Caring for People with Alzheimer's Disease Who Show Defensive Behaviours. Part 2: Situation-Specific Fundamentals of Care Practice Process
Abstract
This article amis to present a clinical practice process which is essential for nurses and nursing students caring for people living with Alzheimer's disease (AD) who show defensive behaviours. This discursive paper introduces the Defensive Behaviours Practice Process based on relevant nursing knowledge previously presented. The Defensive Behaviours Practice Process is presented with an algorithm and a clinical form. A clinical scenario presents Mrs. Barbara Henderson, 80, who shows defensive behaviours. We can follow the nurse Florence in her first stages of clinical process with Mrs. Henderson, her family and the formal caregivers. Several tools are integrated in an innovative way, for example a Retrogenesis genogram and ecomap. The Defensive Behaviours Practice Process integrates the main stages nurses should realize for a person living with AD who show defensive behaviours. The process helps the nurse to identify compromised needs and to plan relevant interventions with the person, family and nursing team.
Keywords
Dementia care, Fundamental care, Nursing practice, Nursing process, Aggression management, Family-Centred care 3
List of Abbreviations
AD: Alzheimer's Disease; FOC: Fundamentals of Care
Aim
This article presents the second part of our proposal on how to use nursing knowledge for the care of people living with Alzheimer's disease (AD) who show defensive behaviours. The https://scholars.direct/Articles/nursing/jnp-4-039.php?jid=nursing presented a knowledge structure composed of four essential pieces of nursing knowledge in association with a perspective on nursing practice. This article aims to present a Situation-Specific Fundamentals of Care Practice Process which is essential for nurses and nursing students caring for people living with AD who show defensive behaviours.
Background
Aggressive behaviours shown by people living with AD are quite frequent in nursing homes. These behaviours may have disastrous consequences for the person living with AD but also for all other people involved in their life or care, namely, family members, nursing staff, students, and other residents. The aggressive behaviours should be understood as being significant behaviours related to several triggers such as compromised needs and environmental factors. In fact, it is essential to understand that aggressive behaviours are usually related to discomfort or perception of threat. Such experiences and perceptions can lead people living with AD to show protective and defensive behaviours. Therefore, we will not use the term "aggressive" to describe the behaviours of persons living with AD. Indeed, as explained in the first part of this article, the perspectives of protective and defensive behaviours and that of the relationship-centred care have been chosen for our proposal. It is therefore essential for nurses to understand this defensive perspective and to identify the triggering factors. As suggested in Part 1, knowledge is critical in identifying the triggering factors, understanding the goal of the defensive behaviours and deciding how to respond to the person's specific needs.
In the first part of the article, we presented a vision of nursing practice and the corresponding essential pieces of knowledge to take care of people living with AD who show defensive behaviours. Considering that the first part provides the essential knowledge and is a prerequisite for the reading of the second part, we strongly suggest that the reader start with the first part before moving on to the second one. A simple reminder of the main components of the first article is presented here to introduce this second part, which presents a concrete application of our knowledge structure.
Focusing on the Fundamentals of Care (FOC) Framework, and from a relationship-centred care perspective, we introduced the defensive behaviours essential pieces of knowledge and illustrated them with a prismatic mid-paradigm showing the main components of our proposal. This mid-paradigmatic representation of knowledge and defensive behaviours demonstrated how components of nursing knowledge take shape around the defensive behaviours, allowing nurses to address this complex situation. The mid-paradigmatic proposal also demonstrated the importance of a relationship-centred care approach. Indeed, it is crucial to consider this approach since it takes into account the relationships between the persons living with AD who show defensive behaviours, their family members, other residents living in the unit, as well as the nurse, the nursing team, and the nursing students. Moreover, we also described different theories and data that were consolidated to build the mid-paradigmatic proposal. Therefore, we identified four essential pieces of knowledge, which are: 1) Characteristics of the person living with AD showing defensive behaviours, 2) The goals of the defensive behaviours, 3) The contributing factors, and 4) The needs and senses centred interventions.
Discursive Paper
This discursive paper is intended for all nurses who care for people living with AD who show defensive behaviours regardless of practice areas or clinical settings. This article targets nurse educators, internship supervisors, counsellors or managers, as well as nursing students. This second part of the article introduces the FOC Practice Process specific to the person living with AD showing defensive behaviours.
First, we will introduce the FOC Practice Process. After that, considering the proposals made in the first part of the article, we will present the FOC Practice Process specific to persons living with AD who show defensive behaviours which will be called the Defensive Behaviours Practice Process. Second, a clinical illustration will present the process carried out by Florence, a nurse, with Mrs. Barbara Henderson, a nursing home resident. Inspired by the examples of Feo, Rasmussen, Wiechula, Conroy, and Kitson [1] and Feo, Conroy, Alderman, and Kitson [2] we have incorporated reflective timeouts. These reflective timeouts allow the reader to become involved in Mrs. Henderson's situation and take ownership of the process. This will be useful for demonstrating the main steps and useful insights for understanding the Defensive Behaviours Practice Process. Finally, we will talk about the relevance of our proposal to clinical practice.
The Fundamentals of the Care Practice Process specific to the care of people showing defensive behaviours
In order to illustrate the relevance of the recommendations given in the first part of this article and to promote their practical use, a version of the Fundamentals of Care (FOC) Practice Process elaborated specifically for people showing defensive behaviours will be used. The first part of this article presents the FOC Practice Process including the new specific version of it for people living with AD who show defensive behaviours. Subsequently, a clinical illustration will introduce Mrs. Barbara Henderson's story.
