What is the Ideal Neurosurgical or Orthopedic Specialty Hospital?
Abstract
Specialty Hospitals provide a new element to any community they are centered in. A literature review was conducted to purpose what the most ideal speciality hospital would be. The goal of this literature review was to uncover advantages and disadvantages of a specialty hospital. Furthermore, this review will discover the various factors that affect a specialty hospital viability. A review was conducted through Google Scholar, PubMed and Federal Reserve Economic Data (FRED) databases. A total of 21 sources were found, which were peer review articles, case reports, and government and third party agency reports. Advantages were: Higher quality of care, increase of patient and physician satisfaction, lower adverse events and increased revenue. Disadvantages were: Higher costs, no tax exempt status when operating as a for-profit, accusations of cream skimming and stigma of physician ownership. The factors were: community’s perception, competition by other hospitals and stringent government laws and regulations. The ideal model for neurosurgical and or orthopedic specialty hospital is a not-for-profit institution that is acclaimed for its specialty and centered on a high levels of patient satisfaction.
Keywords
Specialty hospital, Neurosurgical, Orthopedic
Introduction
A Specialty Hospital adds a new dimension to any community that it serves. Specialty Hospitals are not a new concept. Psychiatric and Children's Hospitals are quite common and have a firm standing within the field of medicine, so much so that it has become the prominent standard of practice within these subspecialties.
A Specialty Hospital, as defined by the United States General Accounting Office, is a facility that produces greater than two-thirds of its claims from one to two major diagnostic categories (MDC), or two-thirds or more of its inpatient claims are contributed to a surgical diagnosis group (DRG) [1]. The theory is that a Specialty Hospital will bring focused treatment and care to its patients. In addition, it is claimed that it will decrease overall inefficiencies that other conventional or general hospitals endure.
When creating a Specialty Hospital, we must acknowledge that there are advantages and disadvantages. The advantages are sometimes the easiest standpoint to differentiate and potentially make this venture the most acceptable and profitable. Disadvantages may come about from different variables which could bring inefficiencies or increased expenditures. In addition to advantages and disadvantages, we also must look at stressors political, socio-cultural and competition [2], which may affect the development and existence of a specialty hospital. Therefore a literature review will be conducted to explore what are the advantages and disadvantages. Furthermore, it will look at what factors create the biggest influence on the viability and sustainability of a special hospital. Finally, we will attempt to create the ideal model of what we believe a specialty hospital should be.
Methods
A literature search was conducted in PubMed and Google Scholar. The following terms were searched: "specialty hospital", "neurosurgical specialty hospital" and "orthopedic specialty hospital". Additionally, references from previously published review articles were retrieved and included in this review. A search was also conducted on Federal Reserve Economic Data (FRED) database for up-to-date financial information.
Results
Advantages
A focus factory, as defined by Skinner, et al. 1974, will outperform a traditional factory [3]. This theory can be applied to Specialty Hospitals. A specialty hospital provides the highest quality of care. It also supplies the highest patient and physician satisfaction. From an economic standpoint, Specialty Hospitals are more efficient and profitable than general hospitals [4]. This is because they generally follow a philosophy that every physician focuses on a subset of procedures. The nursing and ancillary staff takes care of patients undergoing the same set of procedures and reporting to the same set of physicians [5,6].
The dynamic of the healthcare climate is ever changing. Individuals are becoming more involved in their healthcare choices. With the advent of the internet and social media, individuals have much more knowledge and subsequently higher expectations. These expectations are led by the need of a high quality of care and satisfaction [4]. Specialty Hospitals bring the highest quality by consistently focusing on their core competency. This directly brings about learning and process improvement [7]. In addition, when comparing a specialty to a general hospital, the ratio of nurse-to-patient is substantially higher. This will create an environment where the entire staff is more specialized in the specific specialty of interest. A study done by Padegimas, et al. 2018, found that the operating room efficiency was far greater in an orthopedic specialty hospital versus a tertiary referral center [8].
