Tibial Sesamoid Graft as a Treatment for Chronic Unstable Proximal Interphalangeal Joint Fracture Dislocation, a New Surgical Technique
Abstract
Purpose
This article reports a new surgical technique applied to treat a patient with chronic comminuted intra-articular volar middle phalanx base fracture of the 3rd finger. This technique uses the tibial sesamoid bone as an osteochondral graft and is characterized bya long-term follow-up.
Methods
The outcomes of the procedure applied on one patient before 10 years were evaluated clinically and radiographically. Besides that, the disabilities of the arm, shoulder and hand (DASH) scoreand the foot function index (FFI) score were used to grade respectively both his hand and foot.
Results
The patient had a full range of motion (ROM) 10 years after the surgery. DASH score was 0/100 while FFI was 0/170.
Conclusion
This technique was easy and cheap. It resulted in good clinical and functional outcomes with no complications 10 years post-operation.
Level of Evidence
Level IV
Keywords
Tibial sesamoid bone, PIP joint fracture, Volar base of middle phalanx, Hemi hamate arthroplasty
Introduction
Phalangeal fractures constitute 59% of all hand fractures. Amongst which, the middle phalanx represents 14% of fractures and the middle finger is involved in 17% of cases [1]. Thus, proximal interphalangeal joint (PIPJ) fracture dislocation is not an uncommon injury in hand traumatology. These involve 3 basic patterns including dorsal dislocation with volar lip fragment, volar dislocation with dorsal lip fragment and pilon fracture. Amongst these, volar base fracture with dorsal subluxation of the middle phalanx is the most common type [2].
As a matter of fact, the fracture recently mentioned above is usually caused by longitudinal compression force with the PIPJ in flexion impacting the volar articular surface of middle phalange against dorsal condyle of proximal phalange [2]. The restoration of the articular surface, stable reduction and safe early mobilization are the main goals of any treatment used. Stable injuries could be successfully treated conservatively [3] whereas, in unstable injuries, the treatment is usually surgical [2].
Acute unstable fractures can be treated by several ways depending on the percentage of volar lip, the degree of instability and the reducibility [2]. In fact, when the fracture is unstable due to large volar lip and can be reduced to a stable position with less than 30 degree of interphalangeal joint flexion, conservative treatment is recommended. These fractures are treated by extension bloc [2,4]. Despite that, all acute unstable fracture should be treated surgically. If the instability originates from one large volar fragment (> 50%), patients can be treated with closed reduction percutaneous pinning or by open reduction internal fixation [2,5]. Whereas, if the instability originates from multiple articular fragments or pilon fractures, it can be treated with dynamic external fixation where fractures are sufficiently reduced by traction [2,6-10]. When traction-based-reduction is impossible, fractures can be treated with interfragmentary screws or plate and screws if the joint is reconstructible [2,11-13]. If not, the last treatment options are volar plate reconstruction and hemihamate arthroplasty (HHA) [2,14-17].
On the other hand, chronic unstable injuries (> 6 weeks) are more difficult to treat and their treatment outcomes are worse than that of comparable injuries treated in due course. In fact, PIPJ fracture has a tendency to subluxate/dislocate more with time increasing the incidence of stiffness and decreasing the chance of achieving full ROM and normal function of the hand [2,18]. These fractures can be treated with open reconstruction of the articular surface with/without osteotomy and bone grafting followed by stabilization by K wires [18]. If the fracture cannot be reduced, volar plate arthroplasty was initially the treatment of choice before the emergence of HHA and prosthetic arthroplasty [16-18]. A recently published technique (2020) has involved the usage of costal osteochondral graft with a pins and rubbers traction system for the reconstruction of complex articular fracture. Their study had a 12-months follow-up period [19] only.
In this article, we describe a new surgical technique for the treatment of chronic unstable volar base fracture of the middle phalanx using the tibial sesamoid as an osteochondral graft to reconstruct the impacted volar articular surface of the middle phalangeal base. The aim of our study is to describe this new surgical technique and evaluate the radiological and clinical results after a long follow up. Our hypothesis was that the shape of tibial sesamoid bone can result in a more anatomical reconstruction of the cup-shaped articular surface of the middle phalangeal base and, thus, allows for a more congruency and stability of the PIPJ noting that its harvesting is simple and has less complication rates than other donor sites described in the literature.
