First Documented Case of Massive Pulmonary Embolism and Massive Ilio-Femoral Deep Venous Thrombosis Treated Simultaneously
Abstract
Deep Venous Thrombosis (DVT) and Pulmonary Embolism (PE) cause major morbidity and mortality. A PE develops from a DVT. Surprisingly there are very few reports of a DVT and a PE being documented together, and there are no reports of a simultaneous treatment of both by a CDT. We report such a case where a patient presented to us with proximalilio-femoral DVT and massive PE. She successfully underwent an emergency simultaneous CDT of both pathologies.
Keywords
Pulmonary embolism, Deep venous thrombosis
Introduction
Venous thromboembolism (VTE) is a spectrum of disease including deep vein thrombosis (DVT) and pulmonary embolism (PE) [1,2]. VTE is a major public health concern, estimated to effect 1 to 2 per 1,000 people in the US each year [1]. PE is responsible for almost all VTE related deaths. Over 80% of PE are the result of DVT in the leg or pelvic veins. These clots dislodge and travel through the venous system to the heart and into the pulmonary arteries. Estimates suggest that at least 100,000 Americans die of VTE each year, with 10-30% of patients dying within 30 days of diagnosis, and 20-25% of PE cases presenting as sudden death [1,2]. Pulmonary embolism (PE) is the third most common cause of cardiovascular death in the United States of America [1,2]. Many patients die within the first few hours of presentation, making an early diagnosis and treatment paramount to survival. Pulmonary embolisms are categorized into three main risk categories: Low risk, intermediate (sub-massive), and high risk (massive). Submassive PEs are further sub-divided into intermediate-high and intermediate-low risk PEs [1,2]. We present a case of massive proximal DVT and massive PE both treated simultaneously.
Case Report
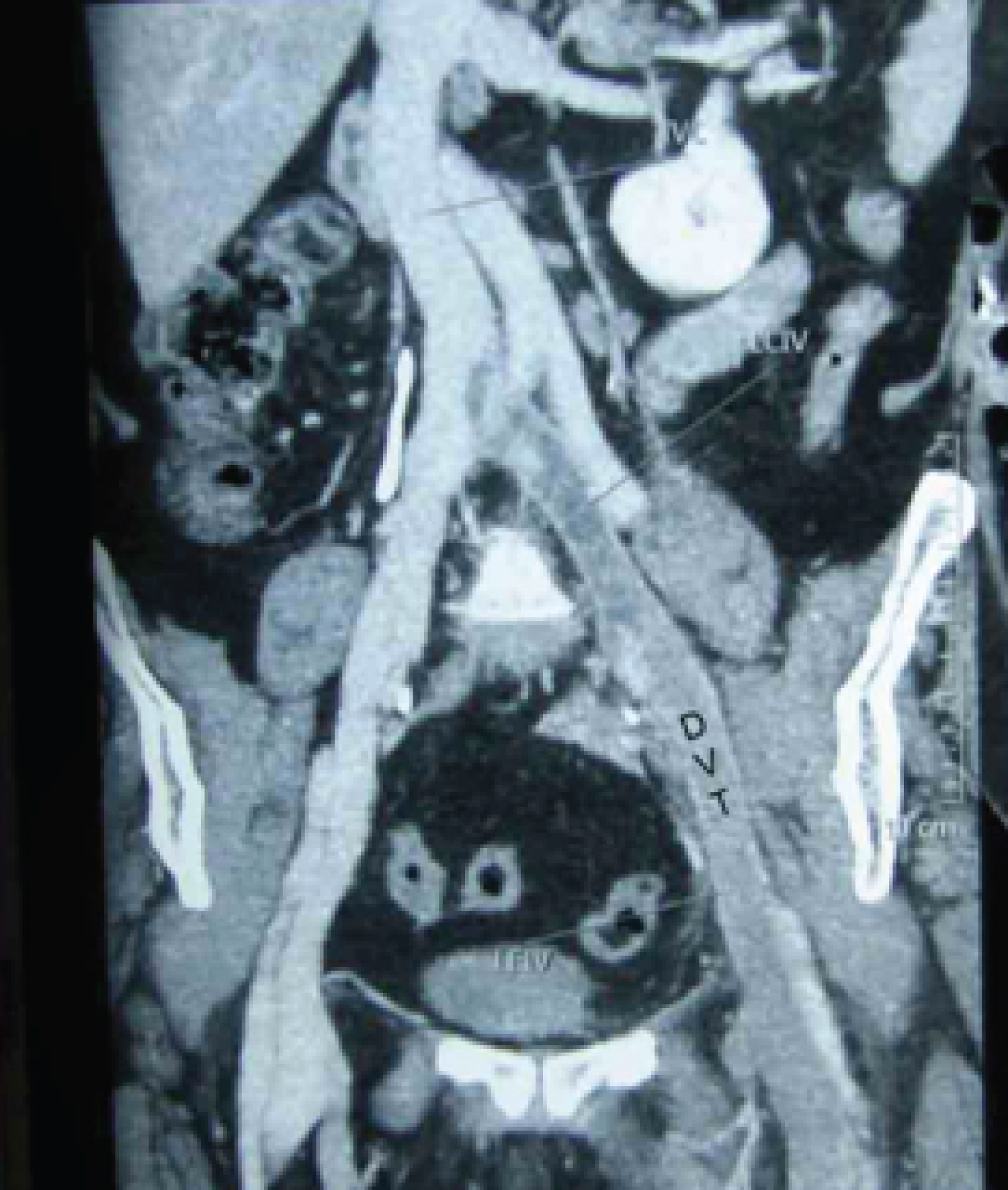
A 46-year-old female presented to an outside hospital with acute left leg swelling. She was an operated case of cancer breast presently on Tamoxifen. On examination and on investigation with Duplex and CT venography she was found to have left sided DVT extending up to the iliac vein-the IVC was free (Figure 1). She was started on low molecular weight heparin (LMWH) and Rivaroxaban. Within 3 hours of diagnosis and start of therapy - she developed dyspnea and collapsed. She was successfully resuscitated. A CT pulmonary angiogram revealed a massive main pulmonary artery (MPA) PE (Figure 2). She was referred to our centre on moderate inotropes. On assessment at admission she was noted to be hypotensive (BP < 90 mmHg on adequate inotropes) and had ECG and echo findings of RV strain. Her Trop I and BnP levels were raised.
