Arthroplasty of the Distal Interphalangeal Joint: A Review of Currently Available Surgical Approaches, Implants and Complications
Abstract
Arthroplasty of the distal interphalangeal joint (DIPJ) of the hand is an uncommonly performed and insufficiently researched procedure used to treat painful DIPJ arthritis. This review article investigates the indications, surgical approaches, clinical outcomes and complications of distal interphalangeal joint arthroplasty to address the following questions: (1) Do the factors of surgical approach and implant design affect the clinical outcomes of DIPJ arthroplasty in patients with DIPJ arthritis? (2) Is DIPJ arthroplasty advantageous compared to arthrodesis for treating DIPJ arthritis in terms of clinical outcomes and complications?.
An electronic search of five databases was conducted for articles published from inception until 18 April 2020. Studies published propose that DIPJ arthroplasty using a silicone implant is a viable alternative to arthrodesis, the current standard surgical treatment for DIPJ arthritis. Arthroplasty enables preservation of joint range of motion and improves pain and patient satisfaction; however, there is inadequate evidence to suggest that any particular implant design or surgical approach is superior to other options.
Keywords
Distal interphalangeal joint, Arthroplasty, Arthrodesis
Introduction
Historically, the development of finger arthroplasty can be traced to the early 20th century, prior to which arthrodesis was the most commonly performed procedure to treat severe arthritic conditions of the finger joints [1]. The earliest arthroplasty techniques included resection arthroplasty with various soft tissue interposition techniques, transplant arthroplasty, and Vitallium "cap" arthroplasty for the metacarpophalangeal joint (MCPJ) and proximal interphalangeal joint (PIPJ) [1]. However, such methods were limited by intraoperative technical issues, ambiguous long-term outcomes and poor resultant stability [1].
In 1959, Brannon and Klein introduced a metallic hinged implant for the MCPJ and PIPJ to improve stabilization of the joint [1]. Subsequently, polyethylene-metal prostheses involving a proximal polyethylene stem and a distal metallic stem were developed. Silicone rubber prostheses - the most popular implant design employed in current practice - were created by Swanson in the early 1960's [2]. Since then, newer implants for finger arthroplasty have been designed, such as surface replacement arthroplasty in the 1970's and pyrocarbon arthroplasty in the 1980's [2].
Anatomy of the PIPJ and DIPJ
The anatomical differences in connective tissue around the PIPJ and DIPJ leads to differentiation in surgical approach during arthroplasty. In general, this can be divided into the dorsal and volar approaches. During PIPJ arthroplasty, either dorsal or volar approach can be applied. The dorsal approach enables easier access to the joint, whereas the volar approach has the benefit of enabling earlier post-operative active rehabilitation [3]. Silicone PIPJ arthroplasty with the volar approach is associated with a lower revision rate than silicone or surface replacement arthroplasty with dorsal approaches [3]. For the DIPJ, however, the difference in anatomical structure creates obstacles for the volar approach. All reported surgical cases of DIPJ arthroplasty use a dorsal approach to access the joint. In certain approaches, the extensor tendon which stabilizes the dorsum of the DIPJ is excised transversely [4].
Overall, dorsal approaches allow easier approach to the articular joint without cutting through the volar plate. Incision of the extensor apparatus is usually required, and it is important to preserve its insertion to the phalanx [5]. Once the prosthesis has been implanted, the extensor apparatus should be repaired and restored to a balanced length [5]. In volar approaches, the extensor apparatus can be preserved. However, care should be taken with the vascularization of the volar plate as it is systematically destroyed during the procedure [5].
Treatment options for DIPJ arthritis
Arthritides is the major disease affecting DIPJ function, which includes osteoarthritis (OA), psoriatic arthritis (PsA) and, less commonly, rheumatoid arthritis (RA) [6-8].
Initial treatment for DIPJ arthritis is non-surgical. Options include activity modification, oral anti-inflammatory medication, intermittent corticosteroid injections and splinting [9]. If the patient's condition does not improve with conservative treatment, surgery is indicated [10].
The standard surgical procedure to relieve pain in an arthritic DIPJ is arthrodesis [11]. Indications for DIPJ arthrodesis are pain, instability or deformity [11]. Various techniques may be employed for fixation, including crossed Kirschner wires (K-wire), headless compression wires, pins and tension band, 90-90 wiring, and lateral plate and screw fixation [11]. Fusion rates have been reported to range from 85% to 100% regardless of fixation method [12]. A systematic review reported the union rate of the three most commonly employed techniques - K-wire, interosseus wire and headless compression screw - to be 91.6%, 91.1% and 96.1% respectively [13].
In general, although arthrodesis is durable, stable and predictably eliminates pain, a disadvantage is that it compromises joint range of motion (ROM) and, therefore, causes functional impairment in activities requiring fine manipulation [8]. Moreover, it is associated with complications such as hardware protrusion or migration, loosening, fracture, nonunion or delayed union and angular deformity [11].