Material and Method
We have recollected the long-term follow-up results of tibial sesamoid graft as a treatment for chronic severe dorsal fracture/dislocation of the PIPJ. This was the case of a 21-years-old right-handed man who had already passed through 3 months of failed conservative treatment of PIPJ fracture dislocation of his right third finger. He had a painful, deformed and limited ROM of the right third finger. Radiographs (Figure 1) showed a comminuted fracture of more than 50% of volar base middle phalanx with dorsal subluxation of PIPJ. The fracture was classified as chronic and unstable according to the Hasting classification [2].
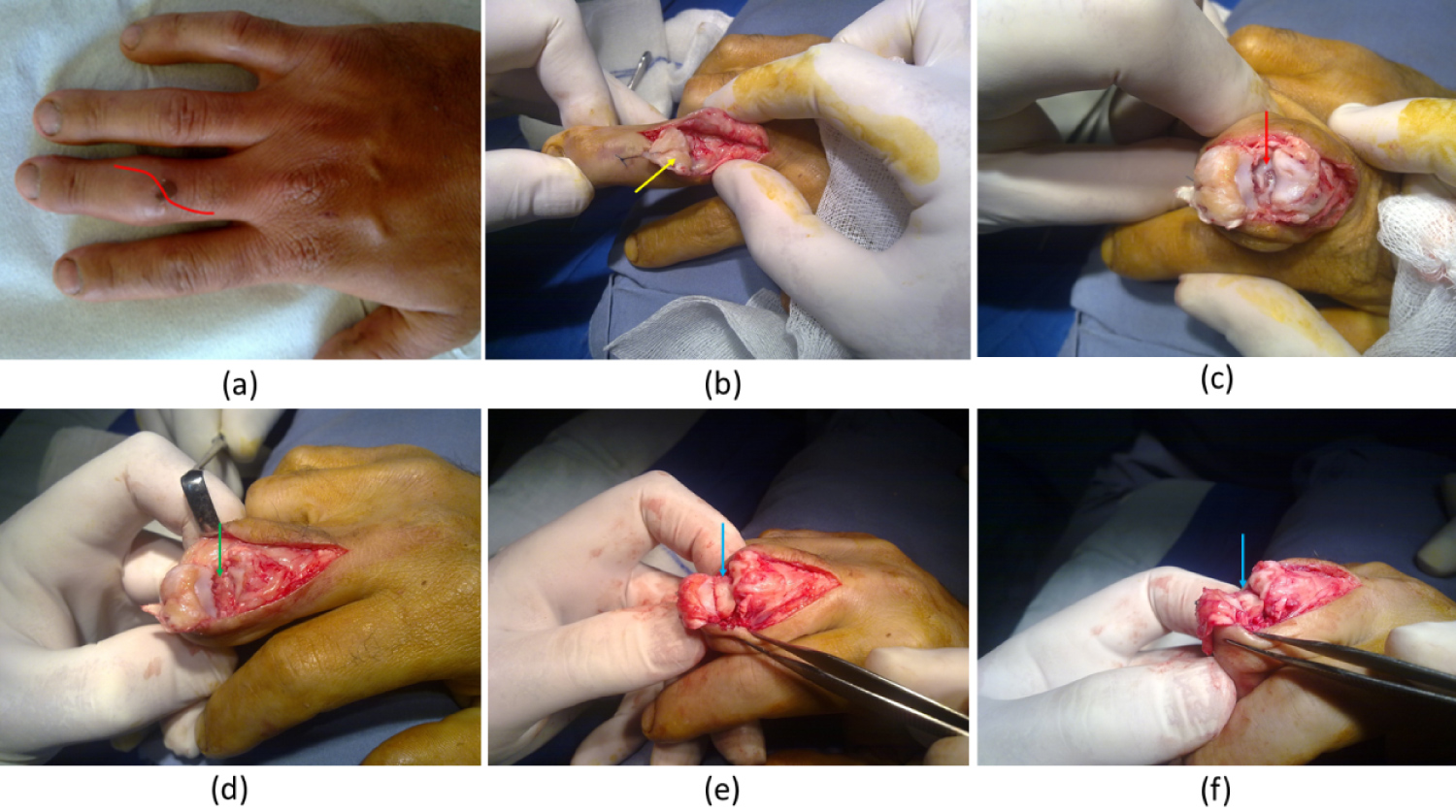
Surgical technique (Figure 2)
Tibial sesamoid harvesting: Through a longitudinal medial incision on the plantar side of the right big toe at the level of metatarsophalangeal joint and after protecting the plantar cutaneous nerve, the tibial sesamoid was identified and harvested. A careful capsulorrhaphy was performed.
