Surgical Hip Dislocation for the Treatment of Slipped Upper Femoral Epiphysis - Demonstration of Surgical Technique
Surgical hip dislocation for treatment of hip intra-articular pathology has been popularized by the Bernese group over the last few years. This approach provides excellent and safe exposure of the hip joint without compromising the femoral head blood supply. It is, however a very demanding approach and requires surgical experience and attention to detail.
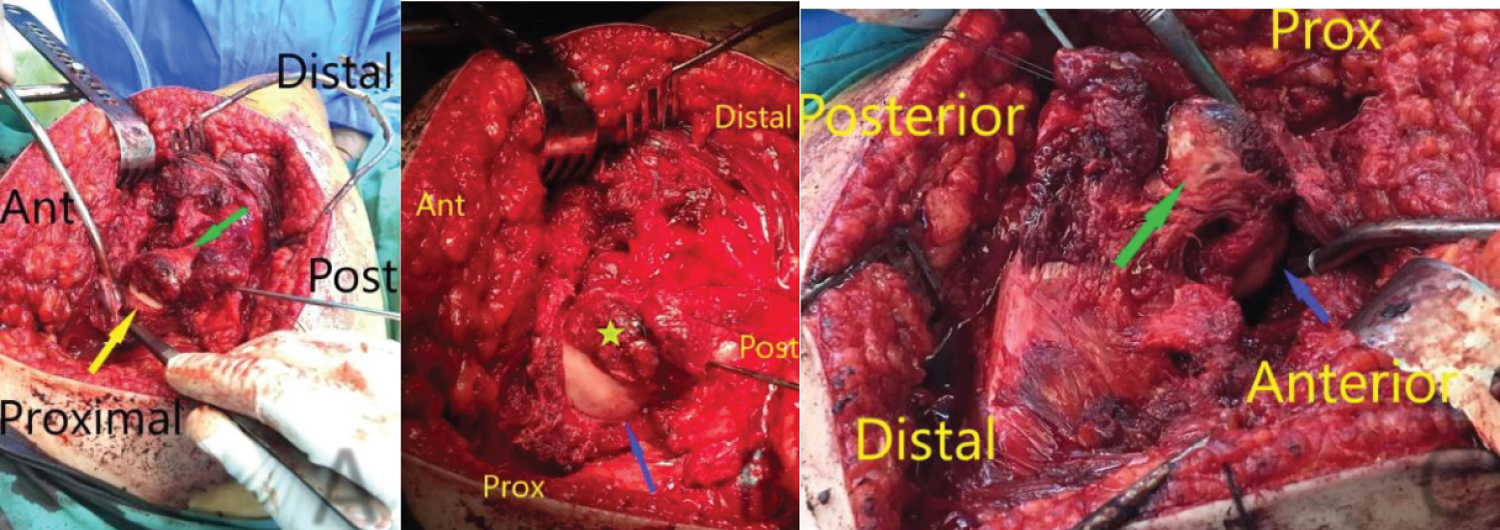
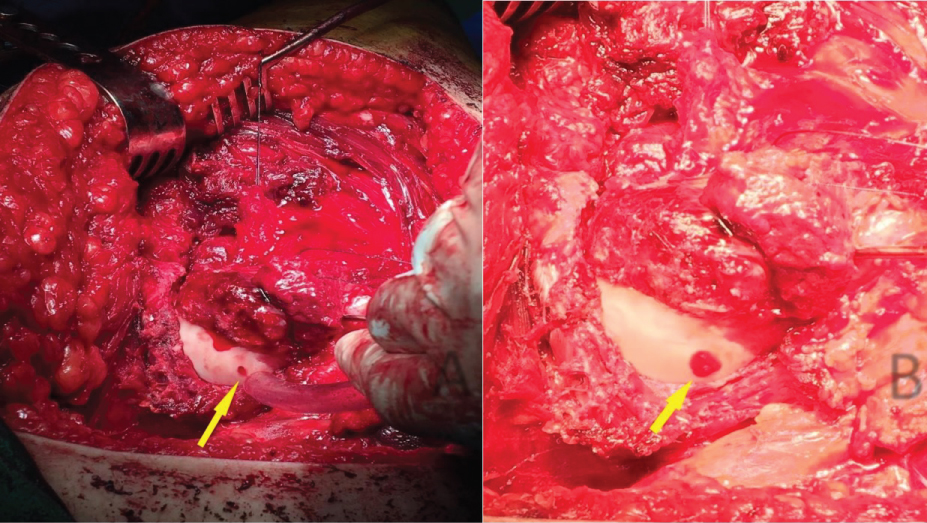
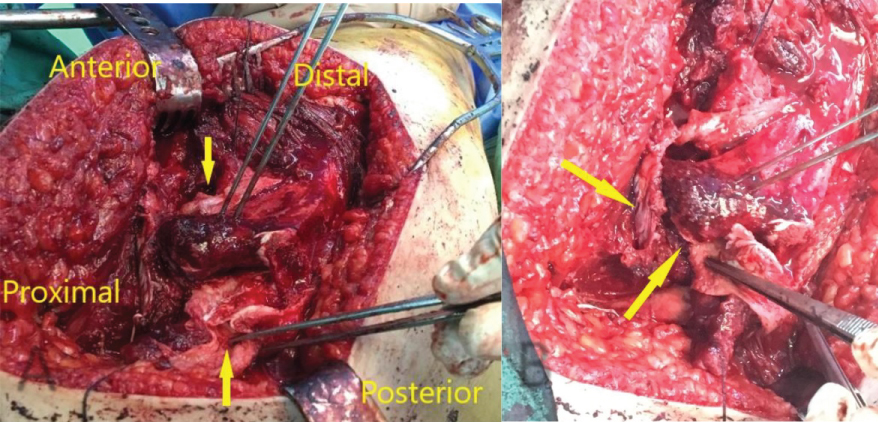
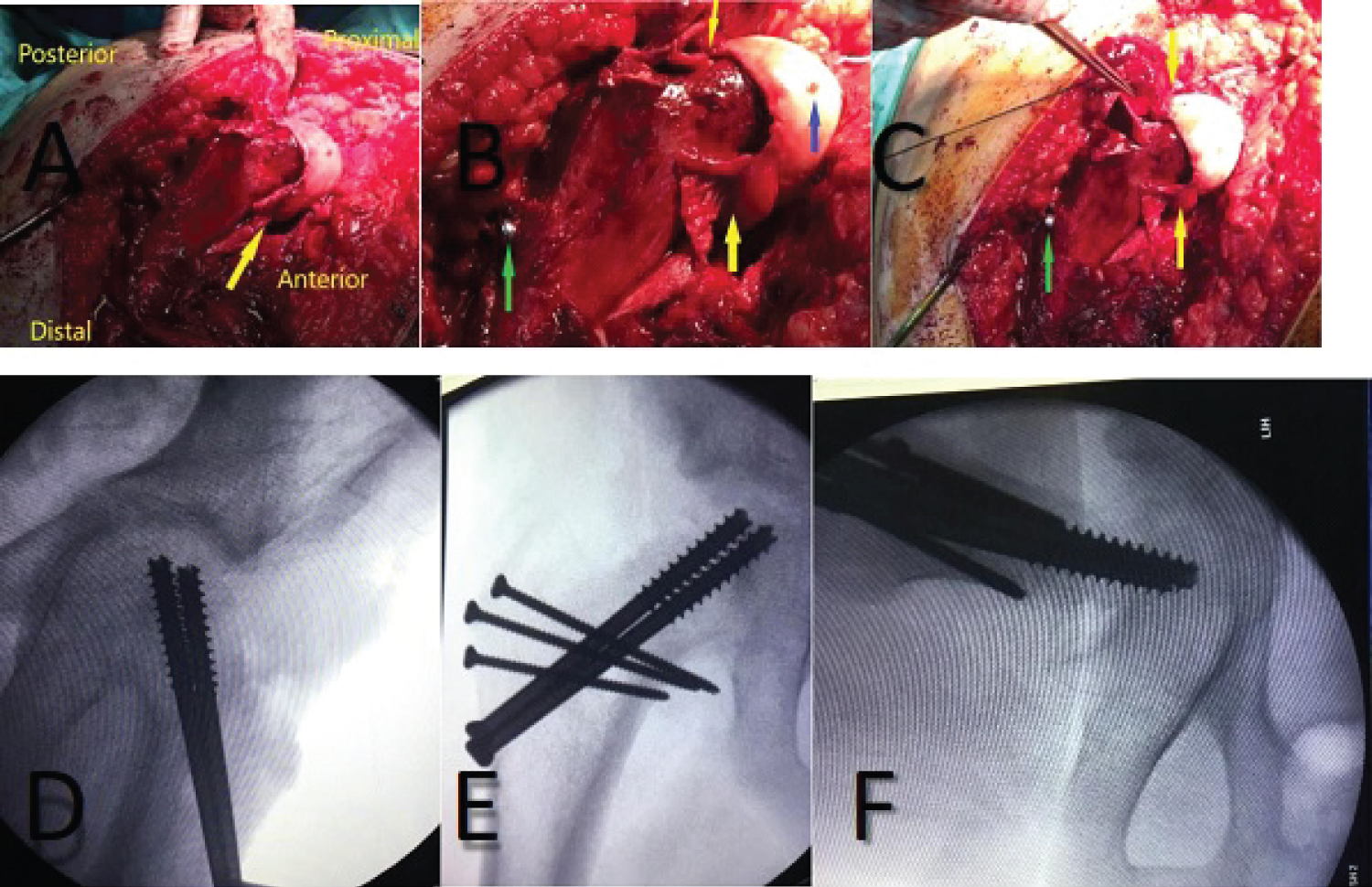
Surgical hip dislocation for treatment of severe cases of Slipped Upper Femoral Epiphysis (SUFE) is even more technical and has few more steps. Severe slips, by definition, can compromise the blood supply and therefore special care must be taken to maintain the remaining vascularity of the femoral head. In this article we will demonstrate in detail the same approach described by Ganz, et al. going through all the surgical steps and demonstrating those using intra-operative photos. The aim of this article is to make the approach clearer to orthopaedic surgeons dealing with this complex problem.
Introduction