Arthroplasty is an alternative, albeit a much less commonly performed, treatment option that enables retention of DIPJ motion and preservation of joint function. Few reports in the literature have evaluated the long-term outcomes of DIPJ arthroplasty. It may be offered in patients with symptomatic arthritis not controlled by other non-operative means, good bone stock and soft tissues, and who prefer to preserve some motion in the affected joints [11].
The predilection for arthrodesis over arthroplasty may be attributed to the belief that the DIPJ has low bone stock and limited need for motion, thus rendering arthroplasty unnecessary or considered only in exceptional circumstances [4]. However, the loss of terminal finger flexion and fine control may be less tolerated in young patients or may be restrictive in patients with multiple digit involvement [10]. Considering the functional benefits of a mobile DIPJ in facilitating pinch, grip and grasp, DIPJ arthroplasty may be a preferred option for suitable candidates.
Compared to arthroplasty of its counterpart PIPJ, DIPJ arthroplasty is an understudied intervention with no consensus on the indications, optimal surgical approach and ideal implant design. Reasons for this phenomenon include the small dimension of bone at the DIPJ, complicated bone anatomy and difficulties in surgical operation. Additionally, it is uncertain whether DIPJ arthroplasty or arthrodesis is superior in terms of clinical outcomes and complications.
This review analyzes the topic of DIPJ arthroplasty to address the following questions: (1) Do the factors of surgical approach and implant design affect the clinical outcomes of DIPJ arthroplasty? (2) Is DIPJ arthroplasty advantageous compared to arthrodesis for treating DIPJ arthritis in terms of clinical outcomes and complications? This is achieved by summarizing the available evidence regarding the following: (1) DIPJ arthritis and treatment options; (2) Indications for DIPJ arthroplasty; (3) Surgical approach; (4) Implant design; (5) Clinical outcomes; (6) Complications; (7) Considerations for choice of treatment; (8) Directions for future research.
Materials and Methods
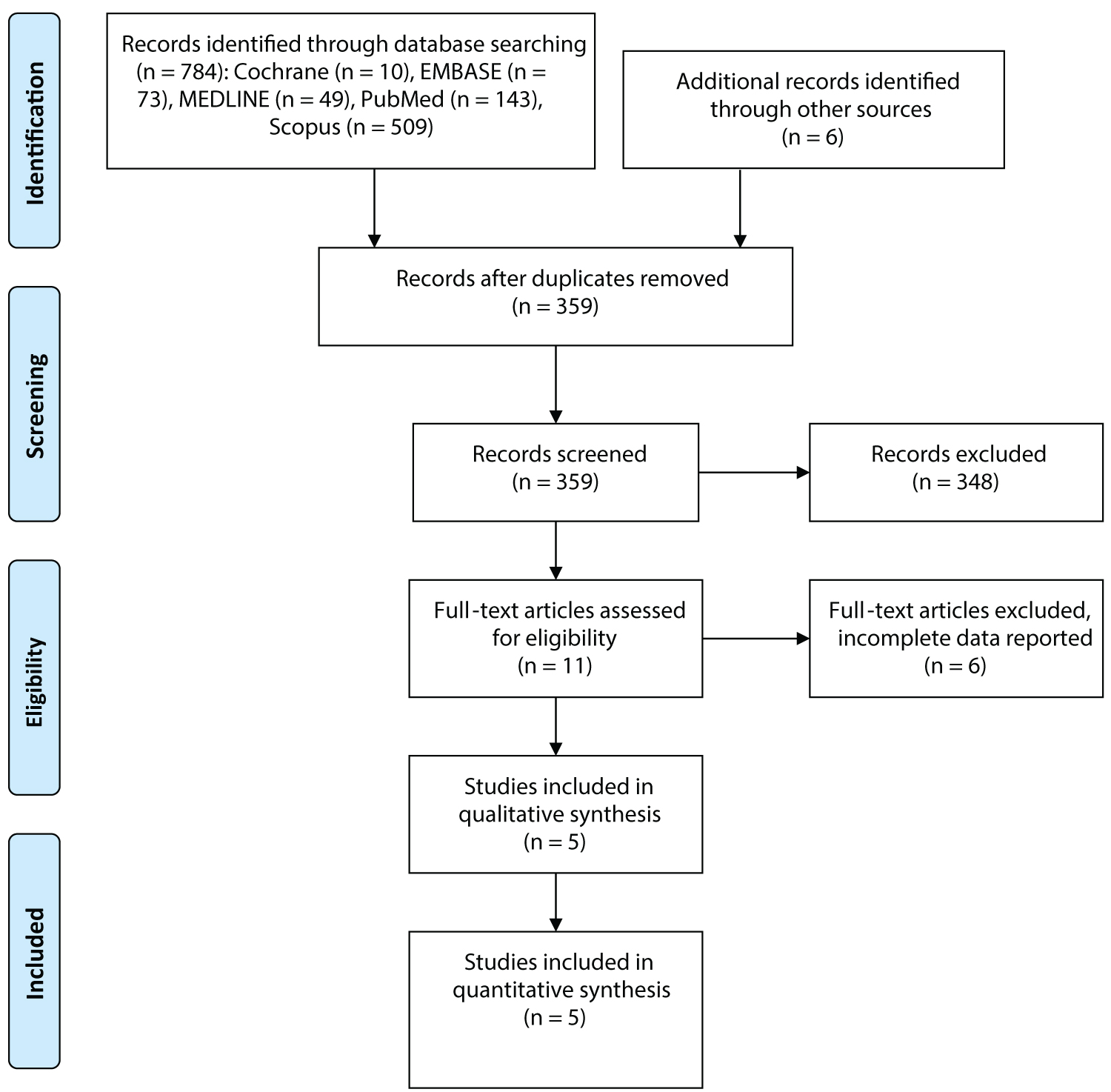
This was a narrative review in which an electronic search of five databases (PubMed, EMBASE, MEDLINE (Ovid), The Cochrane Central Register of Controlled Trials (CENTRAL, The Cochrane Library, Latest Issue) and Scopus) was conducted for articles reporting on outcomes of DIPJ arthroplasty published from inception until 18 April 2020. Details of the study identification and selection process are presented in Figure 1. Search terms included "arthroplasty," "distal interphalangeal" and "finger" and related synonyms. There were no language restrictions. Reference lists of relevant articles were surveyed for further articles.