Exposure and preparation of the fracture site: We made a 6 cm dorsal S-shaped incision over the PIPJ of the 3rd finger. At this level, a V-Shaped tenotomy along with the retraction of the extensor tendon was done. An arthrolysis of the PIPJ was done by releasing the collateral ligament with careful attention to avoid injuring the adjacent neurovascular bundles. Due to the retraction of the extensor tendons along with the hyperflexion of the PIPJ, the fracture was well exposed. Tiny bone fragments were excised then decortication of the middle phalanx base was done in order to create a smooth surface. Special caution was taken to prevent excessive removal of bone that could lead to fracture of the intact dorsal cortex.
Application of the sesamoid bone graft: After measuring the dimensions of bony defect, the harvested sesamoid bone was cut, trimmed and prepared accordingly in order to be congruent and adaptive. The prepared sesamoid bone graft was applied to the bony defect and the joint congruency was demonstrated by direct visualization of the articular surfaces to confirm that no step-off was present. Thus, the sesamoid graft was fixed to the dorsal base using a 1.5 mm diameter K wire. The joint was relocated, extensor tendon was repaired whereas the collateral ligaments were leaved without repair. The stability and ROM of the PIPJ were assessed clinically then skin was closed. Volar splint was applied and syndactyly of the 3rd & 4th finger was done for 1 week.
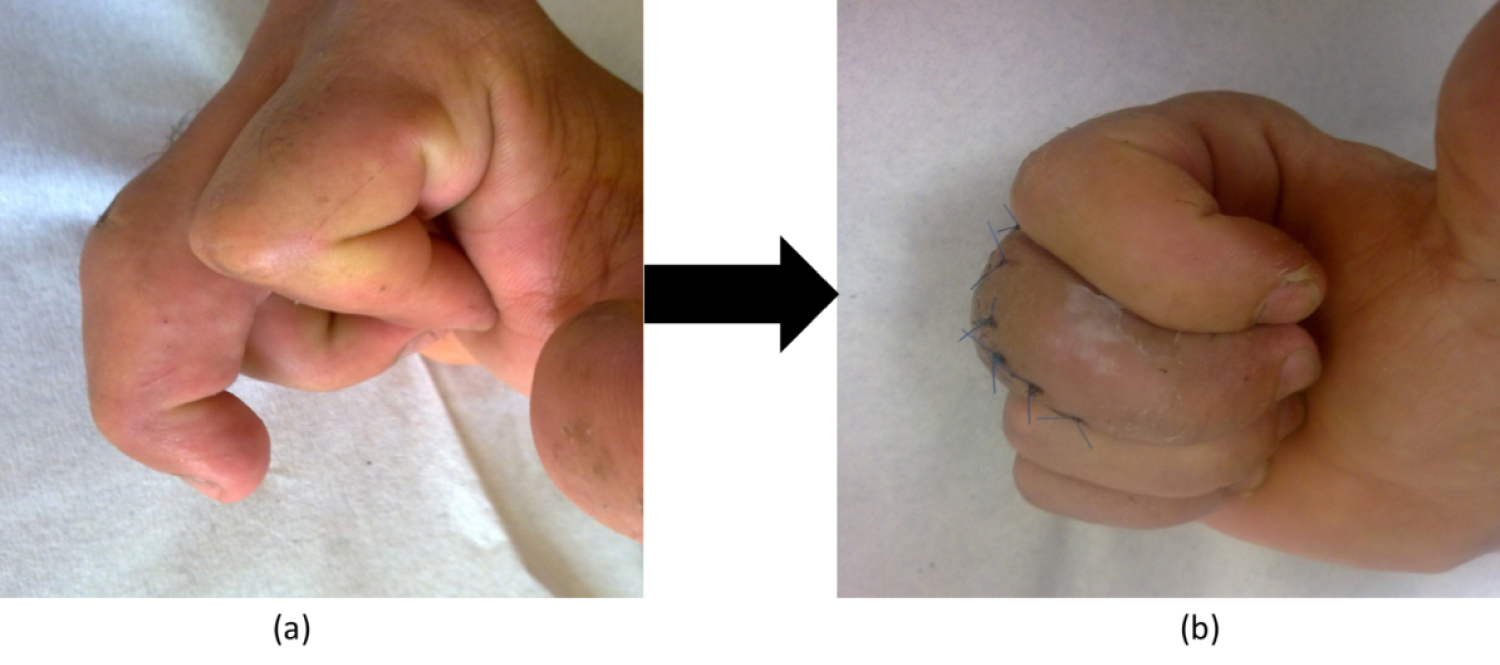
The patient started active ROM exercises for his finger approximately 1 week post-operatively (Figure 3) and was allowed a full weight bearing as tolerated. He returned to his work at week 2 postoperatively. Radiographic evaluation of anteroposterior and lateral radiographs was done pre- and postoperatively at day 1, week 8 and at the end of the follow up. In addition to that, clinical examinations were performed pre- and postoperatively at week 2, week 8 and at the end of follow up. Patient was evaluated for 1) ROM at the metacarpophalangeal joint (MCPJ), PIPJ and distal interphalangeal joint (DIPJ) and 2) Grip strength for the injured and non-injured hand. The involved finger was assessed for stability in both the sagittal and coronal planes. The donor site was evaluated clinically and radiographically post-operation and at the last check-up. The DASH scoring system for the upper limb and the FFI disability scale for the lower limb were used to assess the clinical outcomes.