There have been a few studies comparing Specialty Hospitals with general hospitals by primarily looking at patient reported outcomes and mortality rate. For example, in Cram, et al. 2006, patients undergoing total hip and knee replacement, who had their procedures done at a Specialty Hospital, had better reported outcome when compared to patients having it done at a general hospital [9]. Another example, in Cram, et al. 2005, investigated the difference between patients receiving cardiac revascularization in Specialty Hospitals versus general hospitals, by examining patient characteristics, hospital procedural volume and patient outcomes. This study showed that there was a lower unadjusted mortality rate in patients receiving treatment at a Specialty Hospital. This difference was accounted for by a higher procedural volume and patients being generally healthier [10]. An example of recurrence rate, a study by Malik, et al. 2016, compared recurrence of a inguinal hernia after repair in a Specialty Hospital versus a general hospital. This study showed that Specialty Hospitals had a lower risk of recurrence when compared to a General Hospital [11]. There is also a decrease in other adverse events with hospital specialization. Studies have shown that Specialty Hospitals have a decrease in death, infection, deep venous thrombosis, pulmonary embolism, myocardial infarction, and bleeding [4,12,13].
Another study by Bockhorn 2019, compared orthopedic specialty hospital versus non-specialty hospitals when conducting total joint arthroplasty. This study found that specialty hospitals had statistically significant lower average covered costs, average total payments, average Medicare payments, readmission rates and complication rates when compared to non-speciality hospitals [14]. A study by Krietz, et al. 2019, compared patients receiving a lumbar fusion in a orthopedic specialty hospital versus a tertiary referral center. The specialty hospital has statistically significant lower operative time, total operating room time, and length of stay when compared a tertiary referral center [15].
Specialty Hospitals brings numerous benefits directly to the patients and their families. One benefit is that they focus greatly on patient satisfaction [4,5]. The Center for Medicare Services (CMS) report that Specialty Hospitals have greater patient satisfaction when compared to general hospitals [4,13]. Most procedures occurring at a Specialty hospital is elective in nature and that is attributed to patient satisfaction. Procedural schedule is immune from disruptions that are brought about by emergent cases.
By providing competition to General Hospitals, Specialty Hospitals are an asset to the community it is centralized in [13]. This drives General Hospitals to make advancements in their infrastructure and focus more on patient satisfaction [4,5]. Greenwald, et al. 2006 showed that the community benefited by Specialty Hospitals when compared to its not-for-profit counterparts. This can be equated to a higher uncompensated care cost and no tax exempt status [13].