Selection of articles for inclusion in this review was based on pertinence to the clinical management of DIPJ arthritis and potential impact on the practice of DIPJ arthroplasty. Animal and cadaveric studies, studies without DIPJ arthroplasty, and studies that failed to report the type of implant, joint pathology and clinical outcomes were excluded.
All included studies were assessed for study characteristics (i.e. year of publication, study design, type of implant), patient demographics (i.e. number of patients, average age), finger demographics (i.e. number of joints, finger distribution, joint pathology), average follow-up period, clinical outcomes (i.e. pain, patient satisfaction, joint ROM, extensor lag), complications and revision rate.
Results
Patient demographics
Of the 784 records identified through the searched databases, five articles reported the clinical outcomes of DIPJ arthroplasty. Study characteristics are summarized in Table 1. There was one prospective cohort study, one case report and three case series. A total of 192 DIPJ in 121 patients underwent DIPJ arthroplasty. Mean age at surgery was 62.4 years. The index finger was most commonly operated on, followed by the third, fourth and fifth fingers respectively. The mean follow-up period was 39.4 months.
Indications for DIPJ arthroplasty
Among the studies included in this review, the underlying diagnosis was osteoarthritis except for one rheumatoid arthritis joint [10] and two post-traumatic joints [4]. All reported pain in the DIPJ as an indication for arthroplasty. Additional indications include DIPJ deformity, instability, decreased functional ability, concern for appearance and desire to retain some motion of the DIPJ [4,10,14-16]. A case report on a musician noted the need to retain finger mobility for instrument-playing function as an indication for arthroplasty as opposed to arthrodesis [16]. One study offered arthroplasty solely to DIPJ which retained a degree of movement - other joints which had limited movement were managed with non-surgical means or joint fusion instead [4].
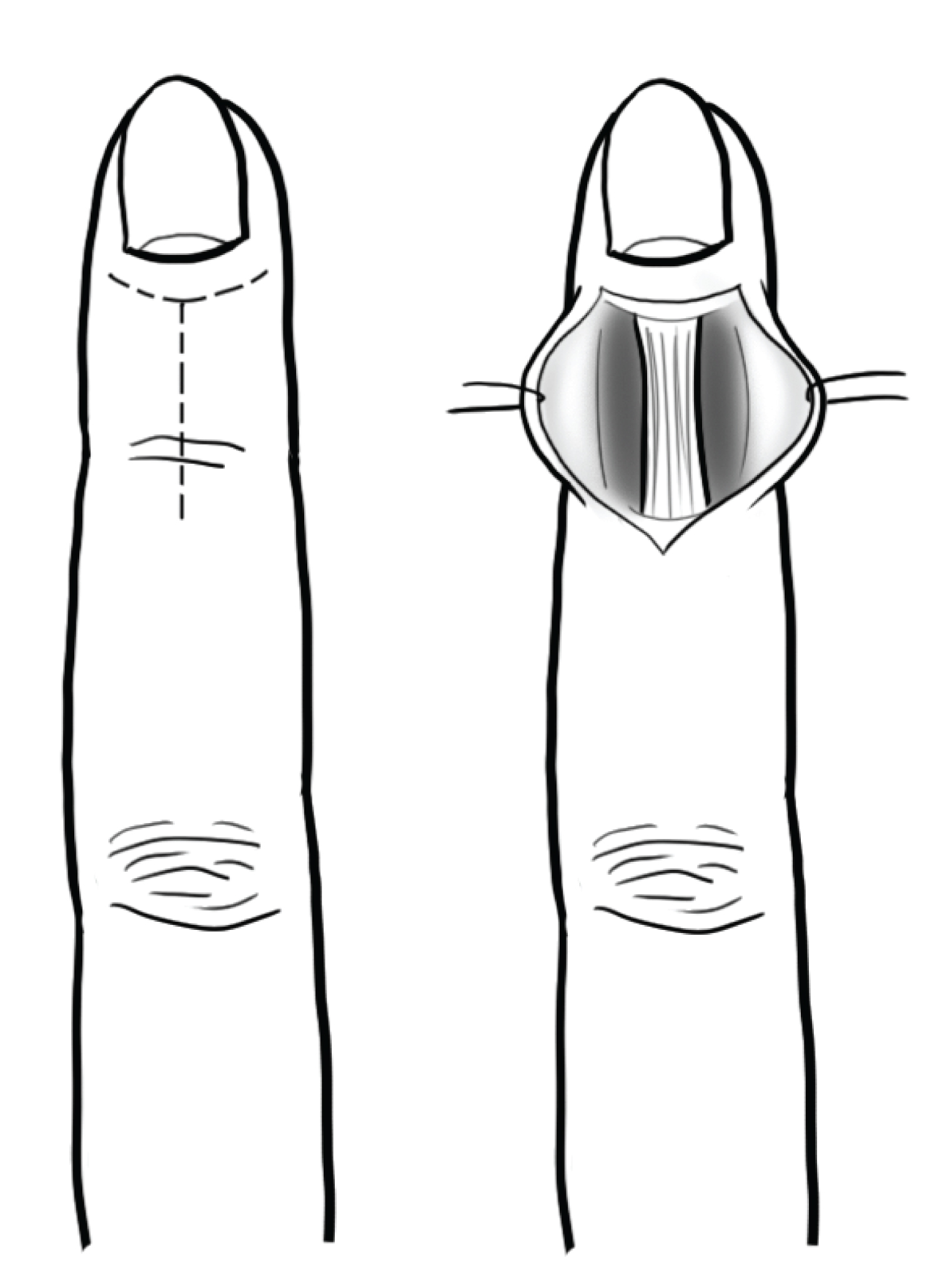
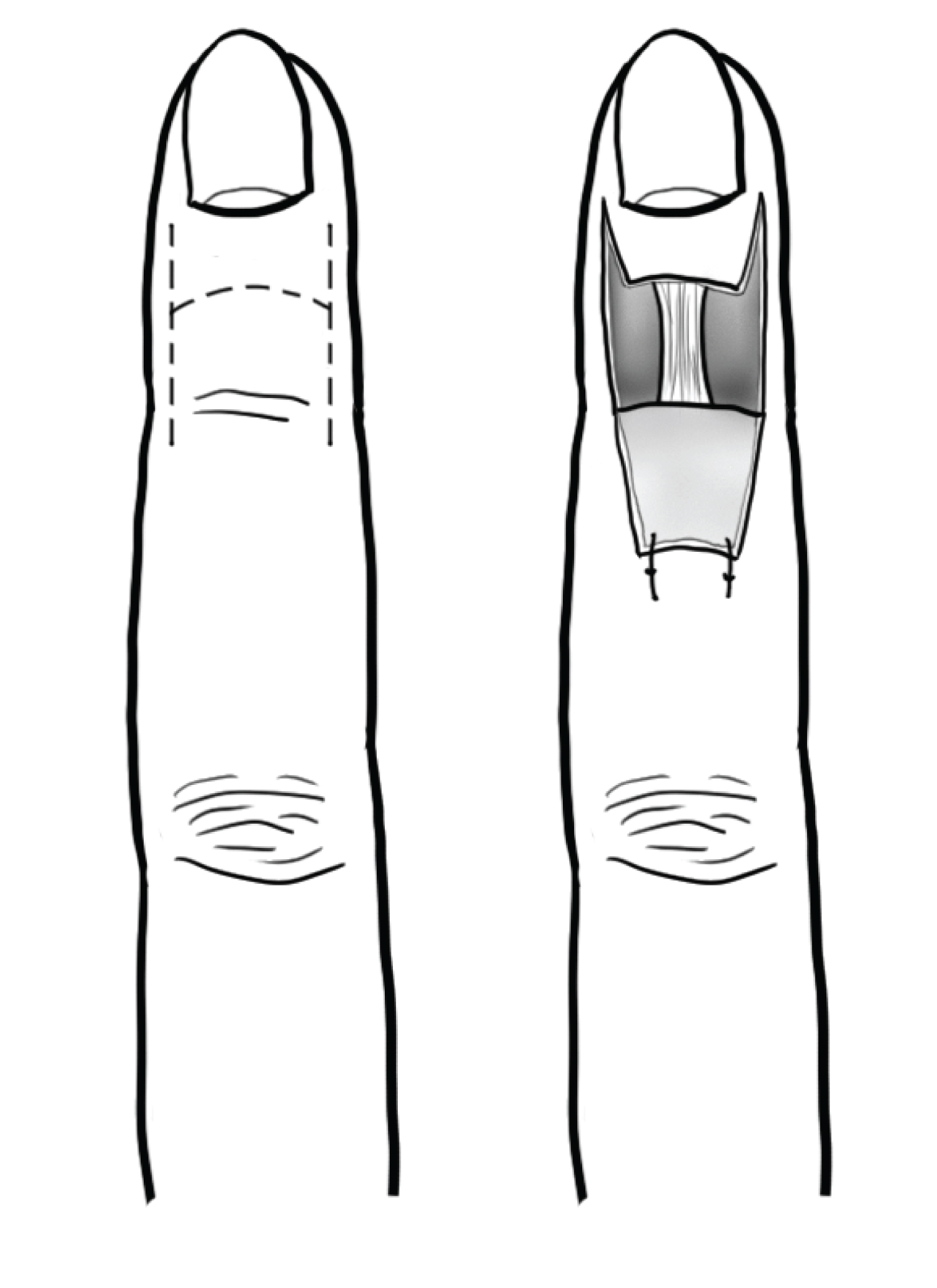
Surgical approaches