Slipped Upper Femoral Epiphysis (SUFE) affects about 1 in 100,000 children [1]. It is usually a disease of the adolescence but can affect younger children occasionally. The condition varies in severity and in chronicity. In situ pinning has been traditionally labelled as the gold standard for treatment of all cases regardless of the severity of the slip [2]. In situ pinning seems to give good results for mild and may be moderate slips. However, bad results have been reported for severe slips and subsequent surgeries did not seem to resolve patients' complains [3]. Many of these patients continue to suffer and require arthroplasty at a very young age. Furthermore, in situ pinning is not necessarily an easy operation in severe slips and some complications have been reported such as chondrolysis, fractures, avascular necrosis etc. in addition to the arguable remodeling potential of the proximal femur after slippage of the femoral head [2,4].
Other treatment options included reductions; closed or open and osteotomies. Closed reductions are not advised in most cases due to the very significant of disrupting the remaining blood supply which will inevitably lead to avascular necrosis. Basal neck and inter-trochanteric osteotomies are technically easier to do but are farther away from the CORA and lead to non-anatomical correction and a further deformity especially in severe slips [5]. Intra-articular osteotomies to achieve a reasonable reduction are more demanding and carry higher risk of avscaular necrosis but in principle correct the original deformity and can achieve better results [4]. The slip site can be approached via an anterior approach e.g. Fish Osteotomy but full access is not possible especially to the posterior aspect of the neck where the slipped femoral head is lying, and anatomical reduction is difficult and carries a very high incidence of AVN. The original Dunn osteotomy utilizes a posterior KockerLangenbeck approach which is slightly better but the created retinacular flaps are short which limits the access and the reduction and again risks the development of AVN.
The concept of 'Safe Surgical Hip Dislocation' was introduced by Ganz, et al. in order to directly visualize and deal with intra-articular hip pathology without compromising the vascularity of the femoral head [6,7]. The Bernese group initially published their technique of dislocating the hip joint after performing an anterior Z-shaped capsulotomy to protect the blood supply. Subsequently the same group described the same approach to perform the 'modified Dunn osteotomy' to treat severe slips [4,8]. We noticed that most surgeons are very hesitant to perform this approach because of its technicalities. In this article we will explain and demonstrate with intra-operative photos all steps of the approach hoping to clarify it for orthopaedic surgeons who deal with such cases.
