Management of Chondroblastoma of the Femoral Head by Controlled Hip Dislocation Technique and Use of Allograft: Case Report
Abstract
Epiphyseal Chondroblastoma (EC) is known to be a very rare tumor with highly aggressive local capacity despite its benign nature. We report a case of a female patient treated for long lasting right hip pain diagnosed with EC of the femoral head. The lesion was treated with complete local resection by means of controlled surgical hip dislocation, "trap door" technique and use of allograft. Functional results in the short run where adequate with no local recurrence and no metastatic lung lesions. Nonetheless, during follow up, Avascular Necrosis (AVN), posterior dislocation of the femoral head and coxa magna took place, requiring multiple re interventions that allowed adequate functionality after 1 year of the initial surgery.
Keywords
Epiphyseal chondroblastoma, Femoral head, Controlled hip dislocation, Trap door technique, Avascular necrosis
Introduction
EC is described as a benign infrequent tumor with local aggressive capacity [1-18], being the femoral head one of the most challenging locations for surgical management [2,10,11]. The clinical and radiological diagnosis reveals distinctive characteristics that allow the identification of the lesions and so its management [4,11,17]. Great controversy exists regarding the best surgical management since, although it has been established that complete lesion resection is a standard, the use of adjuvants and allografts has not been globally accepted [4,8,9,11,12]. Additionally, literature reports good prognosis in the long run with low possibility for malignant transformation and metastasis [1,10,14], however with the possibility of local recurrence, especially in locations that are difficult to access, like the femoral head [5,14]. This case reports an experience with surgical dislocation of the hip for complete lesion resection.
Case Presentation
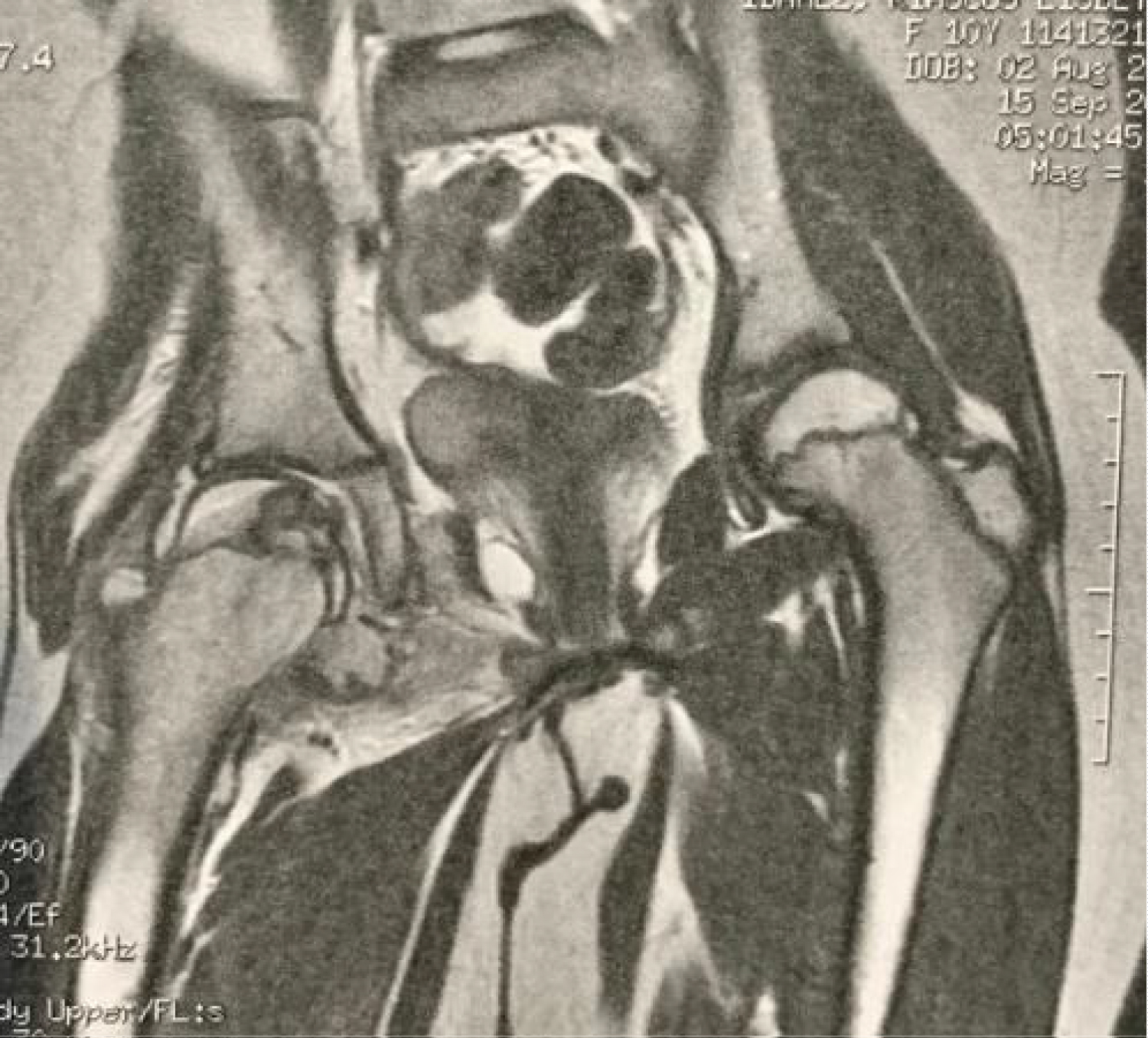
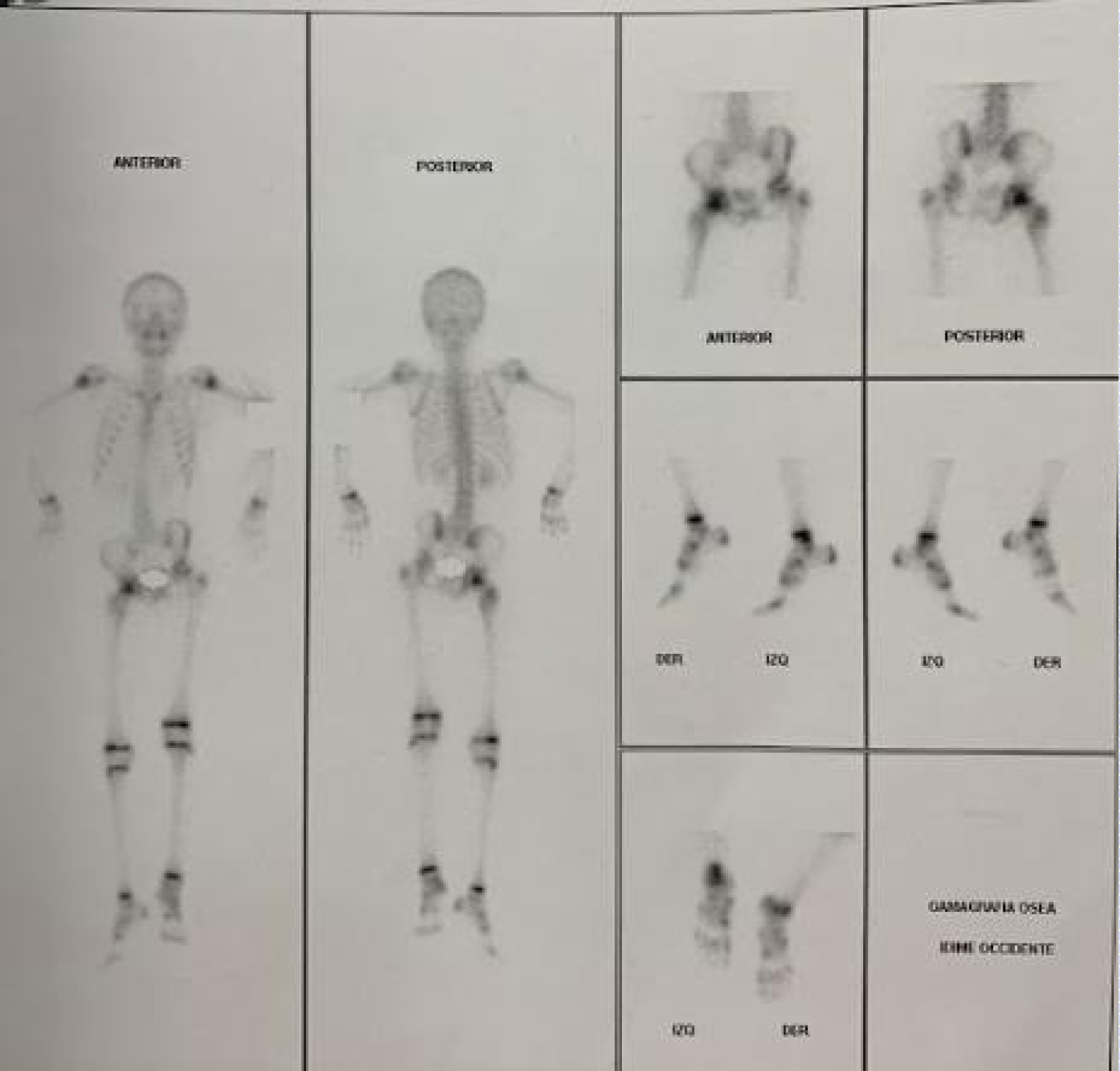
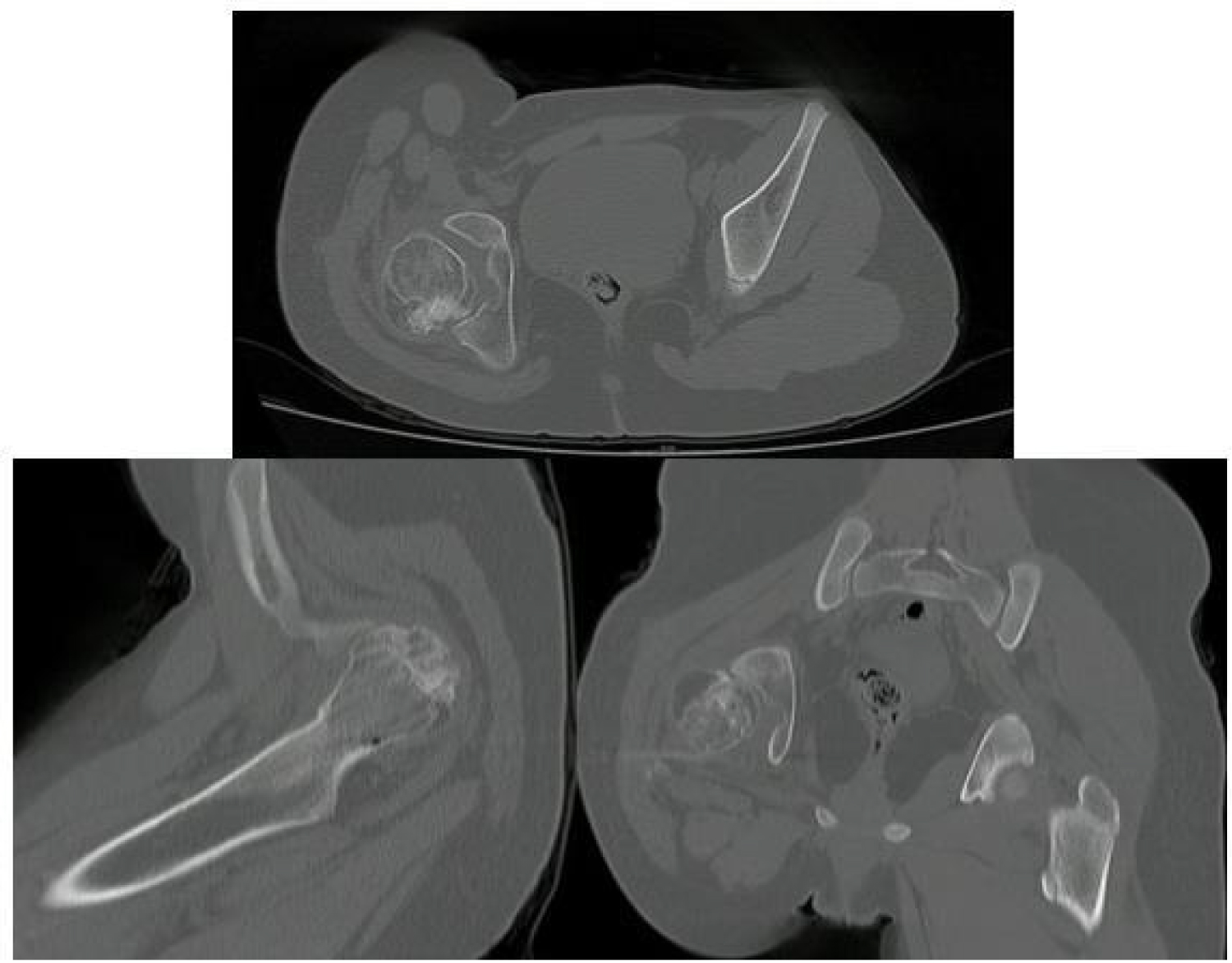
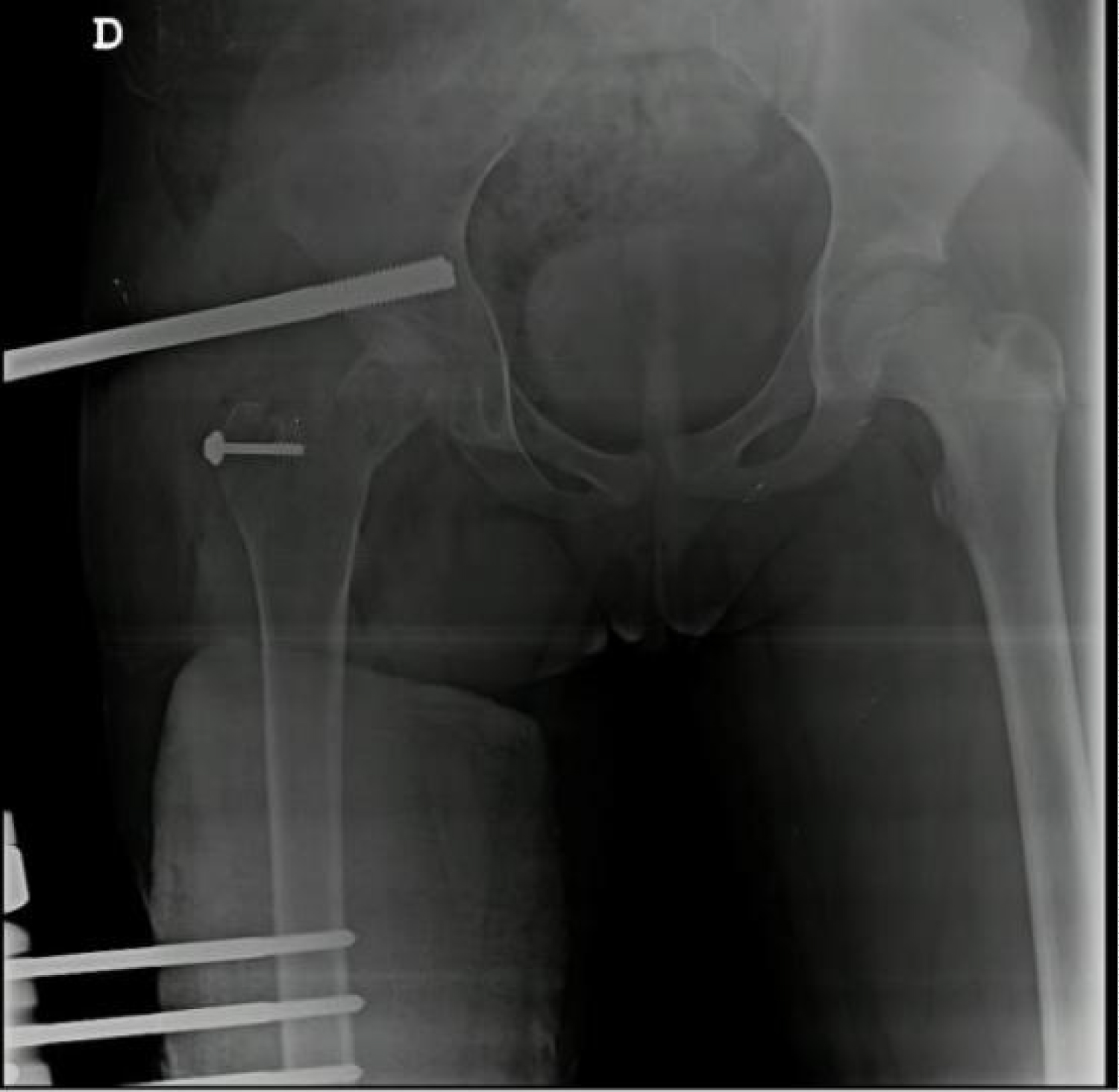
A 10-year-old girl presented to our institution after 2 years of right hip pain which limited deambulation and hip mobility. X-ray revealed a lytic lesion limited exclusively to the epiphysis of the femoral head, destroying it in the anterior and medial quadrants (Figure 1). Magnetic Resonance Imaging (MRI) showed that the lesion did not crossed the growth plate (Figures 2 and Figures 3) and the gamma graphy high lighted the right femoral head epiphys is (Figure 4), with no presence of lung lesions. Due to symptoms and imaging diagnostic for EC, the patient was considered for surgical resection with allograft reconstruction. During follow up, the patient refers great improvement of hip pain, mobility and performs walking with partial support using external aids after 2 months of the initial surgery. Nevertheless, after 6 months of follow up, the patient develops posterior hip dislocation, coxa magna and AVN of the femoral head (Figures 5 and Figures 6) requiring re-intervention for reduction and arthrodiastasis with an external fixation (Figure 7). Regrettably, after 1 month of the procedure, the external fixation fails (7 months after initial surgery), is retrieved and immobilization with abductor casts is held for 4 additional weeks. After 1 year of the initial surgery, despite sequels in radiologic imaging (Figure 8), the patient is able to accomplish acceptable hip movements with no pain and is able to walk using only one external aid.