All reported cases of DIPJ arthroplasty adopted a similar surgical approach. A dorsal T-shaped (Figure 2) or H-shaped (Figure 3) or modified radial Kilgore incision was used to approach the joint. The extensor tendon was excised transversely approximately 5 millimetres proximal to its insertion into the distal phalanx. The collateral ligaments were either divided at their insertion to the proximal phalanx [4,14] or preserved [10]. Marginal osteophytes were debrided from the joint using a rongeur. The head of the middle phalanx was removed using an oscillating saw, and the intramedullary canals of the distal and middle phalanges were prepared for insertion of the implant via a "no touch" technique. The extensor tendon was repaired with an absorbable or nonabsorbable suture and the wound was closed. One study inserted a Kirschner wire retrograde through the distal phalanx of each patient [10]. Another study reported that the joint was pinned into position but did not specify the technique or tool used [16]. A splint or plaster cast was applied for three to eight weeks and active DIPJ exercises were encouraged.
Sierakowski developed a new extensor-sparing technique which left the extensor tendon intact [4]. The middle and distal phalanges were accessed by laterally flexing the joint and retracting the extensor tendon side-to-side with a tendon hook. A rongeur was used instead of a saw to remove the distal end of the middle phalanx in order to protect the extensor tendon. An advantage of this technique is that joint mobilization can be initiated from the first postoperative day, compared to after several weeks of strict immobilization using the standard technique. However, the study found no significant difference in the range of movement or reduction of extensor lag with either technique [4].
Clinical outcomes
All reported cases employed silicone implant for the joint replacement operation. Clinical outcomes of DIPJ arthroplasty are listed in Table 2. For patient-reported outcomes, all but one study reported improvement in pain and patient satisfaction with their digit compared to their preoperative status. The postoperative range of motion of the joint ranged from 30° to 45°. Only one study measured preoperative range of motion and found a 15° mean gain in joint range of