Materials and Methods
We present one of our patients who presented to our department with severe SUFE and who required the modified Dunn procedure through the Ganz Safe surgical dislocation approach. We will present the initial radiological examinations and then go through the operation step by step and demonstrateeach step with intra-operative photos.
Case Presentation
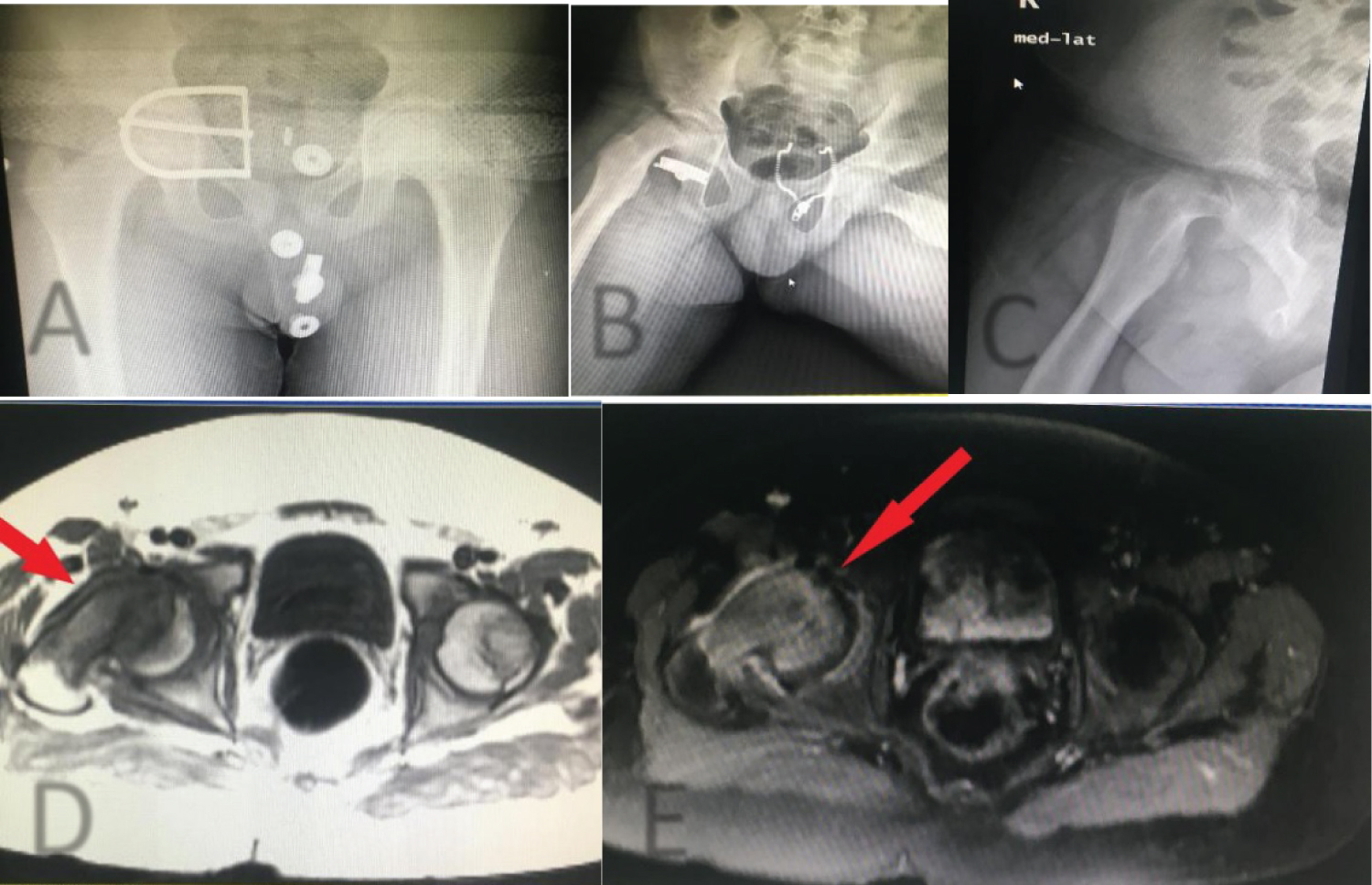
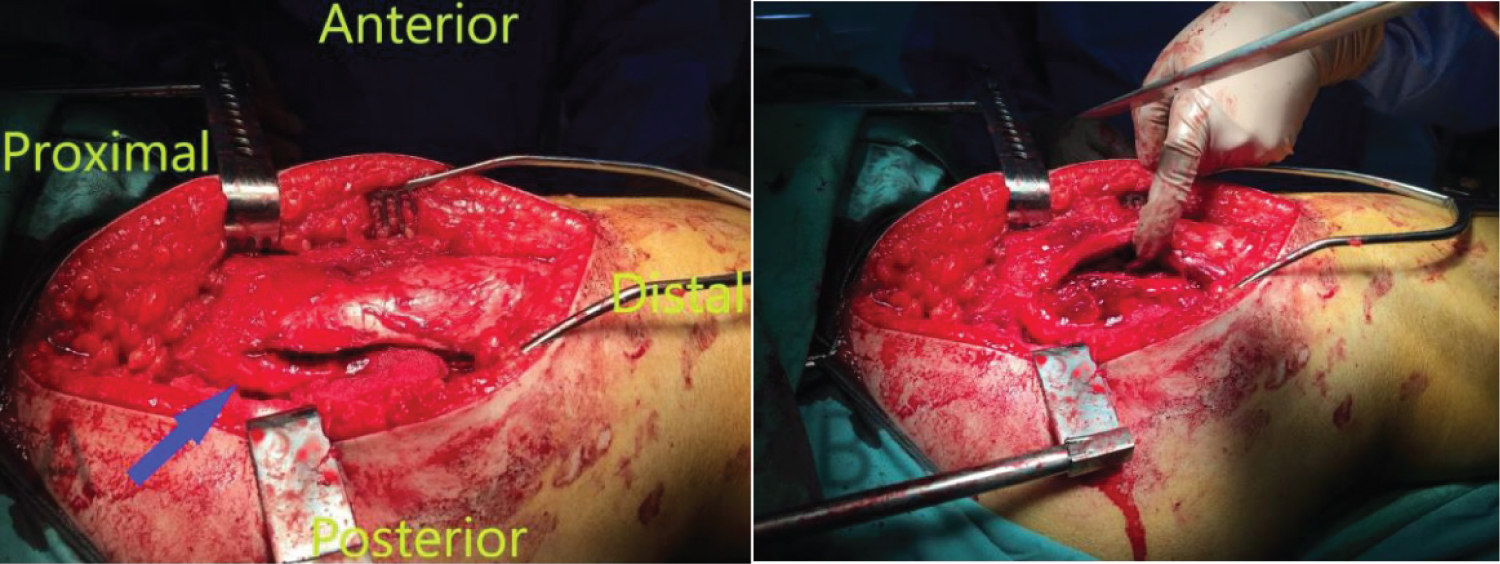
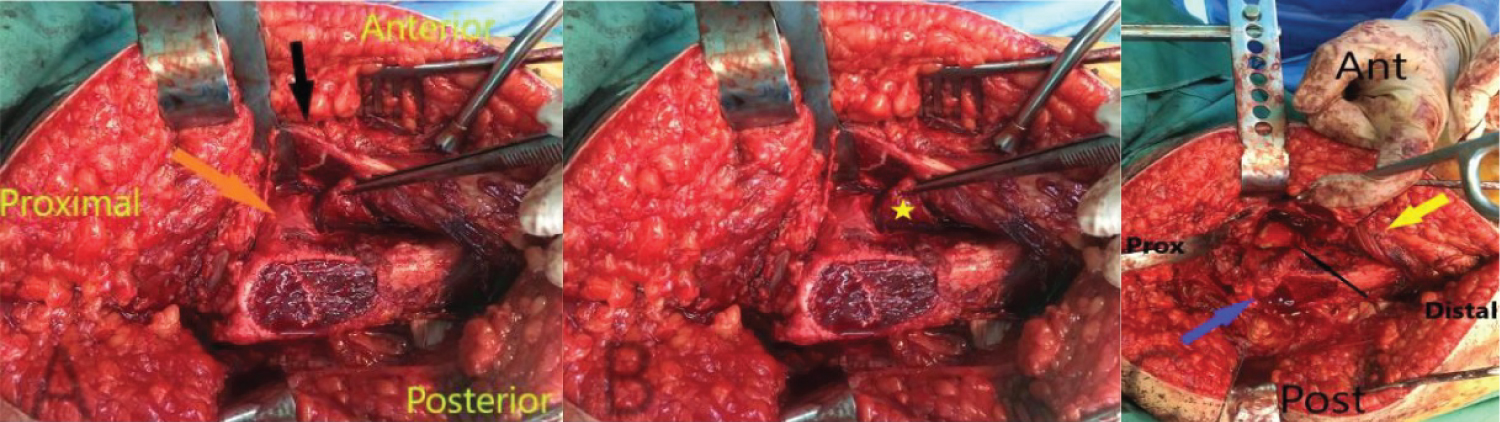
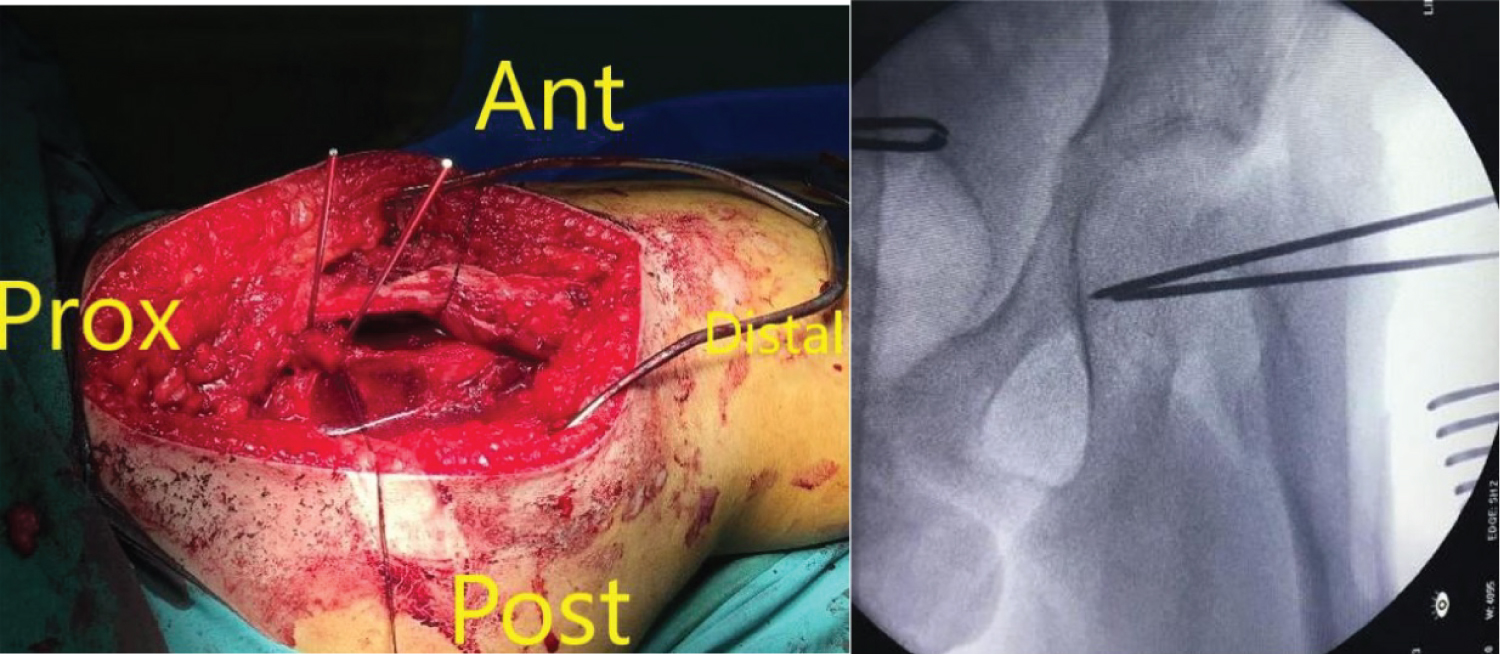
An eleven year old boy with high BMI for age presented to the Emergency Department with R Thigh pain with limping. He had pain for 2 months but the pain got suddenly worse over the previous 24 hours. He was unable to bear weight on the affected side. Clinical examination revealed an externally rotated posture of the Right lower limb with severe pain on any attempted movement of the hip. Initial xray was taken and was thought to be normal although it was suboptimal and as a result the patient was sent home. The following day the patient returned to the hospital with similar complains