Surgical technique for lesion resection
For the procedure, the patient was positioned in left lateral decubitus, covering the surgical site with sterile drapes and leaving the complete extremity available for manipulation during the surgery. The Anterior Superior Iliac Spine (ASIS) and the Femoral Greater Trochanter (FGT) were chosen as reference points. A longitudinal incision is done in a proximal to distal direction, beginning 20 cm posterior to the ASIS towards 2 cm above the FGT.
Subcutaneous tissue is then exposed revealing the fascia lata which is also incised longitudinally, both edges of the surgical area are retracted in order to expose the Vastus Lateralis (VL) and the FGT. We proceed to develop an incision following the anterior border of the VL proximally and parallel to the femoral axis, after this, the VL is carefully dissected under the periosteum. Then, using a bone saw, an osteotomy of the FGT is done following the technique for patelization (digastric osteotomy - gluteus medius proximally and VL distally) [19] (Figure 9).
The now mobile trochanter is retracted in an anterior and superior direction, exposing the articular cápsule. We carry out a "half moon" capsulotomy to avoid injuring the vascular pedicle. Once the femoral head and neck are exposed, a controlled hip dislocation is done by means of external rotation, adduction and flexion, being careful not to injure the labrum.
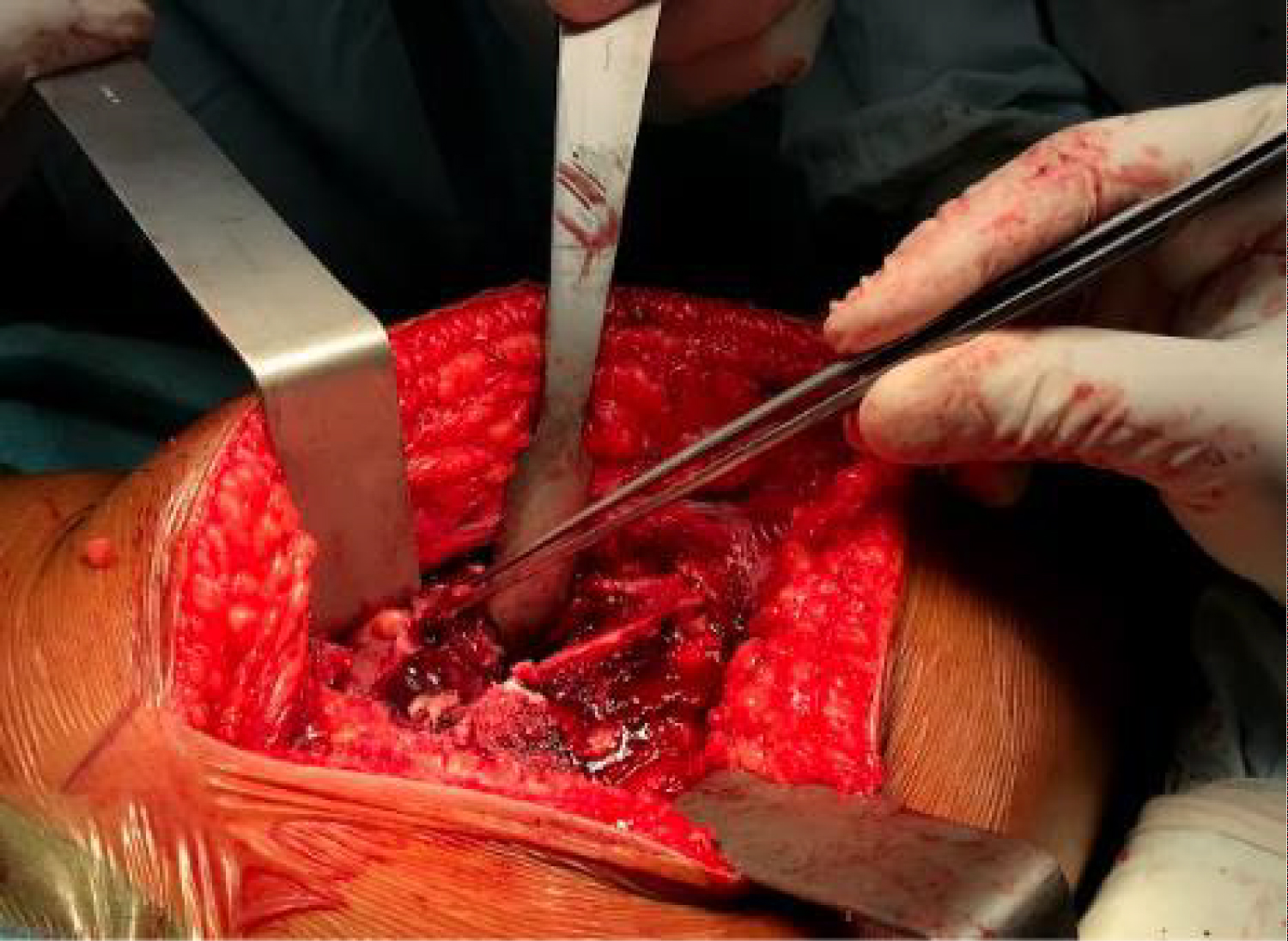
Once the femoral head has been exposed, the lesion is located in the anterior and medial quadrants. It exposes soft cartilage - like consistency while the surrounding articular cartilage is intact (Figure 10).
Curettage of the lesion is done, resecting completely the affected area with no injury to the growth plate. Additional use of a high speed burr (Midax - Rex) to debride the walls of the lesion allows for a more precise resection.
Then, precise measurements of the remaining defect in the femoral head allow the shaping of the humeral head allograft (Figure 11) which is then impacted inside the defect. Adequate covering of the defect is achieved with no instability of the allograft nor surface irregularities (Figure 12).
The hip is then reduced into the acetabulum, capsulorrhaphy and suture of the mobile fragment of the GFT is done with absorbable suture. A 4.5 mm cannulated screw with washer is used for maintaining the reduction of the GFT (Figure 13).
Finally, the surgical site is closed by planes and the pathology of the tumor, capsule and hypertrophic synovial tissue is sent for further examination. Post-surgical X-rays reveal a congruent articulation (Figure 14).
