Alternative Back-Up Approach for Inaccessible Laparoscopy in Cases of Huge Probably Benign Cystic Adnexal Masses
Abstract
Objective: To test if minilaparotomy is a suitable alternative to laparoscopy in cases of inaccessible operative laparoscopy for treating cystic huge adnexal masses.
Subjects and methods: It comprised 28 consecutive reproductive non-pregnant women with above umbilicus huge probably benign cystic adnexal masses beyond the capacity of conventional laparoscopic intervention due to failed access of the intraumbilical primary trochar. Preoperative clinical, biochemical, and sonographic assessment of the cystic lesions revealed probability of benign nature of the cysts. Minilaparotomy (ML) followed by cyst aspiration utilizing a 10 mm laparoscopic trocar followed by cyst wall extraction for histopathology and ovarian refashioning. The primary outcome was to evaluate the feasibility, safety, and success of both techniques. The secondary outcomes were correlation of ultrasonographic diagnosis and histopathologic diagnosis and recurrence rate after surgery.
Results: The procedure was successful in 25 patients (89.29%). Ovarian extraction failed in 3 patients (10.71%); an endometrioma with extensive adhesions and two patients of inflammatory masses. The mean operative time was 37 minutes (28-47 min). The mean amount of sucked cyst fluid was 2.9 liters (2.2-5 liters). Postoperative course passed smoothly in all patients that were discharged within 8 hours (range of 6-11 hours). All women were satisfied with this minilaparotomic microsurgical technique apart from 3 patients (10.71%) that who were switched into laparotomy and stayed over a night as a regular care of our institution. This technique missed a case of borderline serous cystadenocarcinoma.
Conclusions: Despite the technical feasibility of minilaparotomy, it is a not a safe alternative to laparoscopy in cases of cystic huge adnexal masses due to inevitable cyst content spillage, failed cyst extraction in some cases and possibility of missing a malignant lesion.
Keywords
Minilaparotomy, Microsurgical, Laparoscopic, Trocar, Adnexal cyst
Introduction
Both female patients and expert surgeons prefer the concept of "perfect operations via small incisions". Practically, many patients with adnexal masses are too young concerned with cosmetic appearance of their abdomen and subsequent fertility. Basically, operative laparoscopy is the ideal approach in the majority of patients. Unfortunately, it may be inaccessible due to lack of sufficient surgeon's experience or proper instrumentation or inappropriate patient. The latter is encountered in some cases with huge adnexal cystic mass. Minilaparotomy (ML) is a 4 cm small cosmetic cut that helps early recovery after surgery (ERAS) with little costs [1]. Many gynecologic procedures can be successfully performed via ML [2-6]. It offers a minimally invasive option for the management of benign adnexal lesions in the pediatric and adolescent age group with comparable recovery to that of laparoscopy [7]. However, in some patients, it seems difficult to perform complete operation via ML particularly if the mass is huge-sized [8]. This study aims to test if ML is a suitable alternative to laparoscopy in cases of inaccessible operative laparoscopy for treating cystic huge adnexal masses.
Patients and Methods
Study design and setting
This is a non-randomized prospective interventional case series without comparison performed at the Woman's Health University, Assiut, Egypt between September 2019 and April 2020. The institutional review board (IRB) approved the study on August 2019.
Subject selection
A total of 28 consecutive reproductive non-pregnant women with above umbilicus huge probably benign cystic adnexal masses attending gynecologic and infertility clinics were enrolled in this study.
Inclusion and exclusion criteria
It included women aged ≥ 18-40 years with huge above the umbilicus probably benign adnexal cystic masses as Clinically, sonographically and biochemically diagnosed. All women were surgically fit without any medical risk. Exclusion criteria were below umbilicus adnexal cystic masses (usually accessed via laparoscopy at our institution), clinical, biochemical or sonographic suspicion of malignancy or unfit patients due to a well-documented medical or surgical risk. However, some women with raised Ca-125 (and negative other tumor markers) were included in the study whenever TAS and TVS showed a diagnosis of ovarian endometrioma. Women with a history of any type of previous abdominal surgery were excluded for fear of adhesions and scarring. There was no exclusion based on a specified BMI as the used retractors are of long blades.