The fundamentals of care practice process: The Fundamentals of care (FOC) Practice Process helps nurses apply the FOC Framework in concrete situations of care [2]. As mentioned in Part 1, the FOC Framework integrates three dimensions, labelled as: 1) Relationship established, 2) Integration of care, and 3) Context of care [3,4]. The FOC Practice Process presents five successive and iterative stages that guide the nurse in his or her clinical approach [3,2]. The FOC Practice Process consists of five iterative stages that are briefly presented here. More details can be found in Conroy, et al. [3] and Feo, Conroy, et al. [1] writings.
The first stage is related to concepts. This stage is centred on observation and reflection. As a first stage, it permits the nurse to initiate his or her clinical process with the person. It encourages the nurse to explore his or her ideas and opinions, as well as his or her tacit knowledge of the situation. In terms of clinical assessment, this first stage also helps specify the facts describing what is known and observed. This first stage is most often a prerequisite to the use of the theory helping the nurse to understand the situation and to seek interventions that are relevant to the individual and his or her family. The second stage is centred around a working hypothesis elaborated by the nurse, which will guide the following process. The working hypothesis is centred on the identification of the person's needs to be addressed. The third phase integrates the FOC Framework into the Practice Process. Thus, the three dimensions of the FOC Framework, namely, relationship, integration of care, and context of care, are integrated in the Practice Process. The fourth stage incorporates theories sustaining the nurse in his or her clinical assessment and in-situation reflection. The theory is essential for analyzing and understanding the person's situation, as well as to propose relevant explanations to the person and their family and to other formal caregivers and interprofessional team members. The theory also guides the nurse to find solutions that are appropriate for responding to the person and family's needs. Finally, the fifth stage targets the clinical reasoning process. This involves all the different activities related to the care plan, clinical follow-up, and care outcomes evaluation.
Situation specific proposal: The Fundamentals of Care Practice Process for people living with Alzheimer's who show defensive behaviours
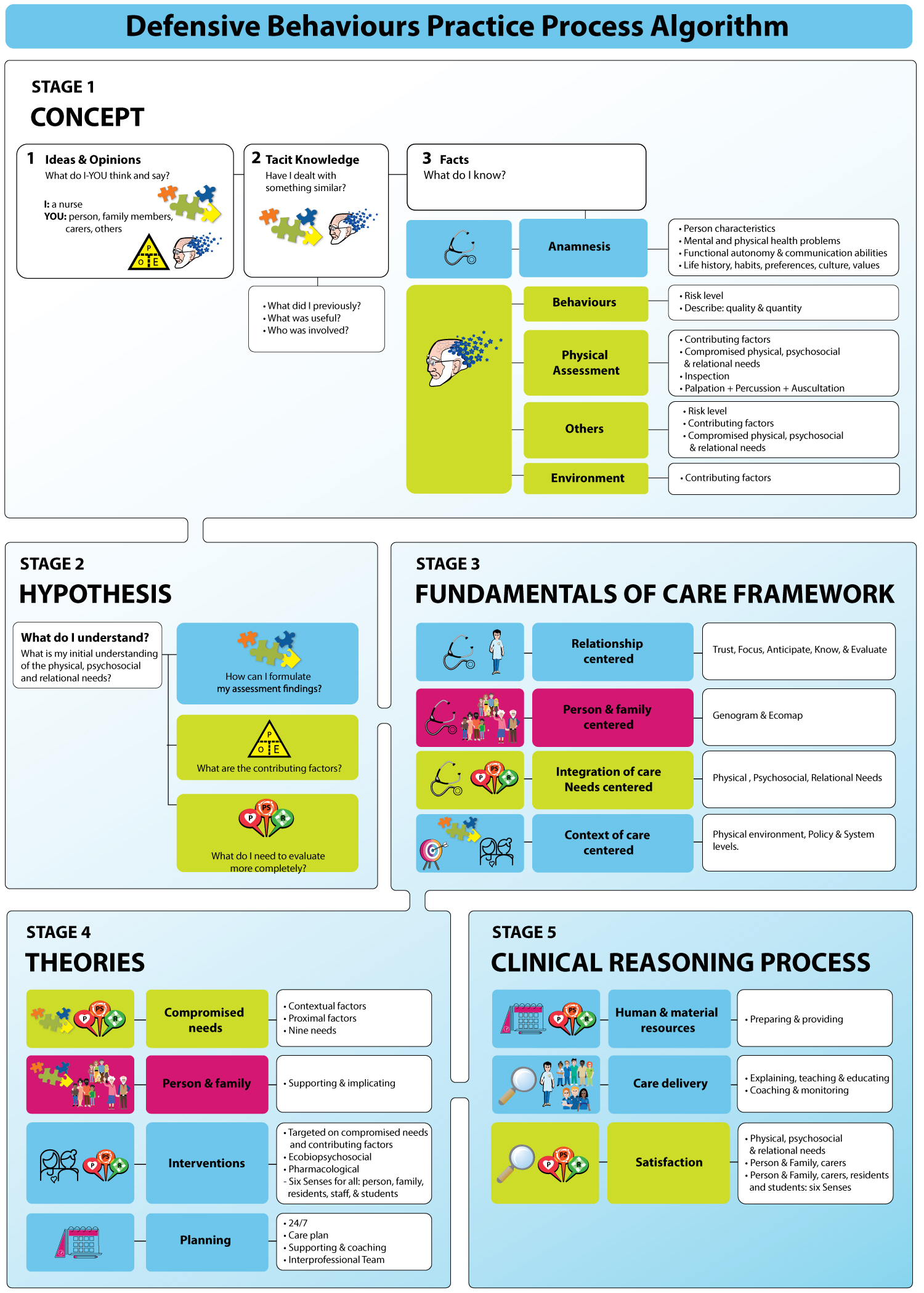
The use of the FOC Practice Process for people living with AD showing reactive behaviours has already been presented [5]. The need to develop a situation specific FOC Practice Process for people living with AD who show defensive behaviours appeared during the process of the academic, clinical, and research achievements of some of the authors. Staying within a situation specific perspective and wishing for the ease of use in nursing practice, we have consequently modified the presentation of the shape of the FOC Practice Process. In this way, the shape has been transformed into an algorithm https://scholars.direct/Articles/nursing-practice/jnp-4-042-Figure-1.pdf. This algorithm presents the most important components of the FOC Practice Process specific to the situation of a person with AD who shows defensive behaviours and their family. This algorithm can be used by all nurses and nursing students caring for these people. It integrates the structure of knowledge presented in Part 1 without replacing it. For the sake of conciseness, the situation specific FOC Practice Process for people living with AD who show defensive behaviours will be referred to as the Defensive Behaviours Practice Process.