movement [4]. Studies also reported improved grip strength [15], power, dexterity, cosmetic appearance, alignment and stability to lateral stress [10,15,16]. In the two studies which recorded extensor lag of the digit, one study found a 9° reduction in extensor lag to 11° from the preoperative mean of 20°, whereas the other study reported the mean postoperative extensor lag to be 12.7° [4,10].
Complications
Complications were reported in two studies. The complication rate was 5% and 9.7% respectively [4,10]. Complications included cellulitis, osteomyelitis, deformity, instability, implant erosion and fracture. Meanwhile, the revision rate in the same two studies was 3% and 9.7% respectively [4,10]. Of the seven joints in total which required revision surgery, four joints received revision to arthrodesis and the other joints underwent implant removal, resectional arthroplasty, or correction of a mallet-type finger deformity [4,10].
Discussion
In this narrative review, silicone DIPJ arthroplasty performed via a dorsal approach was predominantly indicated for pain of the DIPJ due to underlying osteoarthritis. DIPJ arthroplasty showed improvement in patient-reported outcomes including pain and patient satisfaction. Studies also reported benefits to functional outcomes in terms of DIPJ range of motion, grip strength, power, dexterity, cosmetic appearance, alignment, stability to lateral stress and extensor lag. On the other hand, DIPJ arthroplasty was associated with a number of complications, a proportion of which required reoperation and revision. However, results should be interpreted with caution due to the lack of studies available and the poor quality of evidence arising from retrospective case series.
Implants
Although there was scarce data on outcomes of implant arthroplasty on the DIPJ and no articles on alternative implant designs apart from silicone, there is extensive literature on PIPJ arthroplasty using silicone and other implants. A variety of implants are available for PIPJ arthroplasty, the most popular being silicone arthroplasty, surface replacement arthroplasty (SRA) and pyrocarbon arthroplasty. Future adaptions of these designs in DIPJ are possible. The following is a summary of these implants.