and repeat x-rays were taken showing a severe slip. He was admitted and placed on gentle traction (1 Kg). Perfusion MRI scan was requested and showed that perfusion of the femoral head is maintained. It also showed the severity of the slip and the difficulties of pinning the slip in situ. The MRI also showed that there an element of chronicity due to the presence of some callus around the posterior femoral neck. A diagnosis of severe acute on chronic slip was made (All images are in Figure 1). The patient was operated on day 10 after admission. We present below the surgical steps demonstrated by intra-operative photos (Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7, Figure 8, Figure 9 and Figure 10).
Conclusion
Surgical Hip dislocation popularized by the Bernese group is an effective approach to deal with intra-articular hip pathology in all age groups. It is, however, a very technical approach and attention to detail is of paramount importance to avoid complications. Using this technique in treating slipped upper femoral epiphysis is even more challenging due to the nature of the disease and the already compromised femoral head blood supply. In this paper we demonstrated this technique with detailed explanation of every step as well as intraoperative photos aiming to help paediatric and young adult hip surgeons understand each step of the approach. We hope this article will encourage surgeons to use this approach instead of in situ pinning for treating severe slipped upper femoral epiphysis patients.
Level of Evidence
V.
References
- Lehmann CL, Arons RR, Loder RT, et al. (2006) The epidemiology of slipped capital femoral epiphysis: An Update. J Paediatr Orthop 26: 286-290.
- Madan SS, Cooper AP, Davies AG, et al. (2013) The treatment of severe slipped capital femoral epiphysis via the Ganz surgical dislocation and anatomical reduction: A prospective study. The Bone & Joint Journal 95: 424-429.
- Mohammed Elmarghany, Tarek M Abd El Ghaffar, Mahmoud Seddik, et al. (2017) Surgical hip dislocation in treatment of slipped capital femoral epiphysis. Sicot J 3: 10.
- Kai Ziebarth, Christoph Zilkens, Samantha Spencer, et al. (2009) Capital realignment for moderate and severe SCFE using a modified dunn procedure. Clin Orthop Relat Res 467: 704-716.
- Nicola Ebert, Martin Rupprecht, Ralf Stuecker, et al. (2019) Outcome of the modified dunn procedure in severe chronic or acute on chronic slipped capital femoral epiphysis. Journal of Orthopaedic Surgery and Research 14: 349.
- R Ganz, TJ Gill, E Gautier, et al. (2001) Surgical dislocation of the adult hip. A technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br 83: 1119-1124.
- Alessandro Masse, Alessandro Aprato, Caterina Alluto, et al. (2015) Surgical hip dislocation is a reliable approach for treatment of femoral head fractures. Clin Orthop Relat Res 473: 3744-3751.
- M Leunig, HM Manner, L Turchetto, et al. (2017) Femoral and acetabular re-alignment in slipped capital femoral epiphysis. Journal of Children's Orthopaedics 11: 131-137.
Corresponding Author
Saeed Al-Naser, MD, Assistant Professor and Consultant Paediatric Orthopaedic Surgeon, Department of Trauma and Orthopaedics, Faculty of Medicine, The Hashemite University, Zarqa, Jordan, Tel: 00962791130920, Fax: 0096265682237.
Copyright
© 2020 Al-Naser S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.