Results
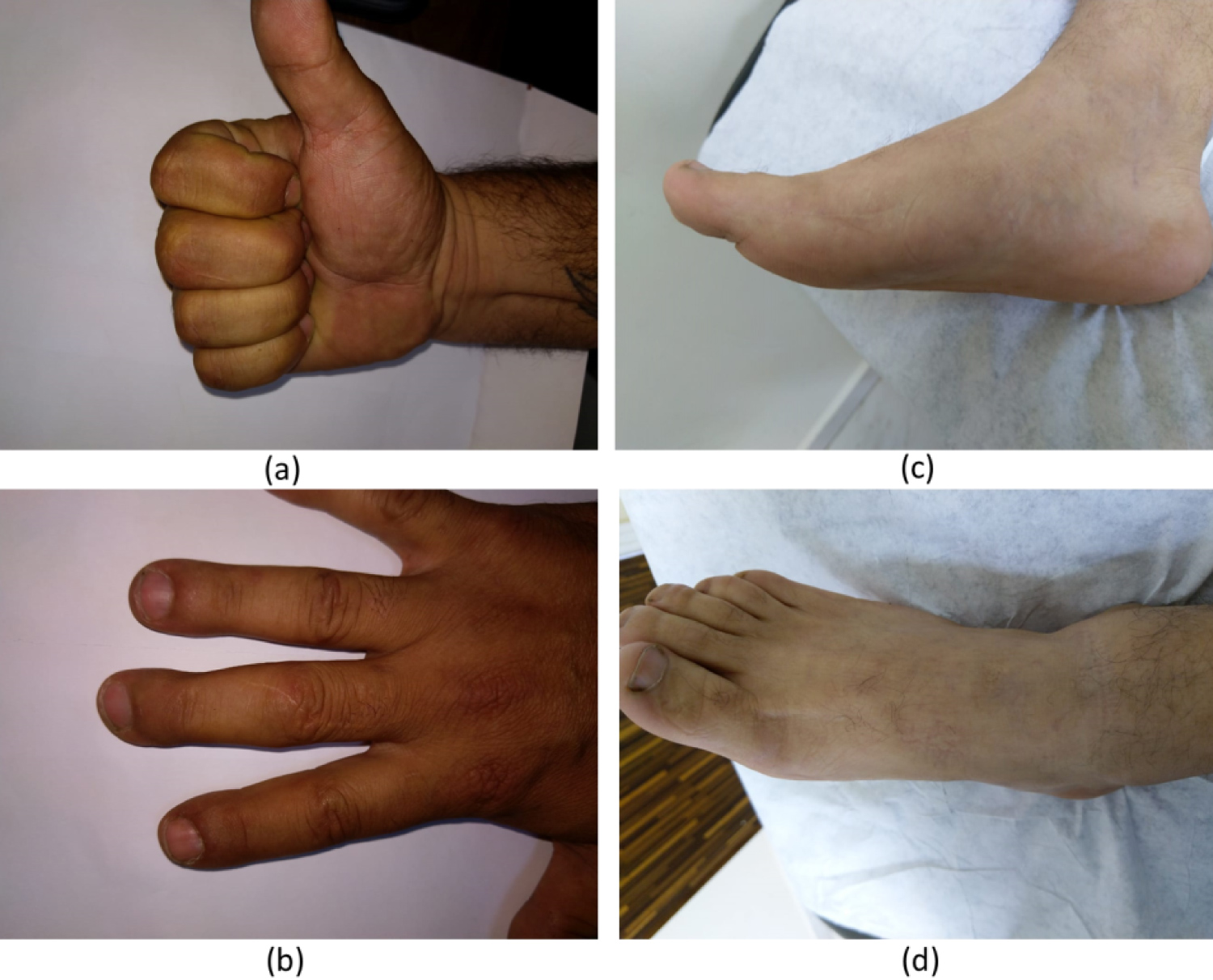
The patient was examined by the operating surgeon. Joint ROM was measured using a goniometer. At week 2, the patient had a ROM of MCPJ of (0°/100°) compared to (0°/100°) preoperatively, aROM of PIPJ of (0°/100°) compared to (5°/45°) preoperatively, and a ROM of DIPJ of (10°/70°) compared to (0°/70°) preoperatively (Table 1). He had no malrotation or angulation and the grip strength was near normal (98%) compared to the uninjured side. The patient was advised to continue active ROM. Concerning the donor site, physical examination revealed full function of the operated big toe with no stiffness and the patient could do the single toe raise test normally. At week 8 postoperatively, the radiographic examination showed good integration of the osteochondral graft along with good congruity. An apparent step-off at the articular surface was noted due to the difference in the articular thickness between the tibial sesamoid and the phalanx (Figure 4). On the other side, clinical examination showed no change. At the last checkup 10 years postoperatively, the patient had no complain of any pain on radial or ulnar stress of the PIPJ. There was no change in the ROM of the MCPJ (0°/100°), PIPJ (0°/100°) and DIPJ (10°/70°). The grip strength was normal (100%) compared to the uninjured side. No rotational or angular deformity was noted (Figure 5). X-rays showed good integration of the graft with no signs of osteoarthritis (Figure 6). The DASH score was 0/100. Concerning the donor site, there was no foot pain, stiffness, functional loss, cock-up deformity, claw toe deformity, hallux valgus deformity or any other complications. Hallux valgus angle (HVA), intermetatarsal angle (IMA) and distal metatarsal articular angle (DMMA) were within the normal ranges (Figure 7). FFI disability scale was 0/170.
Concerning the internal fixation material, it had not cause any clinical or functional derangement for the patient and, accordingly, it was not removed.
Discussion
Our study revealed that this new technique using the tibial sesamoid can restore the anatomy of the donor site morbidity and the complications.