Silicone implants, first introduced for joint replacement by Swanson in 1962, have the longest history and are regarded as the standard choice for small joint arthroplasty. It is a constrained single implant arthroplasty with a hinge element and flexibility that allows motion in multiple planes but not to the extent of native joint articulation (Figure 4) [2]. To address this limitation, the surface replacement arthroplasty was developed. SRA is an unconstrained implant that aims to restore the full, functional range of motion of the native joint while preserving bone stock and collateral ligaments for stability [2]. The most commonly used materials of SRA implants are a proximal cobalt chromium alloy component coupled with a distal ultra-high molecular-weight polyethylene component. More recently, a PIPJ implant made of pyrolytic carbon was developed. Compared to metals and polymers, pyrolytic carbon is supposedly more wear-resistant and durable as it does not degrade by cyclic loading and can withstand large amounts of elastic strain without deformation [2].
A systematic review of different PIPJ arthroplasty implants and surgical approaches found that the silicone implant had the greatest mean gain in joint range of motion, less postoperative extension lag and the lowest revision rate among all implant designs [3]. Another review showed that PIPJ silicone implants required fewer reoperations than pyrocarbon and metal-polyethylene implants, but had a higher rate of finger deviations and instabilities [17]. Revision rates for silicone arthroplasty with a volar, lateral or dorsal approach were reported to be 13%, 10% and 11% respectively, compared to SRA with a volar or dorsal approach which had higher revision rates of 17% and 18% [3]. Primary indications for revision of silicone PIP arthroplasty were breakage, continued pain, infection, implant loosening, decreased range of motion, bony block, instability and synovitis [18]. Implant fracture is also common, with fracture rates of up to 30% after 6.5 years [17]. However, a fractured silicone implant does not necessarily cause joint pain or instability that warrants revision surgery; and the long-term survivorship (8-10 years) of silicone implants remains high at a reported rate between 80% and 90% [2], considerably higher than surface replacing implants [17]. A systematic review found no significant difference in implant-related complications between silicone, pyrocarbon and metal-polyethylene implants [17].
Therefore, existing articles on PIPJ arthroplasty establish silicone implants as a popular option associated with increased postoperative joint range of motion, high survival rate and low revision rate. Further clinical studies are required to assess whether silicone arthroplasty confers similar benefits to the DIPJ. However, alternatives to silicone implants (including SRA) may be advantageous in other aspects, such as by causing less joint instability and deviation or fewer implant fractures, as suggested by PIPJ arthroplasty studies. For the DIPJ, approaches such as excisional arthroplasty with soft tissue interposition and cheilectomy have also been proposed as techniques that preserve joint motion [19,20]. The studies included in this review exclusively performed silicone DIPJ arthroplasty, thus more research is needed on the outcomes and complications of other implants and approaches to DIPJ arthroplasty.
Complications of DIPJ arthrodesis
The current standard surgical treatment for DIPJ arthropathy - DIPJ arthrodesis - is not without complications. DIPJ arthrodesis with Kirschner wires, 90-90 interosseus wires and compression screw techniques has a reported non-union rate of 3% to 15% [18]. A systematic review reported the malunion rate of K-wire, interosseus wire and headless compression screw to be 3.5%, 1.5% and 0.5% respectively [13]. Statistical analysis revealed significantly increased union rate with the headless compression screw compared to K-wire and interosseus wire [13]. However, headless compression screws cost significantly more than K-wires and are associated with unique complications such as nail abnormalities, fracture and screw cut-through [13].
Another review of 144 DIPJ arthrodeses using various fixation methods found that the rate of non-union was 12%; minor complications (stiffness, paresthesias, superficial infection, skin necrosis and cold intolerance) was 16%; and major complications (osteomyelitis, non-union, deep infection, mal-union) was 20% [21]. In particular, patients with psoriatic arthritis had the highest complication rate (44%) [21]. In contrast, the complication rate for DIPJ arthroplasty on primarily osteoarthritic joints was 5% and 9.7% in two separate studies [4,10].
Regarding the need for revision surgery following DIPJ arthrodesis, a case series on 64 DIPJ arthrodesis using the Herbert headless compression screw reported a revision rate of 12.5% [18], compared to 3% and 9.7% in DIPJ arthroplasty as reported by two separate studies [4,10]. Further research comparing the outcomes and revision rates of DIPJ arthrodesis versus arthroplasty is needed.
Study limitations
Although studies on the outcomes and complications of DIPJ arthroplasty included in this review have suggested that this procedure is an acceptable alternative to arthrodesis, there are a number of limitations to the existing literature. Firstly, few articles investigating DIPJ arthroplasty have been published, most of which were retrospective case series of Level 4 evidence that risk having selection bias. The small sample size was mainly restricted to DIPJ osteoarthritis patients, limiting the external validity of results to other DIPJ pathologies such as inflammatory or post-traumatic arthropathy. The various conditions affecting the DIPJ may cause considerable differences in bone stock, bone quality and soft tissue envelope which may influence surgical outcomes and complications [13].