Specialty Hospitals can be either not-for-profit or for-profit. Not-for-profit facilities are tax exempt while for-profit facilities are not. A for-profit facility will generate an increase of tax revenue for the community [5,6]. When comparing net community benefit a study showed that orthopedic/surgery hospitals had higher net community benefit than its competitors [16].
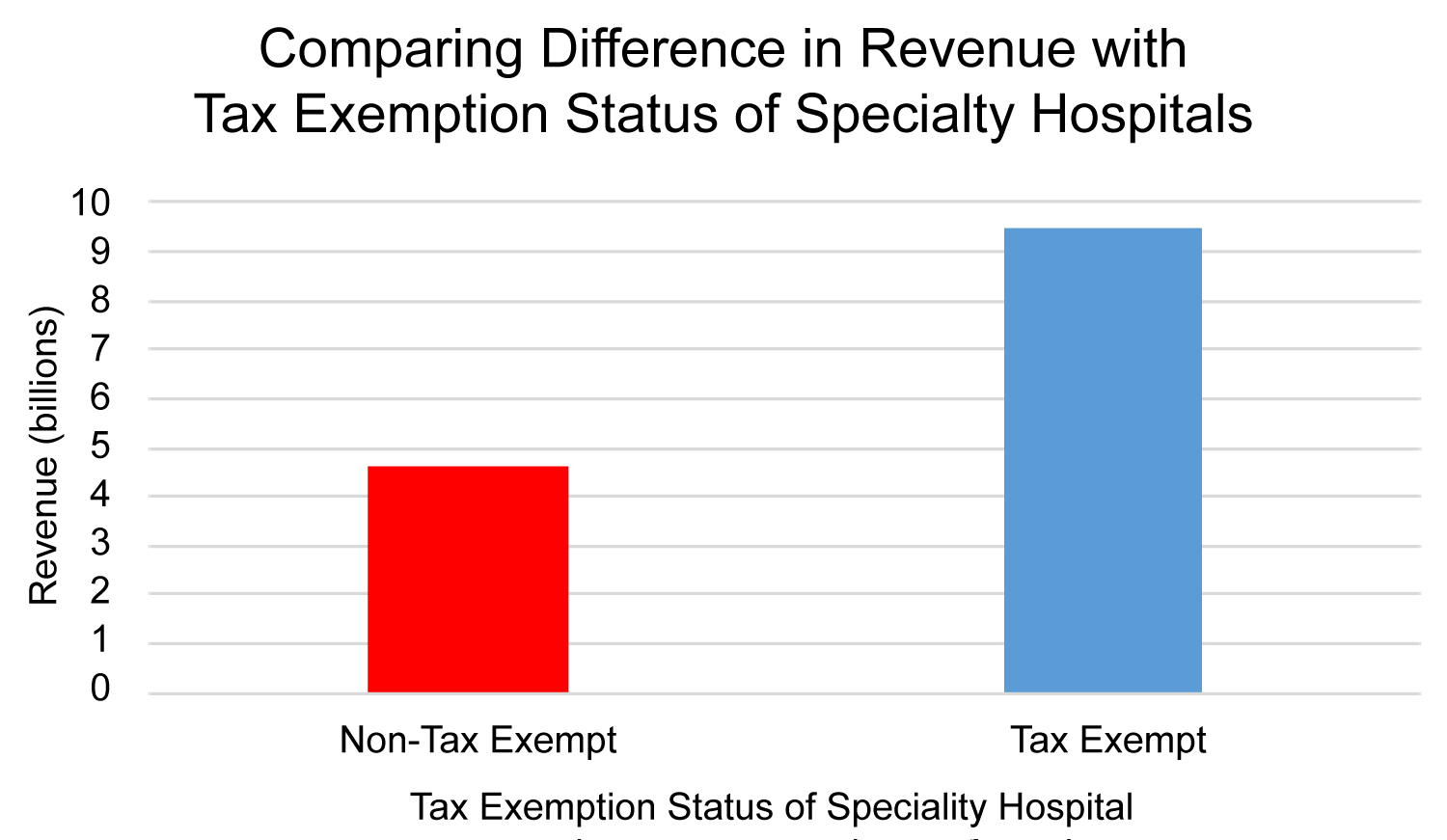
The financial performance of a hospital dictates its viability. A report by the General Accounting Office in 2003 showed that financial performance of Specialty Hospitals are greater than General Hospital across all payers. Additionally, a 2012 report by the US Census Bureau, specialty hospitals produced a total revenue of $33 Billion. This is a substantial increase because in 2002 specialty hospitals produced $14 Billion of total revenue [17]. In the span of 10 years, there was a 140% increase. When comparing revenue in facilities that did or did not utilize tax exemption, revenue in tax exempt specialty hospitals was 9.5 billion versus 4.6 billion in non-tax exempt specialty hospitals [18,19] (Figure 1).
Disadvantages
A hospital can be a very costly investment. Operating costs of a facility has a direct impact on profitability. The expenses for a specialty hospital, reported by the US Census Bureau from 2005 and 2012 was 3.8 and 6 billion dollars, respectively. A non-specialty hospitals expenses from 2005 and 2012 was 1.4 and 2 billion dollars, respectively [20,21] (Figure 2).
Specialty Hospitals are frequently scrutinized for their practices, especially for-profit institutions. They have been accused of taking patients who are healthier and better insured leaving the more complicated and emergent cases for General Hospitals. However, the data does not support this claim. Lu, et al. 2009 investigated Specialty Hospitals with General Hospitals and compared surgical volume and patient case complexity. There was no evidence to support that there was a significant difference in either of these metrics [22] and validated by the 2005 report by the Centers for Medicare & Medicaid Services [13].
The ownership of Specialty Hospitals by physicians could have a potential conflict of interest. This conflict of interest is further exacerbated by overuse of hospital services and can increase hospital costs [4]. Mitchel, et al. 2008 showed that a disproportionate amount of procedures rendered to patients by physicians who own a share of the hospital versus non-owners [23]. In another example, Swedlow, et al. 1992 showed self-referring physicians ordered more MRI scans when compared to an independent physician group [24]. In the 2005 Centers for Medicare & Medicaid Services report, a link was found between physician ownership and referrals, however this correlation was miniscule [13].