In our technique, the tibial sesamoid, after being trimmed and fixed in the PIPJ, fit very well in the bony defect, gave good stability and was easy to apply. X-rays demonstrated good restoration of the anatomy of the PIPJ with good joint line and no osteoarthritis 10 years after surgery. While in other surgical options, the anatomy couldn't be restored perfectly as in our case. In HHA introduced by Hasting on 1999 [20], the radius of curvature of the distal articular surface of the hamate was greater than that of the base of middle phalange. A previous cadaveric study showed that the contour of the distal articular surface of the hamate is shallower than that of the middle phalangeal base, with the phalangeal radius of curvature ranging from 45% to 61% of the hamate [20]. This difference was the main cause of subsequent subluxation observed in HHA [21]. Furthermore, although slight tilting when harvesting the hamate graft gave better results, this step is still considered technically demanding and requires special surgical equipment and instruments.
The patient returned to his work with full ROM of the PIPJ and normal grip strength 2 weeks after surgery compared to an average delay of 29 days following HHA (Williams, et al. 2003) and 78 days (Lindenblatt, et al. 2013) respectively. Also, this took much longer in manual workers, with means of 53 and 124 days respectively [16,21,22]. Moreover, at the last checkup, the patient had no pain, no signs of osteoarthritis and no major complication while there was few data in literature about long term complications especially osteoarthritis which has been proven to exist in up to 50% of cases [16,21]. The complication rate of HHA was 35% including ulnar collapse, subluxation, failure, proximal interphalangeal contracture, fractured dorsal cortex, pulley insufficiency, graft loss, nonunion and tenderness [21].
However, the patient lost 10 degrees of terminal extension of the DIPJ attributed to the extensor tenotomy. Whereas, in the systematic review of several reports concerning HHA done by Frueh, et al. on 2014 including 71 patients, the mean PIPJ ROM was 77° in 71 patients at an average 36-months follow-up and the mean ROM of the DIPJ was 59° in 64 patients [21].
The dorsal approach used in our technique avoided the flexor pulley system of the finger, whereas HHA described by several authors used the volar approach to reconstruct the PIPJ. And, as a matter of fact, this volar approach may end up by unrepairable flexor sheath, pulley insufficiency and flexor tendon bowstringing [23,24].