Another more detailed clinical form which can be useful for less experienced nurses or students is proposed in Appendix 1. This second configuration takes the shape of a step-by-step check list that is more precise than the algorithm, and that can be completed during the clinical process. This clinical form illustrates the knowledge structure presented in Part 1 but cannot replace it.
Appendix 1: Defensive Behaviours Practice Process - clinical form
Now, the FOC Practice Process for people living with AD who show defensive behaviours will be presented through Mrs. Barbara Henderson's story. This clinical scenario and its figures were originally designed in French for education on the Retrogenesis phenomenon and defensive behaviours as well as FOC Framework and Practice Process [6-10]. The initial scenario has been translated to English for this article.
Clinical Illustration: Mrs. Barbara Henderson
We invite you to put yourself in the work shoes of Florence, a nurse who has been working in a nursing home for some years. Returning from a one-week vacation, Florence is back on the ward where she usually works on the evening shift.
The team describes several behaviours shown by Mrs. Barbara Henderson that lead to situations of tension and conflict not only with formal carers, but also with other residents and even family members (Table 1).
Since Florence took part in a workshop on the Defensive Behaviours Practice Process 10 days ago, she decides to use this method with Mrs. Henderson. As it is her first time using it, she decides to use the proposed Defensive Behaviours Practice Process clinical form rather than the algorithm, since the form is more detailed (Appendix 1).
Reflective time out 1 - stage 1: Concepts
|
Considering the Defensive Behaviours Practice Process form (Appendix 1), what can you do first? What about your ideas, opinions, and tacit knowledge? What are the facts you know? What are the essential elements you need to gather while addressing Mrs. Henderson’s situation? |
Having thought through her ideas and opinions, Florence decides to prioritize Mrs. Henderson since her behaviours probably mean that she has compromised needs, and because her behaviours have a negative impact on her own well-being, her family, and other residents. Florence also knows that the situation is difficult for the care aids. Related to her tacit knowledge, Florence remembers several residents who showed defensive behaviours. Some situations were extremely difficult to deal with, and restraints needed to be used. Florence thinks that having a practical process can guide her and help her understand the overall situation and find relevant interventions.
Florence collects some data from the file. She notes that Mrs. Henderson has been living in the nursing home for only six days. Her overall state of health is good a part from Alzheimer's disease at the stage 6a. This means that Mrs. Henderson needs help for her instrumental activities of daily living and that she is disoriented in time and space. Florence remembers too, that the care aids explained that Mrs. Henderson often thinks that she is in her late 30s, which is related to the Retrogenesis phenomenon. Florence also takes notes of Mrs. Henderson's life story milestones (Table 2).