Pathology
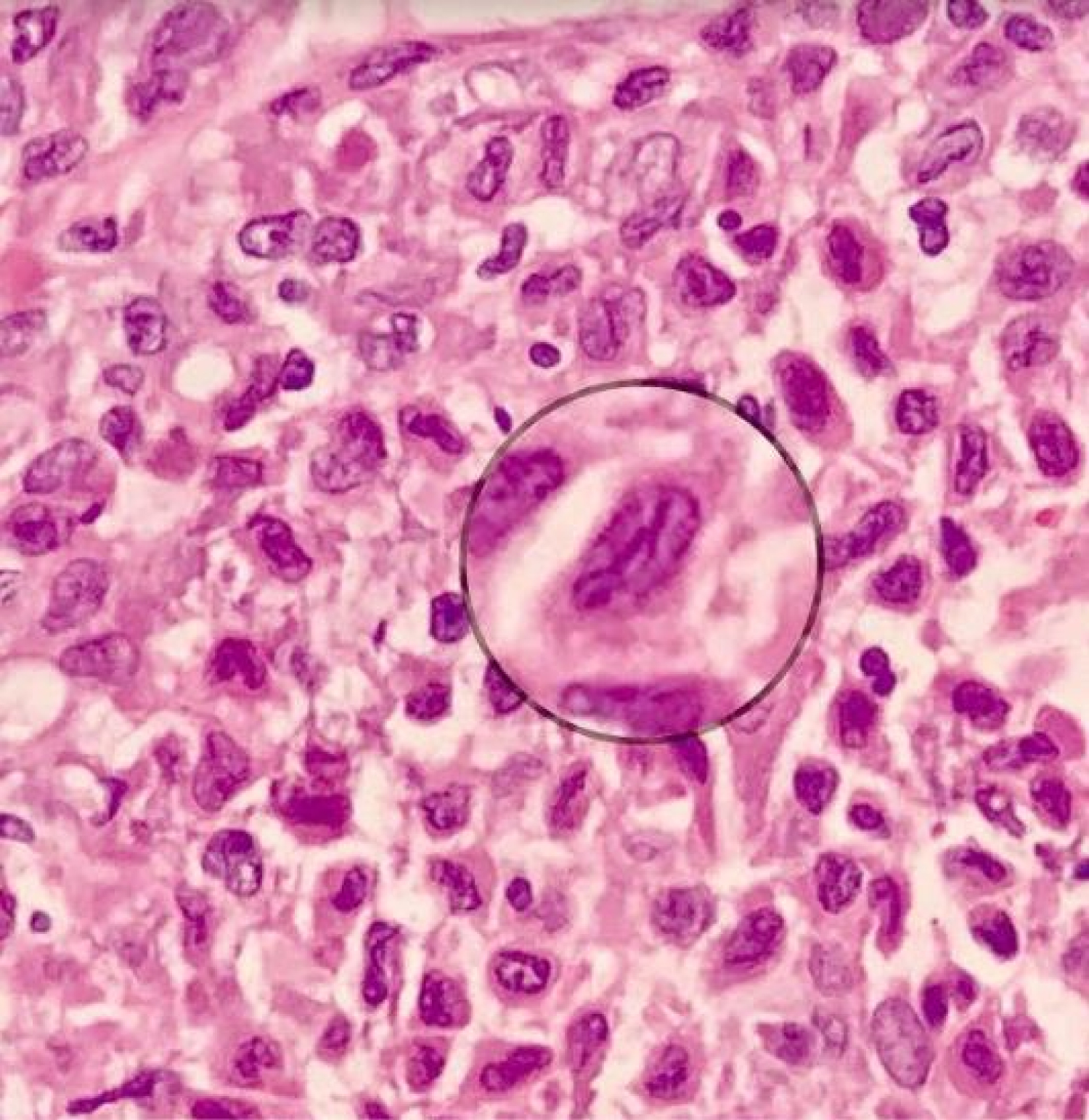
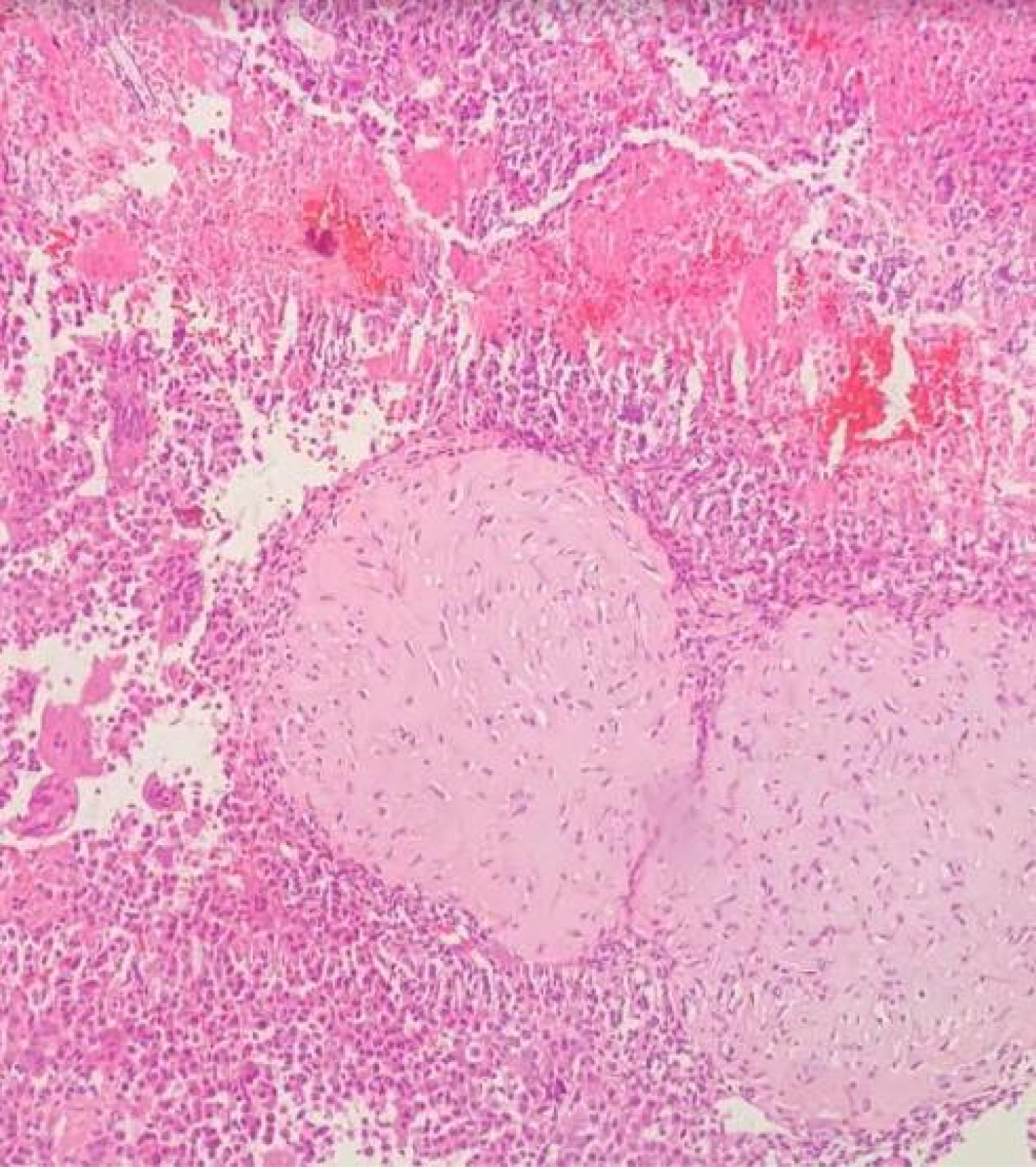
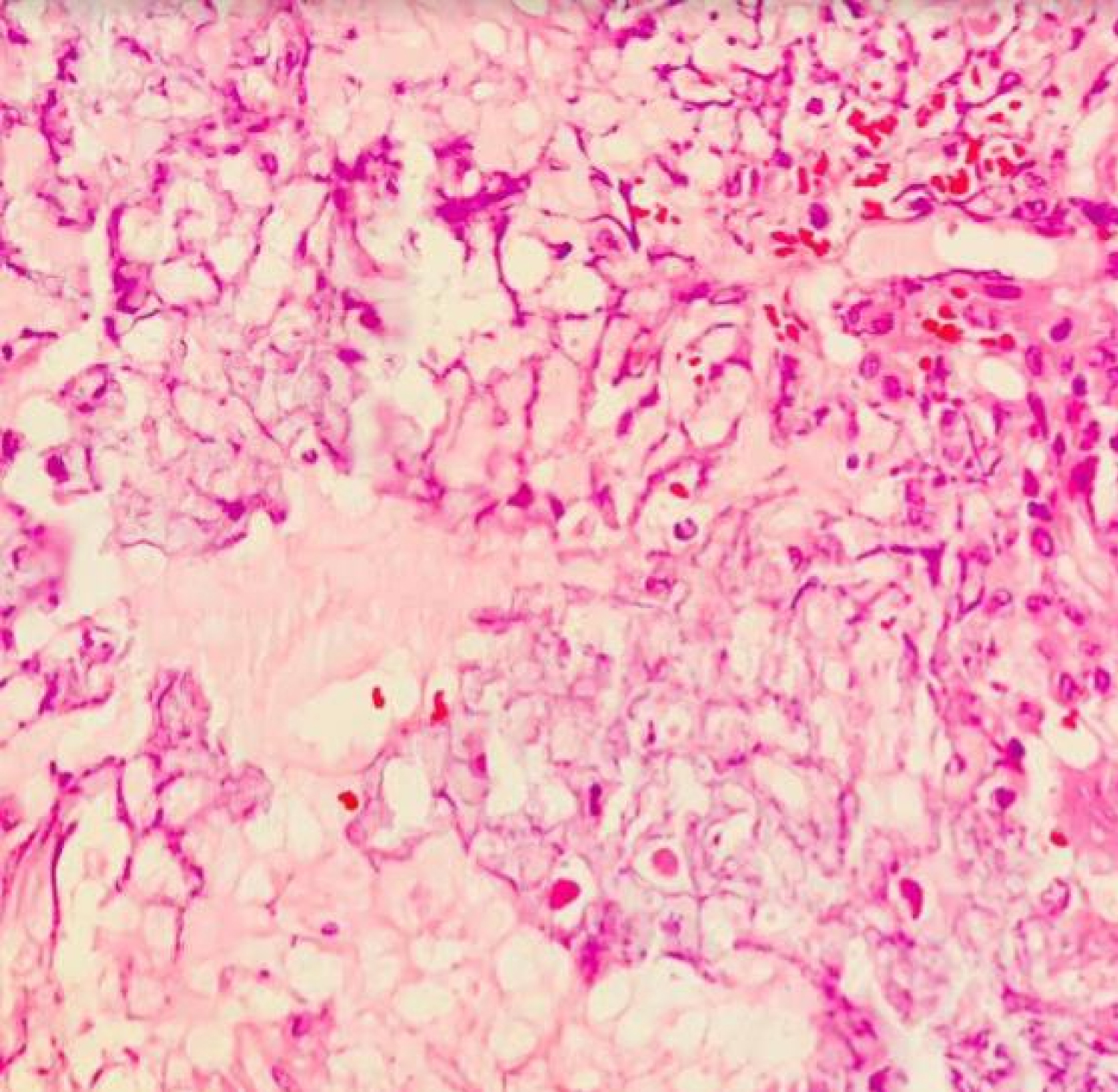
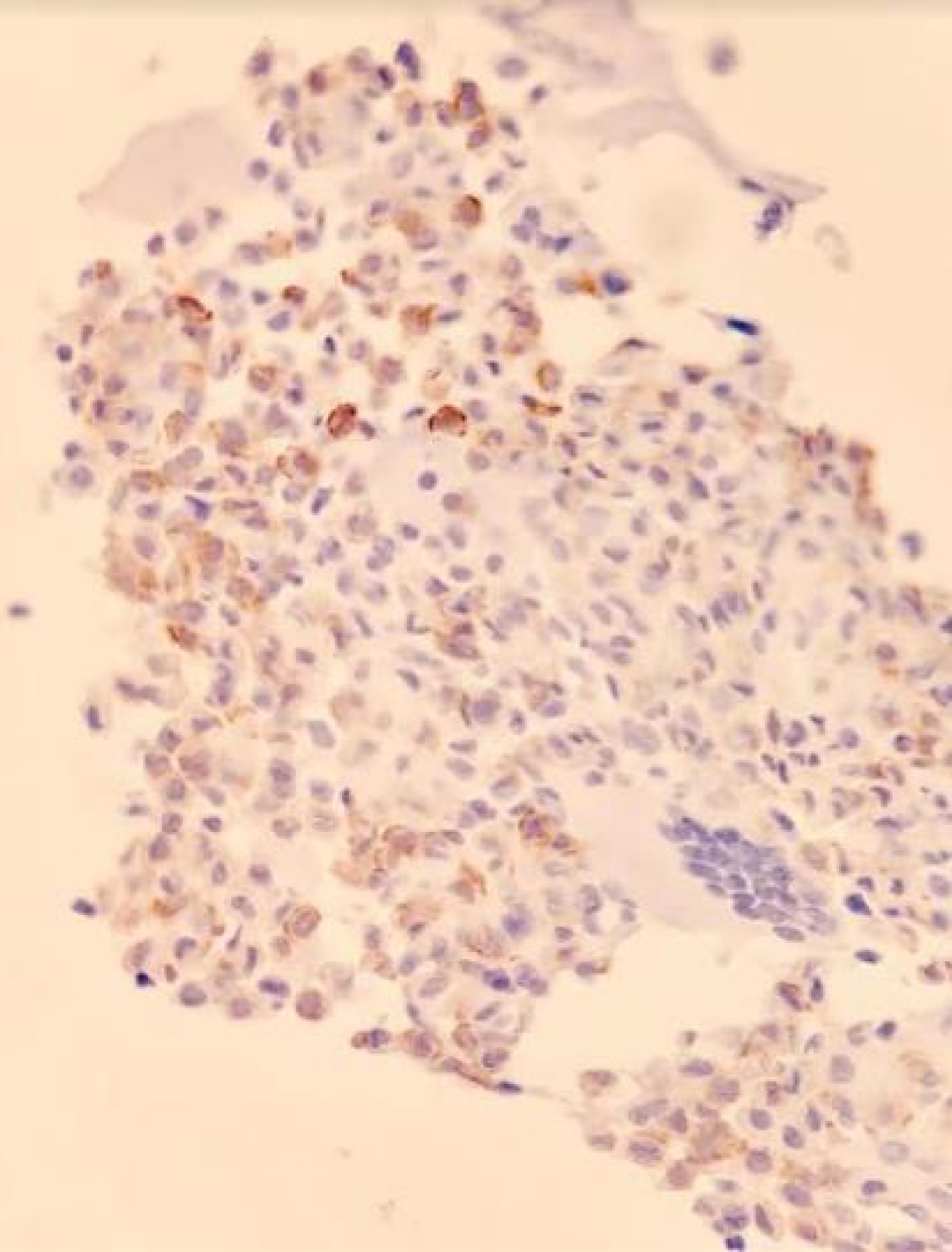
The pathology report showed sheats of epithelioid cells with nuclear clefts (Figure 15), rounded lobules of pink cartilage with individual calcifications in "chicken wire" appearance (Figures 16 and Figures 17) and giant cells. The chondroid components had reactivity for S100 and, if not specific, there was also reactivity to DOG - 1 (Figure 18). These findings are compatible to EC.
Discussion
EC located in the femoral head epiphysis, is characterized for a difficult access and frequent recurrence rate [2,8,11,18], in contrast with other locations previously described in literature. It is also a rare benign tumor (1-2% of all the primary bone tumors; 9% of benign bone tumors), with variable local aggressivity depending on its anatomic location [1-17,20,21]. It presents predominantly in male patients with a 2:1 relationship [1,2,4,16], as well as in long bones, specially in the humerus and the femur [4,5].
Although the final diagnosis is done by the lesion biopsy, the use of diagnostic aids like X-rays and CAT scan allow a better approach. Lesions are usually oval or rounded, well circumscribed, with