In the first metatarsal head, the medial sesamoid is larger and elongated with an average 9 mm diameter [25,26]. As far as we know, sesamoidectomy has never been used as an osteochondral graft, but many authors described sesamoidectomy as a treatment of choice to treat sesamoid disorders such as fracture or sesamoiditis [27-32]. Several studies showed that isolated tibial sesamoidectomy with soft tissue repair is efficacious and safe even for the patient populations with the highest physical demands [82,33-41]. The donor site was easy to access in our technique and graft harvesting was simple in contrast to the osteochondral graft in HHA which, as mentioned above, is complex, difficult and technically challenging with steep learning curve [20]. Our patient didn't complain of any donor site morbidity. He had no foot or toe pain and maintained full ROM of the big toe with normal motor power. The FFI disability scale was 0. X-rays demonstrated normal HVA, IMA and DMAA. There was no claw toe or cock up deformities. While in HHA, donor site complications may include pain, a decreasing ROM of wrist and fingers, scar, osteoarthritis, hamate fracture, radioulnar instability, edema and thermal bone necrosis during graft harvesting and angulation [17,21,42].
HHA is contraindicated in patients with severe soft tissue damage, preinjury arthritis and other carpal problems [17]. In addition, this type of injury is more frequent in athletes and handworkers and they may not tolerate a second type of surgical trauma to the hand in order to treat the original one delaying their return to their basal activity. On the contrary, our technique can be safely performed on those patients since the donor site is far from the hand.
Several options other than HHA were described to treat chronic unstable volar base fracture of middle phalange. The microsurgical hemi-hamate free flap is a new option which might reduce the risk of long-term osteoarthritis but the procedure is more technically challenging and requires microsurgical skills and equipement [22,43,44]. Prosthetic arthroplasty is another option but high rates of complications and failure [45-50] were reported. Failure and severe complications were also observed in allogenic osteochondral graft which requires adequate lifelong immunosuppressive therapy [51].
Since the PIPJ is not a weight bearing joint, anatomical reduction is not necessary in a reduced, well aligned joint that has acceptable, safe and painless ROM [52-54]. Studies showed that the quality of reduction is not correlated with clinically relevant posttraumatic arthrosis in the PIPJ. The problem in the PIPJ is the stiffness. Thus, early mobilization is the most important factor to achieve the best clinical outcomes [55].
Our study is not without limitations. Since this type of injury is most often treated acutely, the chronic cases are limited and not seen in our daily practice, so we need more cases to evaluate the clinical and radiographic outcomes of the procedure. Moreover, patients with preoperative high HVA are at high risk to develop hallux valgus after medial sesamoid excision. In addition, we don't have a cadaveric study to assess the exact shape and radius of curvature of the sesamoid bone and the base of the phalanx in order to compare and try to match the articular surfaces together.
Conclusion
The treatment of chronic unstable fracture dislocation of the PIPJ requires an osteochondral graft that can restore the anatomy and maintain the stability of the joint with less complication rates and donor site morbidity. All these goals could be achieved by tibial sesamoid osteochondral graft followed by capsulorrhaphy and early mobilization.
Conflicts of Interest and Source of Funding
All authors have no conflict of interest and have not received any funding for this work from any of the following organizations: National Institutes of Health (NIH), Wellcome Trust, Howard Hughes Medical Institute (HHMI) and other(s).
References
- Van Onselen EB, Karim RB, Hage JJ, et al. (2003) Prevalence and distribution of hand fractures. J Hand Surg Br 28: 491-495.
- Caggiano NM, Harper CM, Rozental TD (2018) Management of proximal interphalangeal joint fracture dislocations. Hand Clin 34: 149-165.
- Phair IC, Quinton DN, Allen MJ (1989) The conservative management of volar avulsion fractures of the P.I.P. joint. J Hand Surg 14: 168-170.
- Hamer DW, Quinton DN (1992) Dorsal fracture subluxation of the proximal interphalangeal joints treated by extension block splintage. J Hand Surg Br 17: 586-590.
- Aladin A, Davis TR (2005) Dorsal fracture-dislocation of the proximal interphalangeal joint: A comparative study of percutaneous Kirschner wire fixation versus open reduction and internal fixation. J Hand Surg Br 30: 120-128.
- Krakauer JD, Stern PJ (1996) Hinged device for fractures involving the proximal interphalangeal joint. ClinOrthopRelat Res 327: 29-37.
- Morgan JP, Gordon DA, Klug MS (1995) Dynamic digital traction for unstable comminuted intra-articular fracture-dislocations of the proximal interphalangeal joint. J Hand Surg Am 20: 565-573.
- Schenck RR (1986) Dynamic traction and early passive movement for fractures of the proximal interphalangeal joint. J Hand Surg 11: 850-858.
- Stark RH (1993) Treatment of difficult PIP joint fractures with a mini-external fixation device. Orthop Rev 22: 609-615.