Preoperative evaluation
Combined high resolution 2D transabdominal (TAS) and transvaginal (TVS) ultrasonography were performed for all women to determine the size, site, and number of masses. Cyst wall thickness, echogenicity of fluid inside, presence and thickness of septa, and any evidence of ascites were recorded. Sonographic exclusion criteria included the presence of ascites, metastases or intracystic solid nodules ≥ 1 cm. Blood samples were taken from all patients for surgical fitness and for tumor marker estimation. CA-125 ≤ 35 U/ml, carcinoembryonic antigen (CEA) ≤ 5 ng/ml and α- fetoprotein ≤ 8.5 ng/ml were considered normal. MRI was requested for all patients to confirm the diagnosis, define the borders of the ovaries, and detect any LN or others lesions as recommended [9].
Operative interventions
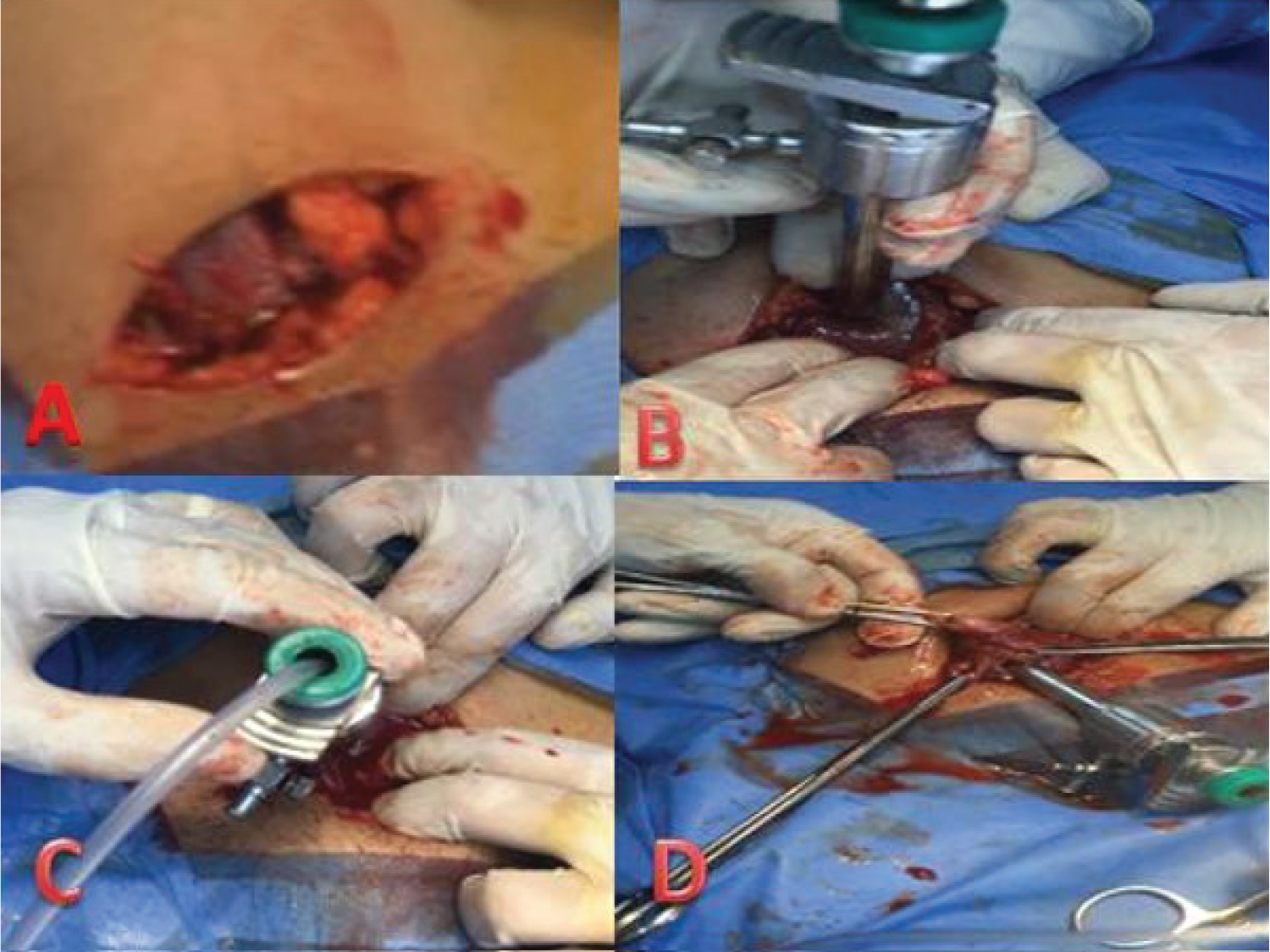
After patient preparation as usual for open surgery, a 4 cm length ML transverse incision crosswise suprapubically about 2-3 cm over the upper edge of the pubic symphysis was made (Figure 1A). Both the fascia and the parietal peritoneum were cut transversely while the rectus muscles were spread laterally. Keys of success of ML included exaggerated lateral incision of subcutaneous fat more than the skin incision, upward dissection of the rectus sheath as high as possible and the use of long-bladed thin retractors.