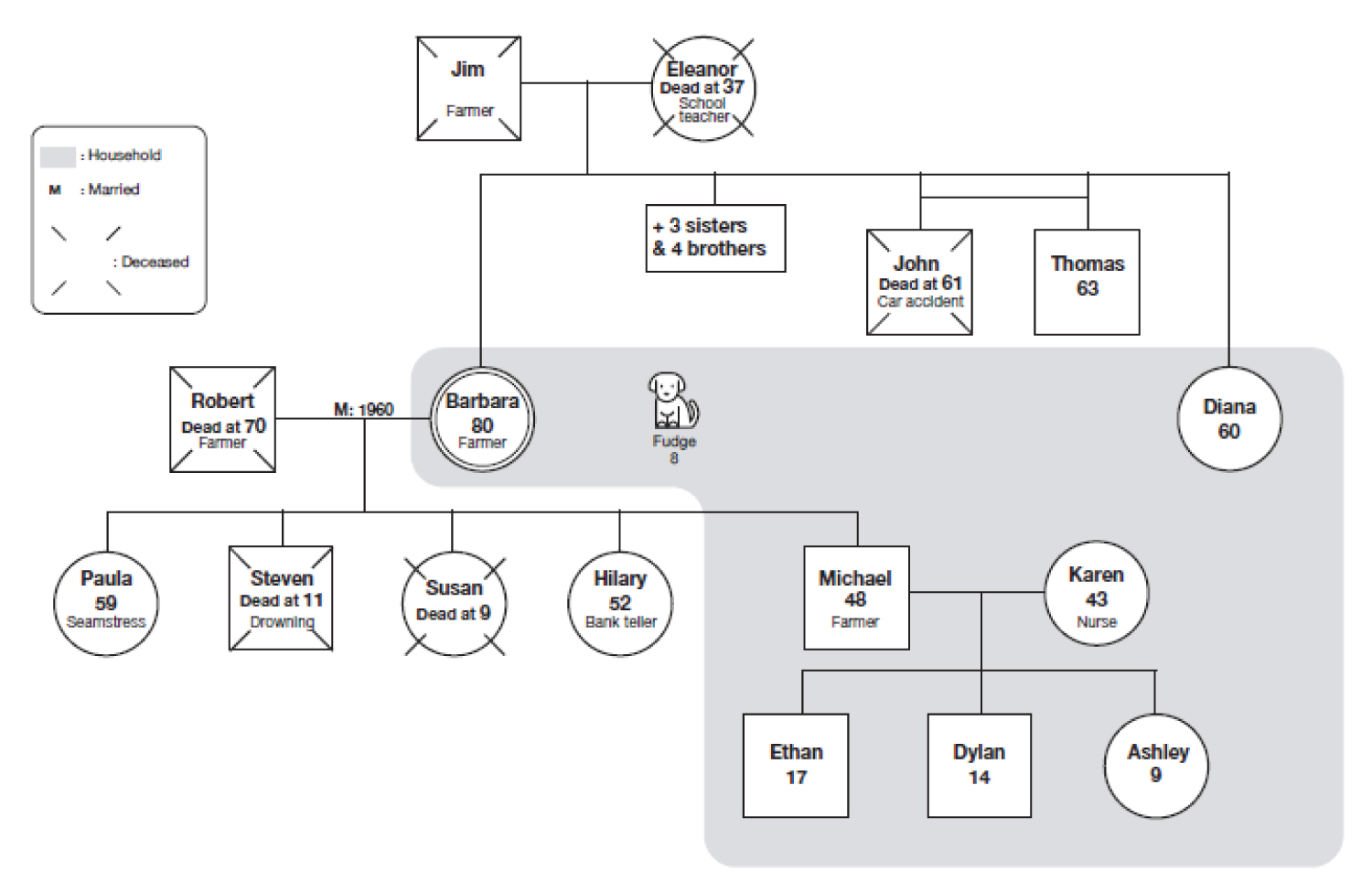
Through Mrs. Henderson's file, Florence can find interesting pieces of information. Therefore, with the data and life story collected from the family members, Florence can construct a genogram (Figure 2). This genogram allows us to graphically present three generations of Mrs. Henderson's family [11]. Because this genogram presents the family as it is today, we call it the "current genogram."
Reflective time out 2 - stage 2: Working hypothesis
What is your first hypothesis? How can you formulate your initial understanding?
Florence's initial working hypothesis is related to several compromised physical, psychosocial, and relational needs. She decides to begin the assessment process but is not sure where to start. She remembers some theoretical cues that were presented during the workshop on the Defensive Behaviours Practice Process. She refers to the clinical form.
Reflective time out 3 - stage 4: Theories
Without looking at the Defensive Behaviours Practice Process form, which theoretical explanations could be useful in Mrs. Henderson's situation? Which ones would you use to guide your clinical assessment process?
Florence looks at the Defensive Behaviours Practice Process form and remembers the contextual and proximal factors to be considered as well as the specific nine needs described by Boettcher. Florence also remembers the importance of involving significant family members. She decides to phone Mrs. Henderson's son Michael, who is the legal guardian. They decide to meet at 7 p.m., where Michael will come with his aunt, Diana, whom he describes as one of the people most important to his mother. Once that is done, Florence goes to Mrs. Henderson to get to know her and proceed to her assessment.
Reflective time out 4 - Stage 1: Facts
What would be your process? Knowing the aforementioned facts, what would you assess more precisely? Bearing in mind the Defensive Behaviours Practice Process, what could you consider evaluating?
At 4:30 p.m., Florence decides to proceed to a physical assessment, made through inspection. She introduces herself and proposes to Mrs. Henderson to have an appointment in her room. Mrs. Henderson accepts immediately, saying she is happy to receive visitors. During the assessment, Florence states that Mrs. Henderson is alert and attentive. Mrs. Henderson explains that she feels good and has no health problems or worries. She has no pain and can walk easily without instability. Florence also observes Mrs. Henderson's physical environment, which is her room. She notes there are only a few personal things: Some pictures without identification or explanation, three poetry books, some choir music CDs, two plush dogs, candies, personal toiletries, and clothes. There is no television but there is a radio with a CD player. The bedding is that of the establishment.
Mrs. Henderson says she wants to go home to take care of her children and her farm and asks Florence when she can return there. Using the Validation® Approach strategies, Florence helps Mrs. Henderson to speak of her life and explain all the daily activities and worries she is convinced she must manage as a mother, wife, and farmer. After three or four minutes, Florence uses diversion, guiding Mrs. Henderson to the dining room for dinner. There, Mrs. Henderson helps a care aid prepare the tables and fold napkins.
During the dinner, Florence can observe interactions between Mrs. Henderson, the caregivers, and other residents. She notes that Mrs. Henderson, rather than setting down and eating, is helping serve the meals and clean up. The two carers in the dining room repeatedly ask Mrs. Henderson to sit down and eat, which she does, but only after the soup is finished and the main dish has been served to every resident. Then, Mrs. Henderson intervenes several times with people seated at her table, telling them authoritatively what they should do, that is, to eat and finish the contents of their plate. A resident shows impatience with her, and her neighbour asks her to "shut up."