Moreover, arthroplasty in the DIPJ is a less investigated topic. Only silicone implants were subject to investigation and no tailor-made prosthesis for the joint has been developed. As suggested by literature on PIPJ arthroplasty, other techniques including pyrocarbon and metal-polyethylene implants may offer advantages such as reduced finger deviation and greater stability [17]. It may be worthwhile to compare DIPJ silicone arthroplasty to other implant designs in future studies.
Incomplete data reporting was another limitation of existing literature on DIPJ arthroplasty. Most studies failed to conduct preoperative evaluation of outcomes such as joint range of motion, extensor lag and pain status. Outcome parameters and assessment tools were also inconsistent across studies and most failed to report standard errors or deviations, thus prohibiting further statistical analysis.
Furthermore, although arthroplasty for the PIPJ is well established and complication rates of the silicone design may be comparable to that of the DIPJ, it is uncertain whether reported outcomes for PIPJ arthroplasty are generalizable to the DIPJ. Similarities between the normal PIPJ and DIPJ have been described, albeit in general terms only. These include their hinge joint structure, asymmetric bicondylar proximal articular surfaces, intercondylar ridges and concavities of the distal articular surfaces, and concavities and tubercles for the attachment of ligaments [6]. In addition to structural differences between normal DIPJ and PIPJ, disease conditions also have variable pathological effects on the bone, cartilage and soft tissues of the DIPJ and PIPJ [7]. Moreover, the DIPJ and PIPJ are subjected to different forces and stresses when performing various activities. The specific loading patterns of the DIPJ and PIPJ may influence which arthroplasty approach is most appropriate for each joint. Therefore, anatomical, pathological and biomechanical differences between the DIPJ and PIPJ may prevent findings for implants on the PIPJ from being generalized to the DIPJ. The architecture and biomechanics of the PIPJ and DIPJ in both their normal and pathological states require further investigation, in addition to long-term studies on implant arthroplasty specific to the DIPJ.
Considerations for treatment options
The choice between arthrodesis and arthroplasty for treating DIPJ arthritis depends on factors beyond those taken into account in the studies included in this review (such as postoperative range of motion, pain and complication rate). Some argue that DIPJ arthroplasty is unnecessary because preservation of motion in this joint is not as important as other joints in the hand [11]. The DIPJ produces 15% of intrinsic digital flexion, but contributes only 3% to the overall flexion arc of the finger (compared to the PIPJ which produces 85% and 20% of intrinsic and overall digital flexion respectively) [22]. However, simulated DIPJ fusion was associated with a 20% to 25% decrease in grip strength compared to the preoperative state [22]. Despite the theoretically negligible impairment of hand function caused by DIPJ arthrodesis compared to PIPJ arthrodesis, patients with DIPJ arthritis may nonetheless prefer arthroplasty to minimize functional deficits.
In addition to the functional outcomes of the procedure, joint factors and other patient parameters may preclude a patient from undergoing either arthrodesis or arthroplasty. Pre-existing joint deformity and instability, such as in patients with an erosive and inflammatory type of osteoarthritis, have been regarded as reasons to consider arthrodesis over arthroplasty, at least for the PIPJ [23]. Other bone and soft tissue factors including the presence of bone defects or cysts, insufficient bone stock, missing or dysfunctional tendons and severe tendon imbalance may favour arthrodesis [23]. For PIPJ arthroplasty which has more implant options than the DIPJ, silicone implants can be used even in patients with limited bone stock and can be performed by surgeons with limited surgical experience; whereas more complex, two-component uncemented implants require adequate bone stock and no large cystic defects, and is a relatively more challenging procedure [23]. Future research on different DIPJ implants may similarly find that multiple joint factors influence decision-making on surgical treatment. Finally, patients' concern for the aesthetic outcome and surgical cost may contribute to the treatment choice.
Future Research
This review reveals DIPJ arthroplasty to be an understudied field. More long-term prospective randomized controlled trials with larger sample sizes are required to evaluate whether DIPJ arthroplasty is an acceptable alternative to the traditional arthrodesis procedure. The outcomes of silicone and other types of DIPJ prosthesis, and various surgical approaches, should be compared in DIPJ affected by different forms of arthritis. Comprehensive reporting of patient characteristics, surgical and rehabilitation protocol, and preoperative and postoperative outcomes are required, with validated assessment tools used to measure subjective and objective variables. Standardized definitions of outcomes and complications would also enable comparisons to be made.
Conclusion
Existing studies suggest that DIPJ arthroplasty using a silicone implant can improve pain and patient satisfaction while preserving joint range of motion in patients with painful DIPJ arthritis. Thus, DIPJ arthroplasty may serve as an alternative to arthrodesis. However, studies investigating DIPJ arthroplasty and its outcomes were scarce, had small sample sizes, flaws in study designs and incomplete data reporting; hence, no conclusions can be made regarding the indications and optimal implant design or surgical approach for DIPJ arthroplasty. In future studies, these methodological aspects must be refined in order to gather robust evidence regarding the efficacy and safety of different implants and surgical techniques for DIPJ arthroplasty.
