral tibia. These cuts were still considered minimal skim cuts through the defects on the distal lateral femur and proximal lateral tibia.
Once the skim cuts were completed, the femur was downsized back to a size 1. Correction to 1 degree of valgus was possible with the tensioning device in extension and flexion (Figure 9-Green box). Implant manipulation was done to generate 18 mm gaps in extension and 19 mm gaps in flexion. The final cuts were made with the robotic arm and final implant placement resulted in a knee that is well balanced in flexion and extension with no flexion contracture. Minimal pie crusting of the IT band was done for final balance fine-tuning. Her clinical follow-up pictures are shown in Figure 10, as well as her postoperative images at the same time point.
Case 5 (Combined fixed varus and valgus deformity case)
The patient is a 70-year-old female who presented with wind swept rigid knees from long-standing rheumatoid arthritis. The skim cut protocol was applied to execute both knee arthroplasties in different settings. Her preoperative and postoperative clinical images and alignment films are shown in Supplemental Figure S6 and Supplemental Figure S7.
Discussion
Total knee arthroplasty is a very effective procedure to address pain and deformity in the arthritic knee. While the goals of TKA are clear, the execution of the procedure can vary depending on approach and philosophy [9]. The robotic arm total knee replacement platform utilizes a CT based implant planning module accompanied with gap balancing during the procedure to achieve a well-aligned and balanced knee. While bone resection using manual jigs is often easy to accomplish, knee balancing with titration of ligament releases is much more challenging [10]. The robotic platform titrates gap tightness with implant manipulation rather than ligament releases.
The robotic total knee system introduces a new workflow for knee balancing. While measured resection and gap balancing techniques both make at least some bone resections before the knee is balanced, the routine robotic platform does the joint balancing prior to any resections. This workflow works well in patients with correctable deformities and is more resembling of the measured resection workflow. The standard approach relies on the premise that there is enough ligament laxity to align the knee into neutral (or close to neutral) mechanical alignment. When this is achievable, small implant manipulations are all that is required to balance the knee gaps in flexion and extension. The adjustments in implant positions in these cases are within the constraints allowed for the Triathlon system (typically 3 degrees of implant rotation and combined femoral flexion and tibial slope of 8 degrees).
In fixed deformities, two challenges are faced. The first is that knee alignment is not achievable by manual stress prior to bony cuts. The second is that achieving balanced gaps requires significant implant manipulations, which are often outside the constraints allowed. The skim cut protocol addresses both of these limitations. The skim resections made prior to balancing allows the knee to be aligned easily with a tensioner, so that pose captures are obtained with the knee in neutral (or close to neutral) alignment. The protocol then addresses gaps with routine implant manipulations that do not fall out of the imposed constraints. The execution of this protocol makes the work flow predictable and reproducible in impressively deformed and rigid knees.
While the above workflow resembles the gap balancing technique, it is more effective in that the thickness of bone resections can be known (and potentially adjusted) prior to making any cuts. It has been shown that the gap balancing method often resects more bone from the posteromedial femur compared to the measure resection technique [1]. With the robotic application, implants can be manipulated to minimize over-resections and match anatomy, while achieving balance.
The limitations of this paper are that it is based on a small, albeit promising case series. We believe it has applicability in scenarios beyond osteoarthritis, possibly posttraumatic arthritis, where ligament compliance is limited and where deformities can be significant and rigid. Our work introduces a reliable workflow to address knees with flexible and rigid deformities using the robotic arm platform. The ability to balance the knee by skim cuts and implant manipulations reduces the need for soft tissue releases in knees with significant deformities. The protocol is reproducible and allows the execution of a balanced knee with less soft tissue dissection.
References
- Tapasvi SR, Shekhar A, Patil SS, et al. (2020) Comparison of gap balancing vs measured resection technique in patients undergoing simultaneous bilateral total knee arthroplasty: One technique per knee. J Arthroplasty 35: 732-740.
- Jones CW, Jerabek SA (2018) Current role of computer navigation in total knee arthroplasty. J Arthroplasty 33: 1989-1993.
- Kizaki K, Shanmugaraj A, Yamashita F, et al. (2019) Total knee arthroplasty using patient-specific instrumentation for osteoarthritis of the knee: A meta-analysis. BMC Musculoskelet Disord 20: 561.
- Kayani B, Konan S, Tahmassebi J, et al. (2020) A prospective double-blinded randomised control trial comparing robotic arm-assisted functionally aligned total knee arthroplasty versus robotic arm-assisted mechanically aligned total knee arthroplasty. Trials 21: 194.
- Sherman WF, Wu VJ (2020) Robotic surgery in total joint arthroplasty: A survey of the AAHKS membership to understand the utilization, motivations, and perceptions of total joint surgeons. J Arthroplasty 35: 3474-3481.e2.
- Krackow KA, Jones MM, Teeny SM, et al. (1991) Primary total knee arthroplasty in patients with fixed valgus deformity. Clin Orthop 273: 9-18.
- Ritter MA, Faris GW, Faris PM, et al. (2004) Total knee arthroplasty in patients with angular varus or valgus deformities of = 20°. J Arthroplasty 19: 862-866.
- Marchand R, Khlopas A, Sodhi N, et al. (2018) Difficult cases in robotic arm-assisted total knee arthroplasty: A case series. J Knee Surg 31: 27-37.
- Dennis DA, Komistek RD, Kim RH, et al. (2010) Gap balancing versus measured resection technique for total knee arthroplasty. Clin Orthop Relat Res 468: 102-107.
- Cho KJ, Seon JK, Jang WY, et al. (2018) Objective quantification of ligament balancing using verasense in measured resection and modified gap balance total knee arthroplasty. BMC Musculoskelet Disord 19: 266.
Corresponding Author
Tarek A Taha, MD, PhD, Orthopaedics and Sports Medicine, Ascension Medical Group, 4677 Towne Centre Road, Med Arts 3, 2nd Floor, Saginaw, Michigan 48604, USA, Tel : +1-989-790-6719, Fax: +1-989-790-9464.
Copyright
© 2021 Miaw TA. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.