Florence records some elements regarding the contextual and proximal factors as well as Boettcher's nine needs (Table 3).
Reflective time out 5 - Stage 3: FOC framework.
Look at the FOC Framework dimensions: what about the relationship dimension and its five elements? What about the integration of care dimension and Mrs. Henderson's physical, psychosocial and relational needs? What can you observe regarding the context of care dimension?
With the Defensive Behaviours Practice Process form, Florence makes a list of Mrs. Henderson's most important physical, psychosocial, and relational needs. As she is doing this, and because she considers the relationship-centred perspective of care proposed by the Defensive Behaviours Practice Process (see Part 1 of this article), Florence decides to also consider family members' and other residents' fundamental needs (Table 4).
Considering the context of care, Florence notes again the importance of personalizing Mrs. Henderson's room with significant belongings. Thinking about the organizational environment, she notices some elements that the staff need to understand. At the policy level, because there are some issues related to the safety and well-being of Ms. Henderson, her family, other residents, visitors, and staff, Florence decides to ask her boss for a meeting. Finally, regarding the system level principle, Florence leaves a message for the nurse advisor, asking for coaching on her approach with the Defensive Behaviours Practice Process.
Florence realizes that this work will help her identify the interventions she needs to plan for Mrs. Henderson, her family, and other residents, as well as priorities for care. Now, Florence asks herself how to summarize Mrs. Henderson situation clearly, so she can formulate a working hypothesis and explain the situation to the family members as well as the nursing staff members and the interprofessional team.
Reflective time out 6 - Stage 4: Theories
What explanation would you choose to clearly explain Mrs. Henderson situation? What could be useful for better understanding Mrs. Henderson's needs and behaviour goals? What could guide you to the identification of relevant interventions?