Conflict of Interest
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributions
E.C.: Wrote the manuscript and performed the data collection and analysis; V.C.: Designed the figures and revised the manuscript; Y.L. and I.W.: Revised the manuscript and supervised the project.
All authors read and approved the final manuscript.
References
- Berger RA (1989) A brief history of finger arthroplasty. The Iowa Orthopaedic Journal 9: 77-82.
- Zhu AF, Rahgozar P, Chung KC (2018) Advances in proximal interphalangeal joint arthroplasty: Biomechanics and biomaterials. Hand Clinics 34: 185-194.
- Yamamoto M, Chung KC (2019) Joint fusion and arthroplasty in the hand. Clinics in Plastic Surgery 46: 479-488.
- Sierakowski A, Zweifel C, Sirotakova M, et al. (2011) Joint replacement in 131 painful osteoarthritis and post-traumatic distal interphalangeal joints. The Journal of Hand Surgery 37: 304-309.
- Rongieres M (2013) Surgical treatment of degenerative osteoarthritis of the fingers. Chirurgie de la Main 32: 193-198.
- Kaufmann RA, Logters TT, Verbruggen G, et al. (2010) Osteoarthritis of the distal interphalangeal joint. The Journal of Hand Surgery 35: 2117-2125.
- Tan AL, Grainger AJ, Tanner SF, et al. (2006) A high-resolution magnetic resonance imaging study of distal interphalangeal joint arthropathy in psoriatic arthritis and osteoarthritis: Are they the same? Arthritis & Rheumatism 54: 1328-1333.
- Jacob S (2018) Arthroplasty of the hand and wrist. In: Borrelli J, Anglen JO (Edn), Arthroplasty for the treatment of fractures in the older patient: Indications and Current Techniques. 91-126.
- Ting BL, Simmons BP (2021) Hand and wrist osteoarthritis. In: Katz JN, Blauwet CA, Schoenfeld AJ (Edn), principles of orthopedic practice for primary care providers. 231-249.
- Zimmerman NB, Suhey PV, Clark GL, et al. (1989) Silicone interpositional arthroplasty of the distal interphalangeal joint. The Journal of Hand Surgery 14A: 882-887.
- Nikac V, Blazar P, Earp B, et al. (2017) Radiographic and surgical considerations in arthritis surgery of the hand. Skeletal Radiology 46: 591-604.
- Wu JC, Calandruccio JH, Weller WJ, et al. (2019) Arthritis of the thumb interphalangeal and finger distal interphalangeal joint. Orthopedic Clinics of North America 50: 489-496.
- Dickson DR, Mehta SS, Nuttall D, et al. (2014) A systematic review of distal interphalangeal joint arthrodesis. Journal of Hand and Microsurgery 6: 74-84.
- Snow JW, Boyes JG, Greider JL (1977) Implant arthroplasty of the distal interphalangeal joint of the finger for osteoarthritis. Plastic & Reconstructive Surgery 60: 558-560.
- Brown LG (1989) Distal interphalangeal joint flexible implant arthroplasty. The Journal of Hand Surgery 14: 653-656.
- Schwartz DA, Peimer CA (1998) Distal interphalangeal joint implant arthroplasty in a musician. Journal of Hand Therapy 11: 49-52.
- Forster N, Schindele S, Audige L, et al. (2018) Complications, reoperations and revisions after proximal interphalangeal joint arthroplasty: A systematic review and meta-analysis. Journal of Hand Surgery 43: 1066-1075.
- Satteson ES, Langford MA, Li Z (2015) The management of complications of small joint arthrodesis and arthroplasty. Hand Clinics 31: 243-266.
- Aslam MZ, Ahmed SK, Fung B (2015) New technique: Tendon interposition arthroplasty in distal interphalangeal joint arthritis in chinese population -new horizon for treatment. Journal of the Pakistan Medical Association 65: S8-S11.
- Lin EA, Papatheodorou LK, Sotereanos DG (2017) Cheilectomy for treatment of symptomatic distal interphalangeal joint osteoarthritis: a review of 78 patients. The Journal of Hand Surgery 42: 889-893.
- Fowler JR, Baratz ME (2014) Distal interphalangeal joint arthrodesis. The Journal of Hand Surgery 39: 126-128.
- Baltzer HL, Moran ST (2016) The biomechanical impact of digital loss and fusion following trauma: Setting the patient up for success. Hand Clinics 32: 443-463.
- Herren DB (2017) Current European practice in the treatment of proximal interphalangeal joint arthritis. Hand Clin 33: 489-500.
Corresponding Author
Evelyn Hui Yi Chan, Department of Orthopaedics & Traumatology, The University of Hong Kong, Hong Kong
Copyright
© 2021 Chan EHY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.