lytic characteristics, affect the growth plate and produce a halo of sclerotic bone around them [4,16-18] as seen in our patient (Figure 1). Symptoms include pain (depending on the anatomical location), antalgic gait (when located in lower extremities) specially in articular locations [3,6,8,13,17,22].
Usually, poligonal chondroblast like cells are present, they are well circumscribed in the surface and posses cleft nuclei. At the same time, foci of cartilaginous matrix are present (pink chondroid) with focal calcifications that give the characteristic aspect of "chicken wire" [2-4,10]. There are several studies that evaluate the role of cartilaginous cells in the growth plates during development in the embrionary stage, concluding that this period is a key moment for the occurrence of these type of tumors through an important disturbance in the signaling paths that will favor the proliferation of cartilage producing cells [7]. As an interesting finding, an association between Aneurysmal Bone Cyst and EC has been identified in 14% of cases [2,4].
Nowadays there is no standard procedure for surgical management of EC [14,17,23], specially when located in the femoral head. Literature has described EC since 1927 and frequently states that complete resection of it through curettage should be a standard of care, including multiple options for covering the remaining defect, mainly by means of structural allograft [1-6,8-14,16,17,23,24].
Additionally, the use of phenol o cryosurgery has been described for enhancing the local treatment to reduce recurrence [4,8,9,11,12,25], nonetheless, its use is not frequent nor described in several publications [1-3,5,6,10,12-14,16]. Then, the main objective and prognostic factor for recurrence, is still the complete resection of the lesion [4,12,14,16]. This can be challenging depending on the anatomic localization of the EC, specially when located in difficult areas such as the femoral head [2,5,8,10,11,14,19]. Recurrence rates in the femoral head are diverse in contrast to other articular locations like the humeral head, which reports high recurrence [5,9,11,14,21].
Furthermore, the use of chemotherapy or radiotherapy, although once recommended as part of the treatment, is now proscribed as it can increase the risk for malignancy [2,4,25-27].
Tumoral recurrence can take place between 10-30% [1,2,4,5,9,10,14,28], being the incomplete resection the main prognostic factor, as stated before. There is also risk for malignancy of the benign lesion, as well as lung metastases in some cases [1,4,5,9,14].