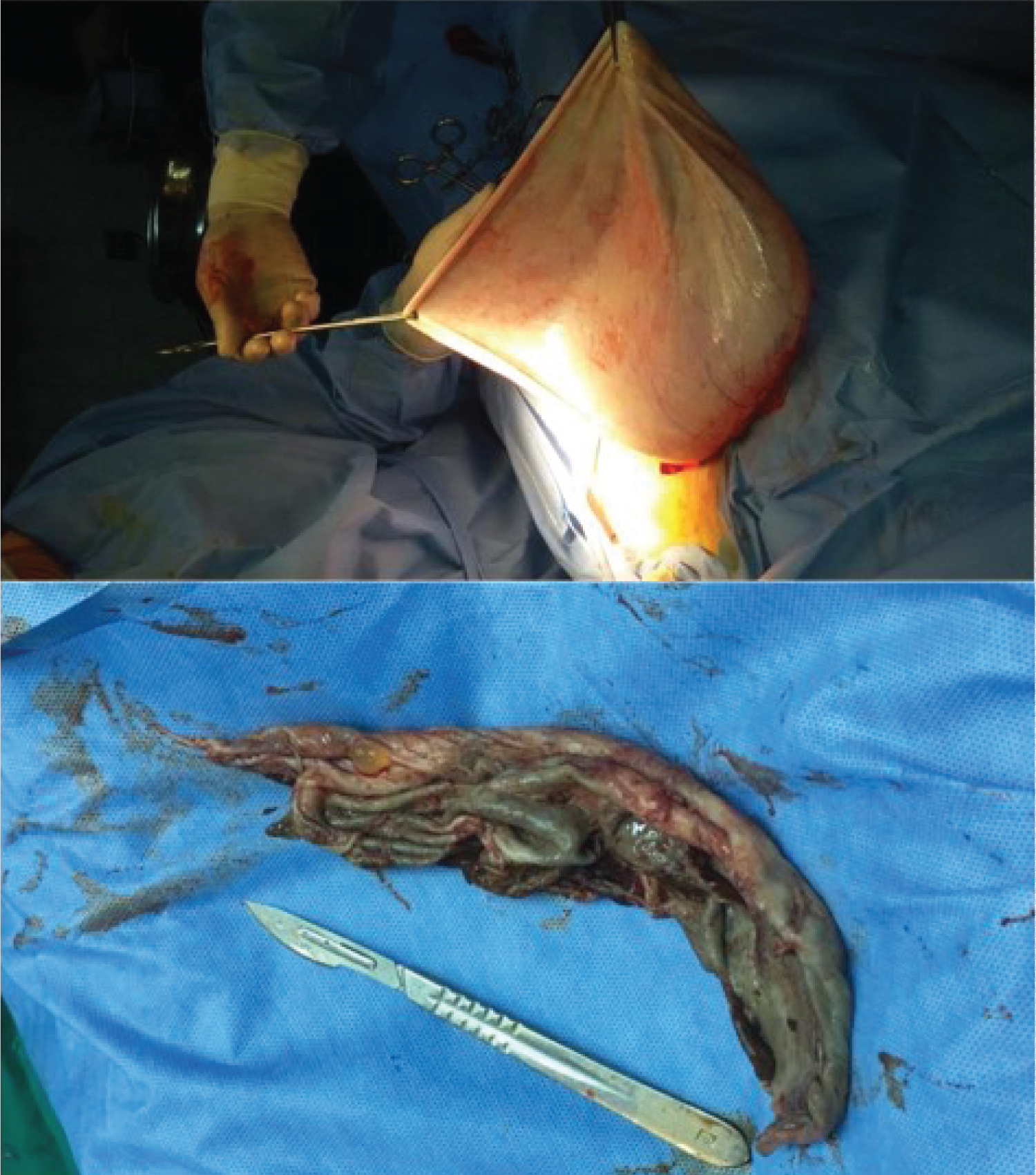
On entrance of the peritoneal cavity, the huge adnexal cyst was pushed towards the incision by the two hands of the assistant to be fitted to the incision and avoid wrong trocar penetration. A 10 mm reusable laproscopic trocar with pyramical tip was pushed perpendicularly on the cyst and penetrated it using screwing movement of the wrist (Figure 1B). Once the cyst was penetrated, the sleeve was left, and a sterile suction tube was loaded inside it to start gradual tight drainage into a central suction unit to avoid sudden decompression of the huge mass (Figure 1C). The color and amount of the fluid were reported. After cyst collapse, its walls were extracted using three Allis forceps applied fitted alongside the sleeve to avoid spillage of the cyst contents into the peritoneal cavity (Figure 1D). After complete extraction of the whole adnexa (Figure 2), with the aid of long-bladed retractors the peritoneal cavity was explored for any evidence of additional masses or paraortic lymph nodes. The upper abdomen could not be reached due to the small incision. Evaluation of the upper abdomen relied on the preoperative high resolution 2D TAS and sometimes MRI. Thereafter, sterile towels were fitted into the incision to avoid peritoneal soiling during cyst extraction. Proper naked eye assessment of the interior of the cyst to rule-out gross appearance of ovarian malignancy like ovarioscopic examination of the adnexal cysts as described by our team before [10]. If the patient was young and desired further fertility, adnexal cystectomy with closure of the bed was done. The 10 mm cyst hole of the ovary was extended followed by cyst wall peeling off with coagulation of the bed utilizing bipolar electrocoagulation. Finally, the bed is sutured with fine Vicryl sutures, and the epithelial incision was sutured in a microsurgical manner with fine in-out continuous suturing for ovarian refashioning. After reinsertion of the ovary into the peritoneal cavity, peritoneal toilet was performed followed by irrigating with 500 cc lactated Ringer solution and insertion of a tube drain. The extracted cyst wall was sent for histopathological examination. Frozen section is not available at our institution. If she completed her family, oophorectomy was done and the whole ovary was sent for histopathologic evaluation. The parietal peritoneum was not sutured while continuous sutures were adopted for the fascia and subcuticular skin using 0 rapid Vicryl stitches. One patient of borderline serous cystadenocarcinoma was a multiparous and was counseled for total abdominal hysterectomy and bilateral salpingoophorectomy 2 weeks after ML.