Florence consults the Defensive Behaviours Practice Process form (Appendix 1). She establishes that the Retrogenesis experience of Mrs. Henderson is fundamental to understand the situation, to establish a working hypothesis, and to identify interventions to implement. Further more, based on the Retrogenesis explanations, Florence can prepare some important explanations for Mrs. Henderson's experiences and behaviours for the family's members and formal carers.
Reflective time out 7 - Stage 2: Working hypothesis
At this point in the Defensive Behaviours Practice Process, what would be your working hypotheses? How would you formulate them?
Florence writes her clinical notes in Mrs. Henderson's file and decides to formulate her clinical hypotheses as follows: Retrogenesis experience creating a need for meaningful activities related to the person's life roles and a need to express the person's emotions and feelings.
Reflective time out 8 - Stage 4: Theories
Imagine you meet Mrs. Henderson's son Michael and sister Diana: What would your objectives be? What about your strategies? What would be the most important elements to share with them?
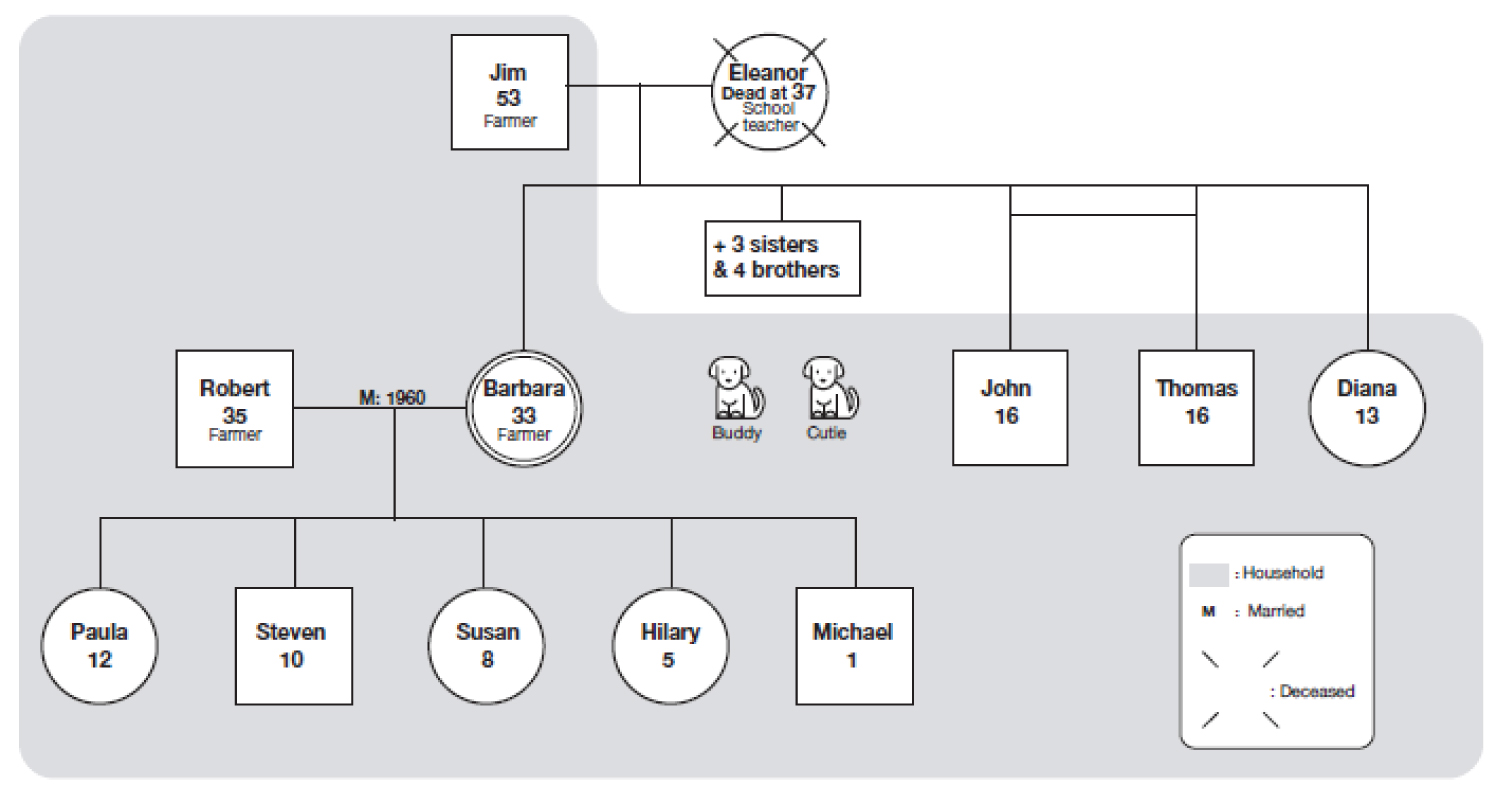
It is possible to conduct a meaningful and helpful 15-minute family interview [12]. Florence plans with the team to organize a 20-minute meeting with Mrs. Henderson's family. Because it is her first meeting with the family and the time available is limited, Florence decides to meet the family members without Mrs. Henderson, to facilitate the family's engagement in the therapeutic conversation. To better illustrate the Retrogenesis phenomenon experienced by Mrs. Henderson, Florence decides to draw a genogram of the family when Mrs. Henderson was around 33-years-old (Figure 3).
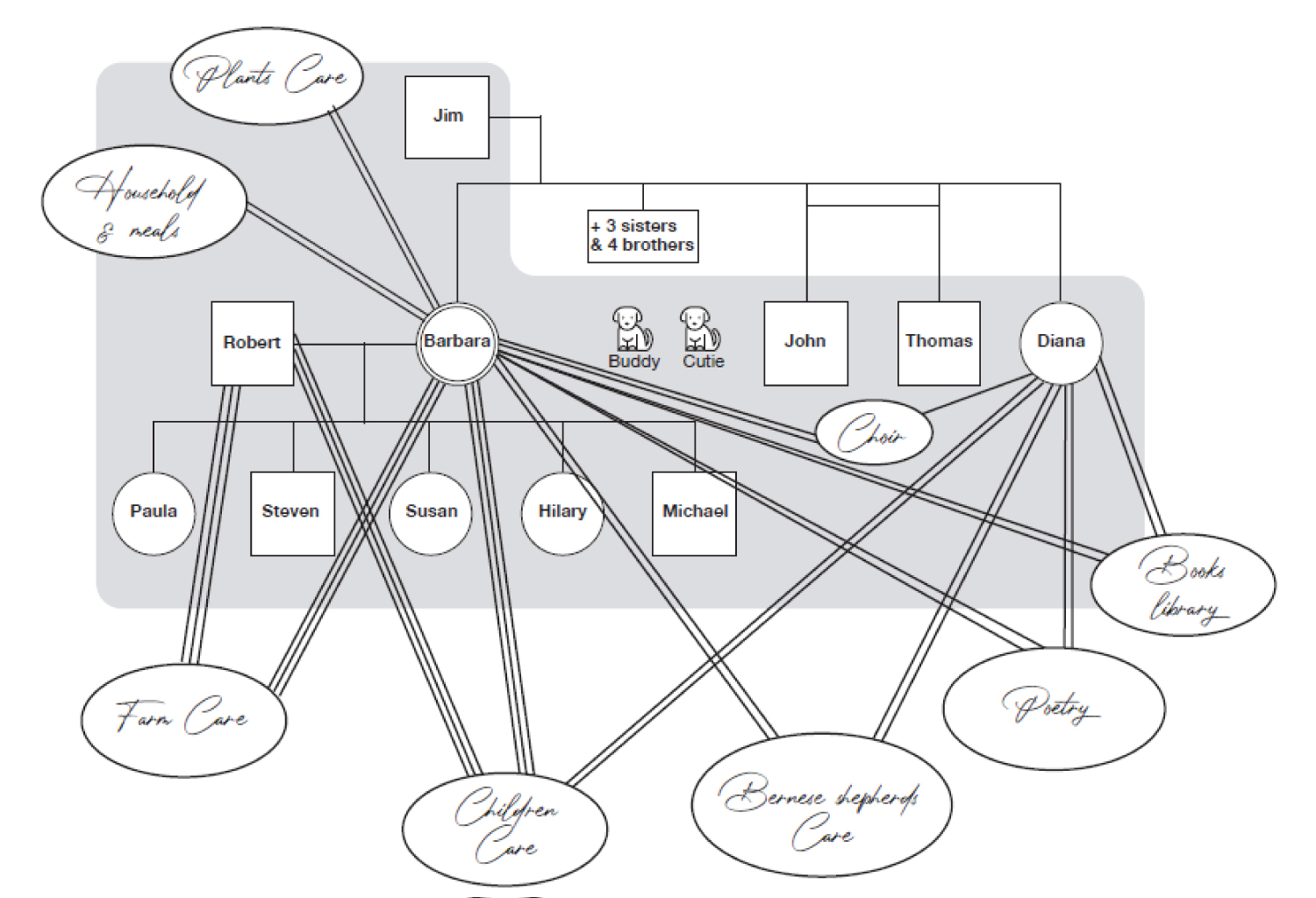
Florence also prepares key points that she will discuss with Michael and Diana, i.e., 1) Presentation and purpose of the meeting (2 minutes); 2) Explanation of assessment findings: Fundamental and compromised needs (3 minutes); 3) Genogram and Retrogenes is genogram (4 minutes); 4) Main principles of the Validation® Approach and resources (2 minutes); 5) Mrs. Henderson's Retrogenesis Ecomap and interventions to plan (7 minutes); and 6) Proposing regular family meetings and support (2 minutes).