- Bain GI, Mehta JA, Heptinstall RJ, et al. (1998) Dynamic external fixation for injuries of the proximal interphalangeal joint. J Bone Joint Surg Br 80: 1014-1019.
- Lee JY, Teoh LC (2006) Dorsal fracture dislocations of the proximal interphalangeal joint treated by open reduction and interfragmentary screw fixation: Indications, approaches and results. J Hand Surg Br 31: 138-146.
- Tekkis PP, Kessaris N, Gavalas M, et al. (2001) The role of mini-fragment screw fixation in volar dislocations of the proximal interphalangeal joint. Arch Orthop Trauma Surg 121: 121-122.
- Grant I, Berger AC, Tham SK (2005) Internal fixation of unstable fracture dislocations of the proximal interphalangeal joint. J Hand Surg Br 30: 492-498.
- Dionysian E, Eaton RG (2000) The long-term outcome of volar plate arthroplasty of the proximal interphalangeal joint. J Hand Surg Am 25: 429-437.
- Eaton RG, Malerich MM (1980) Volar plate arthroplasty of the proximal interphalangeal joint: A review of ten years experience. J Hand Surg Am 5: 260-268.
- Williams RM, Kiefhaber TR, Sommerkamp TG, et al. (2003) Treatment of unstable dorsal proximal interphalangeal fracture/dislocations using a hemi-hamate autograft. J Hand Surg Am 28: 856-865.
- Williams RM, Hastings H 2nd, Kiefhaber TR (2002) PIP fracture/dislocation treatment technique: Use of a hemi-hamate resurfacing arthroplasty. Tech Hand Up Extrem Surg 6: 185-192.
- Ishida O, Ikuta Y (1998) Results of treatment of chronic dorsal fracture dislocations of the proximal interphalangeal joints of the fingers. J Hand Surg 23: 798-801.
- Satake Y, Nanno M, Kodera N, et al. (2020) Use of a costal osteochondral graft for reconstruction of a proximal phalanx head with a comminuted fracture of the proximal interphalangeal joint. J Nippon Med Sch 87: 37-42.
- Capo JT, Hastings H 2nd, Choung E, et al. (2008) Hemicondylar hamate replacement arthroplasty for proximal interphalangeal joint fracture dislocations: An assessment of graft suitability. J Hand Surg Am 33: 733-739.
- Frueh FS, Calcagni M, Lindenblatt N (2015) The hemi-hamate autograft arthroplasty in proximal interphalangeal joint reconstruction: A systematic review. The Journal of Hand Surgery European 40: 24-32.
- Lindenblatt N, Biraima A, Tami I, et al. (2013) Hemi-hamate autograft arthroplasty for acute and chronic PIP joint fracture dislocations. Handchir Mikrochir Plast Chir 45: 13-19.
- Calfee RP, Kiefhaber TR, Sommerkamp TG, et al. (2009) Hemi-hamate arthroplasty provides functional reconstruction of acute and chronic proximal interphalangeal fracture-dislocations. J Hand Surg Am 34: 1232-1241.
- Tang JB, Xie RG (2001) Effect of A3 pulley and adjacent sheath integrity on tendon excursion and bowstringing. J Hand Surg Am 26: 855-861.
- Bizarro AH (1921) On the traumatology of the sesamoid structures. Ann Surg 74: 783-791.
- Vijaianand M, Ravichandran Doraiswamy (2016) Sesamoids of the feet: Cadaveric study on the incidence and morphology in south Indian population. Int J Anat Res 4: 3092-3096.
- Dedmond BT, Cory JW, McBryde A Jr (2006) The hallucal sesamoid complex. J Am Acad Orthop Surg 14: 745-753.
- Bichara DA, Henn RF 3rd, Theodore GH (2012) Sesamoidectomy for hallux sesamoid fractures. Foot Ankle Int 33: 704-706.
- Kane JM, Brodsky JW, Daoud Y (2017) Radiographic results and return to activity after sesamoidectomy for fracture. Foot Ankle Int 38: 1100-1106.
- Tagoe M, Brown HA, Rees SM (2009) Total sesamoidectomy for painful hallux rigidus: A medium-term outcome study. Foot Ankle Int 30: 640-646.
- Inge GAL, Ferguson AB (1933) Surgery of the sesamoid bones of the great toe: An anatomic and clinical study, with a report of forty-one cases. Arch Surg 27: 466-489.
- Mann RA, Coughlin MJ, Baxter D, et al. (1985) Sesamoidectomy of the great toe. Presented at: 15th Annual Meeting of the American Orthopaedic Foot & Ankle Society, Las Vegas, NV.