Follow up
Patients were discharged whenever stabilized on prophylactic BS antibiotics. They were advised to come back for follow-up after two and four weeks for clinical and sonographic evaluation and definition of further plan of management according to histopathology The patient of borderline serous cystadenocarcinoma was followed up for 6 months with frequent clinical, sonographic and MRI monitoring. Finally, patients' satisfaction with the procedure was reported.
Outcome measures
The primary endpoint of the study was to evaluate the feasibility, safety and success of laparoscopically oriented ML while secondary endpoints were recurrence and correlation of ultrasonographic diagnosis and histopathologic diagnosis.
Data collection and statistical analysis
Data were tested for normality using the Anderson-Darling test and for homogeneity variances prior to further statistical analysis. Statistical analysis was performed with the IBM SPSS 20.0 software (SPSS, Inc., Chicago, IL). Data were presented using descriptive statistics in the form of frequencies and percentages for qualitative variables, and ranges, means and SDs, medians and quartiles for quantitative variables in box plots. . A p-value ≤ 0.05 was assumed significant in all tests conducted.
Results
This study comprised 28 consecutive patients presented with above umbilicus huge probably benign cystic adnexal masses. Their sociodemographic data, complaints and tranabdominal and transvaginal ultrasonographic findings are demonstrated in Table 1. The procedure was successful in 25 patients (89.29%). Ovarian extraction after cyst aspiration failed in 3 patients (10.71%); one patient with endometrioma and two patients with inflammatory masses that required widening of the wound to achieve proper dissection of the mass from dense intestinal adhesions and drainage of pockets of pus. The mean operative time was 37 minutes (28 min-47 min). Unintentional peritoneal soiling was encountered in 5 cases (17.8%). The mean amount of sucked cyst fluid was 2.9 liters (2.2-5 liters). In all cases copious peritoneal lavage using isotonic saline was made. Postoperative course passed smoothly in all patients that were discharged within eight hours (range of 6-11 hours) except 3 patients who were switched to laparotomy and stayed in the hospital over a night. Histopathologic diagnosis was consistent with TAS and TVS in 24 patients (85.7%). Histopathology revealed adnexal inflammatory cystic lesions including abscess in three patients and one patient of borderline serous cystadenocarcinoma. Postoperatively, the latter was followed up clinically, biochemically and by MRI which revealed normal anatomy up to 6 months postoperatively. All women were satisfied with this new technique apart from 3 patients (10.71%) that were switched into laparotomy and stayed over a night as a regular care of our institution.
Discussion
Above umbilicus huge adnexal cysts represent a real management challenge whether laparoscopic or laparotomic [11]. Since most patients present with history of progressive abdominal distention (in this study it was diagnosed in 10 patients (35.7%)), early diagnosis and proper management of adnexal masses is very crucial. Follow-up of simple cysts of small size (less than 5 cm) with some treatment resulted in complete disappearance within 8 weeks in 19.4% of patients [12].
The vast majority of large adnexal masses ≤ 10 cm in size can be safely excised via laparoscopy with the following precautions: An experienced laparoscopic surgeon, immediate access to frozen section diagnosis, and preparation of patient to receive an adequate cancer surgery where indicated [13]. These conditions are not always available in all hospitals. Moreover, in this study, laparoscopic approach was not feasible as all patients had cystic lesions above the umbilicus where laparoscopic entry obligatory will lead to peritoneal soiling by above umbilicus cyst contents due to inevitable cyst puncture during entry. A case report used Hasson open laparoscopy technique for laparoscopic excision of huge above umbilicus ovarian cyst due to inaccessible regular entry technique [14]. If compared to laparoscopy, ML requires less learning curve without sophisticated laparoscopic procedures like suturing and endobag use with lower risk of complications. In a study comparing mini laparotomy (< 4 cm vertical or transverse abdominal incision) versus laparoscopy for treatment of benign gynecologic conditions [15], ML was proved to be a safe alternative to traditional minimally invasive approaches in gynecology and offered the additional benefits of shorter intraoperative time and less blood loss despite a significantly higher rate of major wound complications. They concluded that ML is an important surgical approach and should be included in gynecologic surgical training, ML is easy to learn and can be performed utilizing regular surgical instruments by general gynecologists in a shorter operating time. In this study, we selected transverse ML as all patients preferred it over vertical incision from cosmetic point of view.