Reflective time out 9 - stage 1: Facts
Now imagine that you are with Mrs. Henderson's family. You know you have only 20 minutes to meet them. How would you begin the meeting?
Now, Florence is sitting with Michael and Diana. The first four parts of the meeting have been completed. Michael and Diana found Florence's explanations on Retrogenesis very interesting. They asked her for a copy of the two genograms to explain them to other family members. Florence agrees to give copies of the two genograms, and proposes a future meeting for all the family, if needed. Now, Florence asks Michael and Diana to help her understand some of Mrs. Henderson behaviours and to identify some preliminary strategies to implement. She asks them to think about the Retrogenesis phenomena, in other words, to think about a previous time in Mrs. Henderson's life. Here are some examples from their discussion (Table 5).
During this discussion, Florence adds some elements to the Retrogenesis genogram to draw Mrs. Henderson's Retrogenesis ecomap which depicts the nature and the quality of her meaningful activities (Figure 4).
After closing the meeting, Florence reminds Michael and Diana that she will be there to meet and support them. With Michael being very busy at the farm around this time of the year, Florence and Diana plan another meeting three days later. Florence accompanies Michael and Diana to Mrs. Henderson, where she leaves them so she can prepare for the team meeting.
Reflective time out 10 - stage1: Facts
You meet the team; do you think you could ask for their help to complete Mrs. Henderson's assessment? In what points?
Florence could ask her colleagues help to describe Mrs. Henderson's defensive behaviours. She could complete an instrument centred on the frequency and category of behaviours. For example, the Ryden Aggression Scale could be used. The Cohen-Mansfield Agitation Inventory is often utilized to measure and describe defensive behaviours even if this instrument is made for agitation behaviours and describes several behaviours which are not "aggressive."
Reflective time out 11 - stage 4: Theories
What theoretical elements could help you present Mrs. Henderson's care plan to the nursing staff?
For the nursing team, Florence decides to explain Mrs. Henderson's characteristics as well as the Retrogenesis phenomenon. She uses the two genograms to illustrate her explanations. With Mrs. Henderson's ecomap, she can add several pieces of information on Mrs. Henderson's life and habits, and summarize explanations given by her son Michael and sister Diana. This permits Florence to insist on the fact that defensive behaviours are meaningful and are mainly related to the Retrogenesis experience and to the most important family roles in life, personal values, and accomplishments. After that, Florence can explain some of the interventions to be implemented. She can use the FOC Framework to target the physical, psychosocial, and relational needs. Florence can describe what has been planned with the family. She can recapitulate the principles of the Validation® Approach.
Florence can also explain to the nursing staff that they will receive support to implement Mrs. Henderson's care plan. If there is time, she can explain the six Senses perspective to the team and also tell them that it is relevant to them in terms of care objectives. In Mrs. Henderson's situation, among the six Senses, the security one should be addressed.
Reflective time out 12 - stage 5: Clinical reasoning process
What would be your next step? What can you plan regarding Mrs. Henderson's situation?
Obviously, a long journey is taking shape. Florence knows that each step must be taken in its own time. It is therefore essential to document facts and transmit some directives regarding Mrs. Henderson's care plan. It is also essential to schedule clinical follow-ups for her. Additionally, Florence must consider Mrs. Henderson's family's needs and those of the other residents, as they are part of a system [11]. Finally, collaboration with the nursing care teams in other shifts and with members of the interprofessional team must be given careful consideration.
At the end of her shift, Florence will look at the Defensive Behaviours Practice Process Algorithm (Figure 1) and Form (Appendix 1) and realize how much these two tools have guided her in her clinical approach. She will also become conscious of how important specific knowledge is to support quality nursing practice. She can now communicate to her colleagues a thorough assessment of needs as well as useful explanations and relevant and feasible interventions to be implemented.
Conclusion
This article presents a Situation-Specific Fundamentals of Care Practice Process, which is essential for nurses and nursing students caring for people living with AD who show defensive behaviours. As described in the first part of this article, this Defensive Behaviours Practice Process was built on relevant theoretical propositions as well as empirical data.
The Defensive Behaviours Practice Process is based on the FOC Practice Process, which integrates the FOC Framework. In order to support its concrete application in the care of people living with AD and showing defensive behaviours, a clinical form and a memory aid algorithm have been proposed. These two tools originated from a theoretical proposal illustrated by a mid-paradigmatic illustration (Figure 2 in Part 1 of this article). Through the five steps of this process and considering a relationship-centred perspective of care, Florence is able to begin an assessment of Mrs. Henderson. The process allows her to gather relevant information about Mrs. Henderson's characteristics and needs. With the help of the FOC Framework, the physical, psychological, and relational needs are considered in the context of the care. Additionally, the factors contributing to the expression of defensive behaviours are carefully researched. Because the Defensive Behaviours Practice Process integrates the theories, Florence can find some essential explanations on defensive behaviours, as well as some relationship-centred interventions and clinical tools that are theoretically supported and effective. For example, using the genogram, the Retrogenesis genogram, and the Retrogenesis ecomap is really helpful in formulating a working hypothesis, explaining the situation to family and caregivers, and identifying the elements of intervention.