- Lee S, James WC, Cohen BE, et al. (2005) Evaluation of hallux alignment and functional outcome after isolated tibial sesamoidectomy. Foot Ankle Int 26: 803-809.
- Nayfa TM, Sorto LA (1982) The incidence of hallux abductus following medial sesamoidectomy. J Am Podiatr Assoc 72: 617-620.
- Inge GA (1936) Congenital absence of the medial sesamoid bone of the great toe. J Bone Joint Surg (Am) 18: 188-190.
- Aper RL, Saltzman CL, Brown TD (1994) The effect of hallux sesamoid resection on the effective moment of the flexor hallucis brevis. Foot Ankle Int 15: 462-470.
- Aper RL, Saltzman CL, Brown TD (1996) The effect of hallux sesamoid excision on the flexor hallucis longus moment arm. Clin Orthop Relat Res 325: 209-217.
- Saxena A, Krisdakumtorn T (2003) Return to activity after sesamoidectomy in athletically active individuals. Foot Ankle Int 24: 415-419.
- Canales MB, DeMore M 3rd, Bowen MF, et al. (2015) Fact or fiction? Iatrogenic hallux abducto valgus secondary to tibial sesamoidectomy. J Foot Ankle Surg 54: 82-88.
- Shimozono Y, Hurley ET, Brown AJ, et al. (2018) Sesamoidectomy for hallux sesamoid disorders: A systematic review. J Foot Ankle Surg 57: 1186-1190.
- Biedert R, Hintermann B (2003) Stress fractures of the medial great toe sesamoids in athletes. Foot Ankle Int 24: 137-141.
- Afendras G, Abramo A, Mrkonjic A, et al. (2010) Hemi-hamate osteochondral transplantation in proximal interphalangeal dorsal fracture dislocations: A minimum 4 year follow-up in eight patients. J Hand Surg Eur Vol. 35: 627-631.
- Rozen WM, Niumsawatt V, Ross R, et al. (2013) The vascular basis of the hemi-hamate osteochondral free flap. Part 1: Vascular anatomy and clinical correlation. Surg Radiol Anat 35: 585-594.
- Rozen WM, Niumsawatt V, Leong JC, et al. (2013) The vascular basis of the hemi-hamate osteochondral free flap. Part 2: Surgical anatomy and clinical application. Surg Radiol Anat 35: 595-608.
- Ashworth CR, Hansraj KK, Todd AO, et al. (1997) Swanson proximal interphalangeal joint arthroplasty in patients with rheumatoid arthritis. Clin Orthop Relat Res 342: 34-37.
- Branam BR, Tuttle HG, Stern PJ, et al. (2007) Resurfacing arthroplasty versus silicone arthroplasty for proximal interphalangeal joint osteoarthritis. J Hand Surg Am 32: 775-788.
- Linscheid RL (2000) Implant arthroplasty of the hand: Retrospective and prospective considerations. J Hand Surg Am 25: 796-816.
- Minamikawa Y, Imaeda T, Amadio PC, et al. (1994) Lateral stability of proximal interphalangeal joint replacement. J Hand Surg Am 19: 1050-1054.
- Tuttle HG, Stern PJ (2006) Pyrolytic carbon proximal interphalangeal joint resurfacing arthroplasty. J Hand Surg Am 31: 930-939.
- Sweets TM, Stern PJ (2010) Proximal interphalangeal joint prosthetic arthroplasty. J Hand Surg Am 35: 1190-1193.
- Revell CM, Athanasiou KA (2009) Success rates and immunologic responses of autogenic, allogenic, and xenogenic treatments to repair articular cartilage defects. Tissue Eng Part B Rev 15: 1-15.
- Kiefhaber TR, Stern PJ (1998) Fracture dislocations of the proximal interphalangeal joint. J Hand Surg Am 23: 368-380.
- Agee JM (1987) Unstable fracture dislocations of the proximal interphalangeal joint. Treatment with the force couple splint. Clin Orthop Relat Res 214: 101-112.
- Salter RB (1994) The physiologic basis of continuous passive motion for articular cartilage healing and regeneration. Hand Clin 10: 211-219.
- Strickland JW, Steichen JB (1982) Difficult problems in hand surgery. American society for surgery of the hand. St. Louis, Mosby, MO, 434.
Corresponding Author
Ali Hellani, Department of Orthopedic Surgery, Zahraa University Hospital, Beirut, Lebanon
Copyright
© 2020 Mansour O, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.