The final disadvantage of a specialty hospital is local and federal laws and regulations that impose restrictions and limitations. One such example of this is the Affordable Care Act of 2010 (ACA). ACA section 6001 amends section 1877 of the Social Security Act, which enforces physician-owned hospital to meet additional provisions to qualify for a whole hospital or rural provider exception. Furthermore, physician-owned hospital facilities are not allowed to increase their capacity [25]. This is very problematic since physician ownership of orthopedic/surgery specialty hospitals has averaged around 80% [16].
Discussion
A Specialty Hospital is disruptive innovation that permanently changes the nature of healthcare. A disruptive innovation is described as a new entrant in a market that competes with an incumbent [26]. The competition can be generated by many different methods and affecting various different channels. The competition brought by Specialty Hospitals is decentralization and decreased costs.
A Specialty Hospital thrives in an environment where they become the benchmark for that specific specialty. This facility will have an ability to form brand recognition for its consumers. Brand recognition is the ability of a company to form a product or service with potential value, and displaying this value to the consumers [27]. When developing a business model, the perceived value from the consumer is key as well as other components such as key resources, key processing, and profit formula [28].
The major key resources of a Specialty Hospital is surgical or medical specialization, which would primarily focus on one or two areas. A significant benefit is that this then calls for all levels of the employee hierarchy to fixate on this one specialty. Therefore building and modelling there infrastructure and staff around this one specialty. Forming this key resource will aid in the development of the hospital’s core competency.
With developed resources, will come key processing. When looking at a Specialty Hospital, all levels of the employee hierarchy needs to function and communicate with each other efficiently. The first process for the employee hierarchy is training. Training needs to be designed to teach the employees the most up to date and advanced equipment and methodology, while implementing it seamlessly and effectively.
The profit formula is very difficult to maximize with one of the major components being operational costs. Operational costs of a Specialty Hospital tends to be less when compared to a General Hospital. When implementing the best infrastructure where all stakeholders are in agreement, operational cost should be a top-down cost approach. The top-down cost approach positions the most expensive item or service at the top of the balance sheet [29]. For example, a da Vinci robotic system costs approximately $2.6 Million [30]. The hospital will structure their profit formula around the robot and adjusting other fixed and variable costs to achieve the highest profitability.
Specialty Hospitals has a reputation of "cream skimming" and self-referring patients. Cream skimming is choosing patients based on particular qualities and not based on need for care, but rather health insurance [31]. We propose one way to prevent both situations is creating a specialty hospital that is completely not for profit. This will completely eliminate physician’s conflict of interest. Moreover, making a specialty hospital not for profit will make the hospital more suitable to comply with regulations set by the ACA. It is imperative that the developers of the specialty hospital work collaboratively with government bodies and regulatory agencies. Lastly, as a not-for-profit status will award the facility with tax exemption, and as have reports have shown it will increase the cash flow. The only downside of tax exemption status is that it will decrease community benefit. Previously taxation of for-profit institutions generated a significant amount of revenue for the community. We also propose that inspiring institutions implement public outreach and community services. This could potentially alleviate the factor of socio-culture pressure that may exist in the market against specialty hospitals. Examples of community outreach activities would include donating money to notable charities, sponsoring and holding health fairs, etc.
Conclusion
The ideal specialty neurosurgical or orthopedic hospital would be a not-for-profit institution that focus its infrastructure and staff on one specialty. The hospital should base their mission statement on providing the best quality of care and satisfaction to all their patients. Furthermore, while operating as not-for-profit to utilize a tax exempt status to achieve the highest profitability. Finally, new inspiring institutions should work closely with regulatory bodies and government authorities when developing this new facility.
References
- Gao G (2003) Specialty hospitals: Geographic location, services provided, and financial performance. General Accounting Office, Washington, DC, 1-41.
- Perera R (2017) The pestle analysis. Nerdynaut.
- Skinner W (1974) Focused factory. Harvard Business School Reprint.
- Badlani N, Boden S, Phillips F (2012) Orthopedic specialty hospitals: Centers of excellence or greed machines? Orthopedics 35: e420-e425.
- Blackstone EA, Fuhr JP Jr (2007) Specialty hospitals: The economics and policy issues they pose. J Health Care Finance 34: 1-9.