One of the main problems of huge adnexal cysts is potential peritoneal dissemination of carcinoma or gelatinous material caused by unintentional rupture which was encounterd in 3 cases in this study. However, this risk was minimal as proved by postoperative histopathologic assuring results except one patient proved to be borderline cystadenocarcinoma after complete excision of the cyst wall via ML. This case is considered the main disadvantage of this technique as missing one case of borderline malignancy is serious and deserves reassessment of the procedure. Gynecologists shouldn't ignore clinical, ultrasonographic, biochemical and possible MRI evaluation of patients [9]. Imaging is paramount for planning management of giant ovarian cysts as imaging identifies any suspicious features of malignancy e.g., multiple partitions, and endo- or exocystic vegetations [16]. Moreover, meticulous intraoperative naked-eye assessment of the ovary and the ipsilateral ovary are good assuring steps. Despite not available at our institution, frozen section has a risk of misdiagnosing malignancy and under-staging women [17].
Devices used for simultaneous cyst penetration and concomitant aspiration are many like disposable Topel Endoscopic Cyst Aspirator Set which is disposable and not available in many OR in addition of being principally designed for laparoscopic surgeries. Others can simply place a purse string suture in the cyst wall, create a hole and drain via a Poole aspirator but huge cyst is usually tense and stiches in its wall will eventually lead to fluid leakage. In a study on ML for huge ovarian cysts, a surgical adhesive, glued a large plastic wound dressing to the surface of the cyst was put to prevent leakage of contents into the abdominal cavity [18]. Their technique is costly and not available in many OR while our technique is easier and costless. Moreover, they used a Verres needle for cyst aspiration which is time consuming to drain a huge cyst while this technique used a 10 mm trocar for rapid and tight drainage. In another study [19], 6 liters of cystic fluid were drained via creation of a non-tight small hole in a huge cyst that was proved to be serous cystadenoma. The authors were obliged to do hysterectomy and bilateral salpingoophorectomy three-month latter for fear of recurrence. Technical tricks used in this study guarded against unintentional peritoneal soiling by cyst contents as cyst wall hole was 10 mm regular and aspiration was controlled by insertion of the aspiration catheter via the well fitted sleeve. Moreover, counter traction on the edges of the hole with Allis forceps associated with gradual extra-abdominal extraction of the decompressing cyst eventually prevented peritoneal soiling by cyst contents. The current study describes an innovative minilaparotomy technique for the removal of benign ovarian cysts and offers the advantages of laparoscopic and laparoscopic-assisted procedures while omitting the major disadvantage such as lengthy operative time, and long learning curves. This approach is valuable in low health care setting to bypass the necessity for specialized and expensive equipment while providing surgical management and cosmetic benefit in the management of large adnexal mass.
However, this study has its limitations being non-randomized, non-comparative and of small sample size which can be explained by rarity of patients of huge probably benign above umbilicus adnexal cystic lesions. Short follow-up period for most patients. Unintentional peritoneal soiling and inability to meticulously examine the upper abdomen and lack of intraoperative frozen section are practical disadvantages of this study.
Conclusions
For this study, it is concluded that despite the technical feasibility of minilaparotomy using a 10 mm laparoscopic trocar, it is a not a safe alternative to laparoscopy in cases of cystic huge adnexal masses due to inevitable cyst content spillage, failed cyst extraction in some cases and possibility of missing a malignant lesion.
Disclosure of Potential Conflicts of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contribution
The authors confirm contribution to the paper as follows: study conception and design, operative procedures, and manuscript writing: Atef Darwish; data collection: Dina Darwish; analysis and interpretation of results: Atef Darwish.; draft manuscript preparation and reference check Ahmed Dervis. All authors reviewed the results and approved the final version of the manuscript.