Moreover, because the Defensive Behaviours Practice Process is rooted in a relationship-centred perspective of care, Florence is keen on developing a relationship with Mrs. Henderson and her family. She also carefully considers the relationship between Mrs. Henderson, other residents, and caregivers.
As explained in Part 1, this article represents a first version of our proposal, and is bound to evolve with new theoretical proposals and developments, as well as the conceptualization work of the authors. We invite readers to visit the International Learning Collaborative website to learn more about Fundamental Care as well as the Fundamentals of Care Framework: https://ilccare.org/
Relevance to Clinical Practice
The Defensive Behaviours Practice Process can be extremely useful not only in improving the quality of nursing care for people showing defensive behaviours but also in guiding the teaching of nurses and nursing students. Indeed, the situations of defensive behaviours shown by people living with AD are extremely complex. These situations require adopting a rigorous clinical process. In this regard, we note that, due to the nature of this article and Ms. Henderson's health condition, the physical examination dimension included in the nursing assessment process was solely addressed from an inspection perspective. An example of a clinical assessment specifically addressing the physical examination of a person showing reactive behaviours has been previously conducted [5].
Regarding the Defensive Behaviours Practice Process, we can state that the situations of defensive behaviours shown by people living with AD also absolutely require referring to several theoretical proposals and explanations. These theoretical references are essential to understanding the characteristics of AD. One of the key explanations is related to the phenomenon of Retrogenesis. Theories also help in understanding the purpose of defensive behaviours and the factors contributing to their expression. Most of the theoretical explanations included in the Defensive Behaviours Practice Process reinforce the relationship-centred perspective of care of the FOC Framework. This relationship perspective guides nurses to consider their own relationship with the person, the family members, the other residents, as well as the nursing team.
Faced with the complexity of the needs of people living with AD who show defensive behaviours and considering the important needs of family members, other residents, and members of the nursing team, nurses and nursing students must be able to carry out a relevant and rigorous clinical approach. The Defensive Behaviours Practice Process supports nurses in their clinical approach and helps them integrate the relationship-centred perspective of care and the specific knowledge about defensive behaviours into their daily practice. Moreover, the Defensive Behaviours Practice Process can be used to provide concrete explanations to family members and nursing staff.
Because the Defensive Behaviours Practice Process is based on theory and empirical data, it will evolve over time. This will support nurses and nursing students in grounding their professional practice in contemporary knowledge, which is of utmost importance.
References
- Feo R, Rasmussen P, Wiechula R, et al. (2017) Developing effective and caring nurse-patient relationships. Nurs Stand 31: 54-63.
- Feo R, Conroy T, Alderman J, et al. (2017) Implementing fundamental care in clinical practice. Nur Stand 31: 52-62.
- Conroy T, Feo R, Alderman J, et al. (2016) Building nursing practice: The fundamentals of care framework. In J Crisp, C Douglas, C Rebeiro, et al. (Eds), Potter and Perry's fundamentals of nursing - Australian version (5th edn). Elsevier, Chatswood, NSW, Australia, P: 15-29.
- Kitson A (2018) The fundamentals of care framework as a point-of-care nursing theory. Nurs Res 67: 99-107.
- Rey S, Voyer P, Bouchard S, et al. (2020) Finding the fundamental needs behind resistance to care: Using the fundamentals of care practice process. Journal of Clinical Nursing 29: 1774-1787.
- Rey S (2018) Facilitate understanding of the "retrograde dive" by using the genogram and the ecomap: Systemic nursing intervention (oral communication). Paper presented at the Assembly of practitioners in psychogeriatrics Conference workshop, Lausanne (CH).
- Rey S (2020) Understanding the defensive behaviours expressed by people with Alzheimer's disease (in French). 7-hour training for caregivers with practical workshop. Humanitae - Residence for seniors with Alzheimer's disease.
- Rey S (2020) Understanding the defensive behaviours expressed by people with Alzheimer's disease (in French). 7-hour training for caregivers with practical workshop. Quebec City Centre of Excellence on Aging.
- Rey S, Gauthier M, Despois L, et al. (2018) Genogram, ecomap and retrograde dive: Represent the person's experience. (Oral communication in French). Paper presented at the 7th World Congress of French-speaking Nurses, Bordeaux (F).
- Rey S, Savoie C (2020) Five fundamental stages to meet the physical, psychosocial and relational needs of the elderly person (in French). 7-hour training for caregivers with practical workshop.
- Kaakinen JR (2018) Family nursing assessment and intervention. In J R Kaakinen, DP Coehlo, R Steele, et al. (Eds), Family health care nursing: Theory, practice, and research (6th edn), FA Davis Company Philadelphia, USA, P: 113-146.
- Shajani Z, Snell D (2019) Wright and Leahey's nurses and families: A guide to family assessment and intervention (7th edn). F A Davis Company, Philadelphia, USA.
Corresponding Author
Dr. Sylvie Rey, Faculty of Nursing Sciences, Laval University, Pavillon Ferdinand-Vandry 1050, Avenue de la Médecine, Quebec City, Canada, Tel: 1418-326-5010, E-mail: sylvie.rey@fsi.ulaval.ca
Copyright
© 2021 Rey S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.