- Greenwald L, Cromwell J, Adamache W, et al. (2006) Specialty versus community hospitals: Referrals, quality, and community benefits. Health Aff 25: 106-118.
- Schneider JE, Miller TR, Ohsfeldt RL, et al. (2008) The economics of specialty hospitals. Med Care Res Rev 65: 531-553.
- Padegimas EM, Hendy BA, Chan WW, et al. (2019) The effect of an orthopedic specialty hospital on operating room efficiency in shoulder arthroplasty. J Shoulder Elbow Surg 28: 15-21.
- Cram P, Vaughan-Sarrazin MS, Wolf B, et al. (2007) A comparison of total hip and knee replacement in specialty and general hospitals. J Bone Joint Surg Am 89: 1675-1684.
- Cram P, Rosenthal GE, Vaughan-Sarrazin MS (2005) Cardiac revascularization in specialty and general hospitals. N Engl J Med 352: 1454-1462.
- Malik A, Bell CM, Stukel TA, et al. (2016) Recurrence of inguinal hernias repaired in a large hernia surgical specialty hospital and general hospitals in Ontario, Canada. Can J Surg 59: 19-25.
- Hagen TP, Vaughan-Sarrazin MS, Cram P, et al. (2010) Relation between hospital orthopaedic specialisation and outcomes in patients aged 65 and older: Retrospective analysis of US Medicare data. BMJ 340: c165.
- Jerry Cromwell, Walter Adamach, Shulamit Bernard, et al. (2005) Specialty hospital evaluation final report. Centers for Medicare & Medicaid Services 187.
- Bockhorn LN, Goytia RN, Laughlin MS, et al. (2019) Increased orthopedic specialization lowers costs and improves outcomes in total joint arthroplasty. J Arthroplasty 34: S76-S79.
- Kreitz TM, Tarazona D, Padegimas EM, et al. (2019) Comparison of short-term outcomes after lumbar fusion between an orthopedic specialty hospital and tertiary referral center. Spine 44: 652-658.
- Leavitt MO (2005) Study of physician-owned specialty hospitals required in section 507 (c)(2) of the medicare prescription drug, improvement, and modernization act of 2003. US Department of Health and Human Service, Baltimore, USA.
- (2019) Total revenue for specialty hospitals-private, all establishments, employer firms.
- (2019) Total revenue for specialty (except psychiatric and substance abuse) hospitals, establishments subject to federal income tax.
- (2019) Total revenue for specialty (except psychiatric and substance abuse) hospitals, establishments exempt from federal income tax.
- (2019) Total expense for hospitals, all establishments.
- (2018) Total expense for specialty hospitals - government, all establishments, employer firms (Discontinued).
- Lu X, Hagen TP, Vaughan-Sarrazin MS, et al. (2009) The impact of physician-owned specialty orthopaedic hospitals on surgical volume and case complexity in competing hospitals. Clin Orthop Relat Res 467: 2577-2586.
- Mitchell JM (2008) Do financial incentives linked to ownership of specialty hospitals affect physicians’ practice patterns. Med Care 46: 732-737.
- Swedlow A, Johnson G, Smithline N, et al. (1992) Increased costs and rates of use in the california workers’ compensation system as a result of self-referral by physicians. N Engl J Med 327: 1502-1506.
- (2019) Physician Owned_Hospitals, Centers for Medicare and Medicaid Services, Baltimore, USA.
- Christensen CM, Raynor ME, McDonald R (2015) What is disruptive innovation. Harv Bus Rev 93: 44-53.
- Karjalainen T-M, Snelders D (2010) Designing visual recognition for the brand*. The Journal of Product Innovation Management 27: 6-22.
- Johnson MW, Christensen CM, Kagermann H (2008) Reinventing your business model. Harv Bus Rev 86: 57-68.
- (2015) Cost Estimating: Bottom-Up vs. Top-Down.
- Ho C, Tsakonas E, Tran K, et al. (2011) Table 16, capital and operating costs of da vinci surgical system*. Canadian Agency for Drugs and Technologies in Health.
- Friesner DL, Rosenman R (2009) Do hospitals practice cream skimming? Health Serv Manage Res 22: 39-49.
Corresponding Author
Sukhbir Singh, MD, Brain and Spine Surgeons of New York, White Plains, New York, USA.
Copyright
© 2020 Singh S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.