References
- Ljungqvist O, Scott M, Fearon KC (2017) Enhanced recovery after surgery: A review. JAMA Surg 152: 292-298.
- Barone MA, Mbuguni Z, Achola JO, et al. (2017) Safety of tubal ligation by 4 cm minilaparotomy provided by clinical officers versus assistant medical officers: Study protocol for a non-inferiority randomized controlled trial in Tanzanian women. Trials 18: 499.
- Antell K, Deshmukh P, Brown EJ (2017) Contraception Update: Sterilization. FP Essent 462: 30-34.
- Glasser MH (2005) 4 cm minilaparotomy myomectomy: A minimally invasive alternative for the large fibroid uterus. J Minim Invasive Gynecol 12: 275-283.
- Ksiezakowska-Lakoma K, Zyla M, Wilczynski J (2015) Removal of uterine fibroids by mini-laparotomy technique in women who wish to preserve their uterus and fertility. Wideochir Inne Tech Maloinwazyjne 10: 561-566.
- Beriashvili Z, Gurgenidze M, Zurashvili M (2007) Advantages of 4 cm minilaparotomy approach in treatment of acute destructive cholecystitis. Georgian Med News 153: 7-10.
- Trotman G, Foley C, Taylor J, et al. (2017) Postoperative outcomes among pediatri and adolescent patient undergoing 4 cm minilaparotomy vs laparoscopy in the management of adnexal lesions. J Pediatr Adolesc Gynecol 30: 632-635.
- Bolla D, Deseö N, Sturm A, et al. (2012) 4 cm minilaparotomy a good option in specific patients: A patient report of bilateral ovarian germ cell tumor. Case Rep Obstet Gynecol 589568.
- Karnik A, Tembey RA, Mani S (2015) Value of MRI in characterizing adnexal masses. J Obstet Gynaecol India 65: 259-266.
- Darwish AM, Amin AF, El Feky MA (2000) Ovarioscopy, a technique to determine the nature of cystic ovarian tumors. J Am Assoc Gynecol Laparosc 7: 539-544.
- Elhassan SA, Shabina Khan S, El Makki A (2015) Giant Ovarian Cyst masquerading as Massive Ascites in 11-Year-Old. Patient Rep Pediatr 2015: 878716.
- Darwish AM, Amin AF, Abdel-Aleem MA, et al. (2001) Laparoscopic management of benign adnexal masses: Experience in a developing country Gynaecological Endoscopy 10: 159-165.
- Ghezzi F, Cromi A, Bergamini V, et al. (2008) Should adnexal mass size influence surgical approach? A series of 186 laparoscopically managed large adnexal masses. BJOG 8: 1020-1027.
- Baradwan S, Sendy F, Sendy S (2017) Complete laparoscopic extirpation of a giant ovarian cyst in an adolescent. Case Rep Obstet Gynecol 2017: 7632989.
- Kumar A, Pearl M (2014) Mini-laparotomy versus laparoscopy for gynecologic conditions. J Minim Invasive Gynecol 21: 109-114.
- Diop B, Niang MM, Ba PA, et al. (2016) Management of giant ovarian cysts: A review of 5 patient reports. J Gynecol Surg 32: 162-166.
- Ratnavelu ND, Brown AP, Mallett S, et al. (2016) Intraoperative frozen section analysis for the diagnosis of early stage ovarian cancer in suspicious pelvic masses. Cochrane Database Syst Rev 3: CD010360.
- Pelosi III M, Pelosi III M (2004) A novel 4 cm minilaparotomy approach for large ovarian cysts. Obg Management 17-30.
- Moslemi MK, Yazdani Z (2010) A huge ovarian cyst in a middle aged iranian female. Patient Rep Oncol 3: 165-170.
Corresponding Author
Darwish AM, MD, PhD, Department of Obstetrics & Gynecology, Woman's Health University Hospital, 71111 Assiut PO Box, Egypt, Fax: 020-882-368-377.
Copyright
© 2022 Darwish AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.