In terms of complications, most studies do not report surgical complications. These ones are not frequent, do not happen in an acute stage and even in case of requiring additional surgeries, the functional results are adequate [1,9]. Among reported complications there are: Limb length discrepancy, heterotopic ossification and AVN [1,2,9,11,12,18,25,26]. Xu, et al. [11] reports a similar case to ours, describing AVN 4 months after the initial surgical procedure, with no recurrence in a patient intervened with the same "trap door" technique. However, there were no publications describing posterior dislocation and/or coxa magna. Despite the risk for AVN, the anterior approach is considered safe for the oncologic treatment of EC [28].
Conclusions
Management of this entity is still a matter for controversy nowadays, however, it is considered that complete resection of the lesion remains as the main prognostic factor for local recurrence. Surgical treatment is not without potential complications, although infrequent. In terms of the use of allograft for filling the resection gap, there is no consensus. Finally, the complication presented in our patient has not been described previously in literature related to the management of EC.
References
- Tiefenboeck TM, Stockhammer V, Panotopoulos J, et al. (2016) Complete local tumor control after curettage of chondroblastoma-a retrospective analysis. Orthop Traumatol Surg Res 102: 473-478.
- Strong DP, Grimer RJ, Carter SR, et al. (2010) Chondroblastoma of the femoral head?: Management and outcome. International Orthopaedics 34: 413-417.
- Qadri S, Ray P Sen, Sherwani RK, et al. (2014) Cytological diagnosis of chondroblastoma: Diagnostic challenge for the cytopathologist. BMJ Case Rep 1-4.
- Chen W, Di Francesco LM (2017) Chondroblastoma an update. Arch Pathol Lab Med 141: 867-871.
- Garin IE, Wang EHM (2008) Chondroblastoma. Journal of Orthopaedic Surgery 16: 84-87.
- Kaneko H, Kitoh H, Wasa J, et al. (2012) Chondroblastoma of the femoral neck as a cause of hip synovitis. J Pediatr Orthop B 21: 179-182.
- Romeo S, Bov J, Jadnanansing NAA, et al. (2004) Expression of cartilage growth plate signalling molecules in chondroblastoma. J Pathol 202: 113-120.
- Stilli S, Reggiani LM, Boriani L, et al. (2010) Osteochondral allograft in a femoral head chondroblastoma?: A case report. Hip Int 20: 280-283.
- Xu H, Nugent D, Monforte HL, et al. (2015) Chondroblastoma of Bone in the Extremities. J Bone Joint Surg Am 97: 925-931.
- Grimer RJ, Belthur M, Jeys L, et al. (2000) Chronology chondroblastoma of bone. J Bone Joint Surg Am 82: 1140-1145.
- Xu H, Niu X, Li Y, et al. (2014) What are the results using the modified trapdoor procedure to treat chondroblastoma of the femoral head?? Clin Orthop Relat Res 472: 3462-3467.
- Xiong Y, Lang Y, Yu Z, et al. (2018) The effects of surgical treatment with chondroblastoma in children and adolescents in open epiphyseal plate of long bones. World J Surg Oncol 16: 14.
- Fan J, Li S, Mei J, et al. (2016) Reconstruction with double pedicel fibular graft and ankle arthrodesis for aggressive chondroblastoma in the distal tibia. World J Surg Oncol 14: 143.
- Hsu C, Wang J, Chen C, et al. (2003) Results of curettage and high-speed burring for chondroblastoma of the bone. Chang Gung Med J 26: 761-767.
- Amary MF, Berisha F, Mozela R, et al. (2016) The H3F3 K36M mutant antibody is a sensitive and specific marker for the diagnosis of chondroblastoma. Histopathology 69: 121-127.
- Atalar H, Basarir K, Yildiz Y, et al. (2007) Management of chondroblastoma: Retrospective review of 28 patients. Journal of Orthopaedic Science 12: 334-340.
- Binesh F, Na R, Abrisham J (2013) Case report a fatal case of pure metaphyseal chondroblastoma. BMJ Case Rep 2013: 2-5.
- Lehner B, Witte D, Weiss S (2011) Clinical and radiological long-term results after operative treatment of chondroblastoma. Arch Orthop Trauma Surg 131: 45-52.
- Leunig M, Slongo T, Kleinschmidt M, et al. (2007) Subkapitale korrekturosteotomie bei der epiphyseolysis capitis femoris mittels chirurgischer hüftluxation subcapital correction osteotomy in slipped capital femoral epiphysis by means of surgical hip dislocation. Oper Orthop Traumatol 19: 389-410.
- Wang F, Li J, Yu D, et al. (2018) Chondroblastoma of the distal femoral metaphysis. Medicine 97: e0336.
- Ragab M, Mohamed H, Shady A (2013) Primary aggressive chondroblastoma of the humerus: An unusual imaging presentation. J Clin Imaging 37: 783-787.
- Dhanda S, Menon S, Gulia A (2015) Atypical giant chondroblastoma mimicking a chondrosarcoma. J Can Res Ther 11: 660.
- Lin PP, Thenappan A, Deavers MT, et al. (2005) Treatment and prognosis of chondroblastoma. Clin Orthop Relat Res 438: 103-109.
- Ryu JJ, Kim W, Lee JS, et al. (2017) Combined autograft and bone cement for painful chondroblastoma: A Case Report. J Foot Ankle Surg 10-14.
- Rybak LD, Rosenthal DI, Wittig JC (2009) Chondroblastoma: Radiofrequency ablation -alternative to surgical resection in selected cases. Radiology 251: 599-604.
- Xie C, Jeys L, James SLJ (2014) Radiofrequency ablation of chondroblastoma: Long-term clinical and imaging outcomes. Eur Radiol 25: 1127-1134.
- Dahlin DC, Ivins JC (1972) Benign chondroblastoma: A study of 125 cases. Cancer 30: 401-413.
- Jilong Y, Wei T, Xiongzeng Z, et al. (2012) Chondroblastoma in the long bone diaphysis: A report of two cases with literature review. Chinese Journal of Cancer 31: 257-264.
Corresponding Author
Carlos A Sanchez, Orthopedist and Traumatologist, Pontificia Universidad Javeriana, Hospital Universitario San Ignacio, Bogota, 110221, Colombia.
Copyright
© 2020 Sanchez CA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.