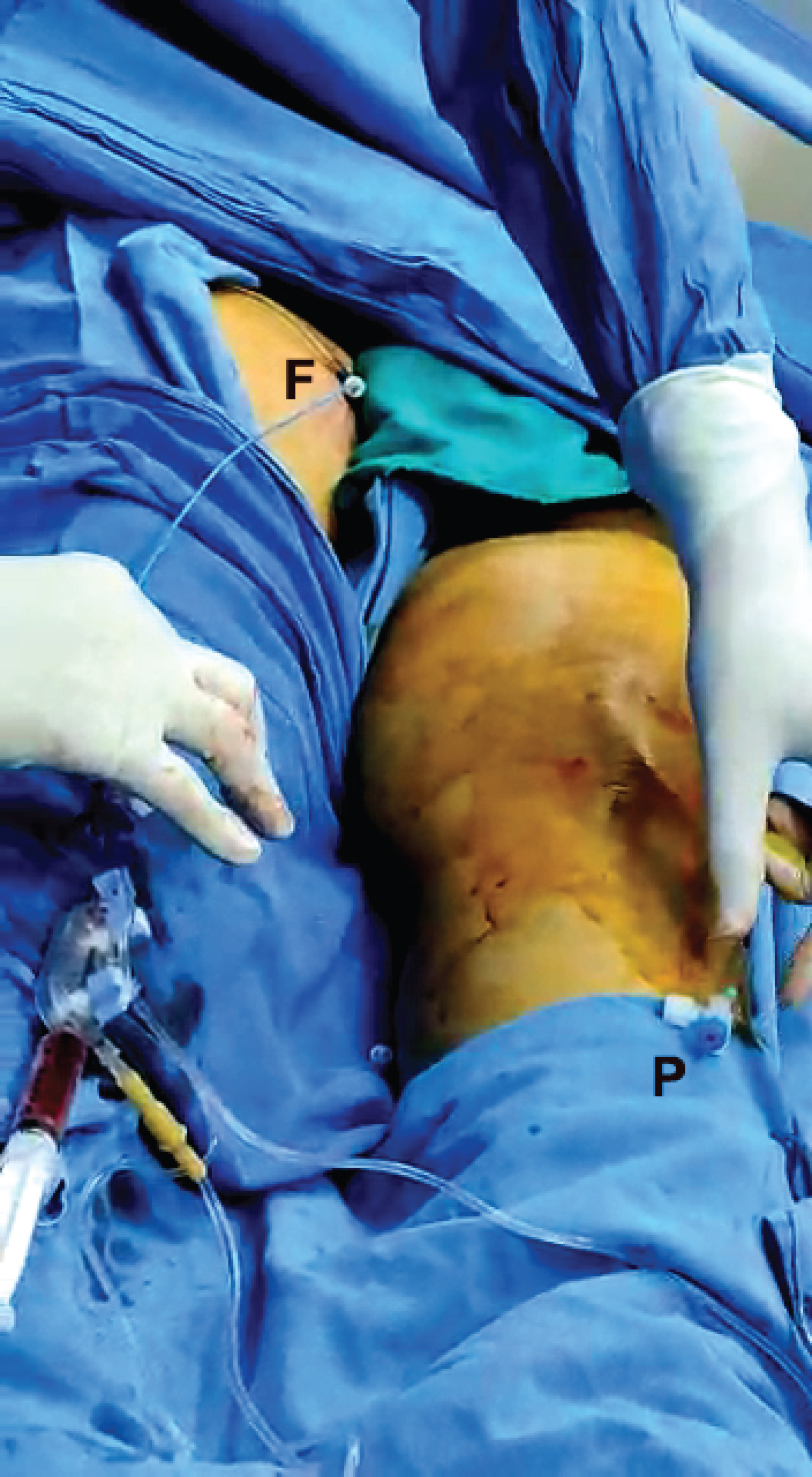
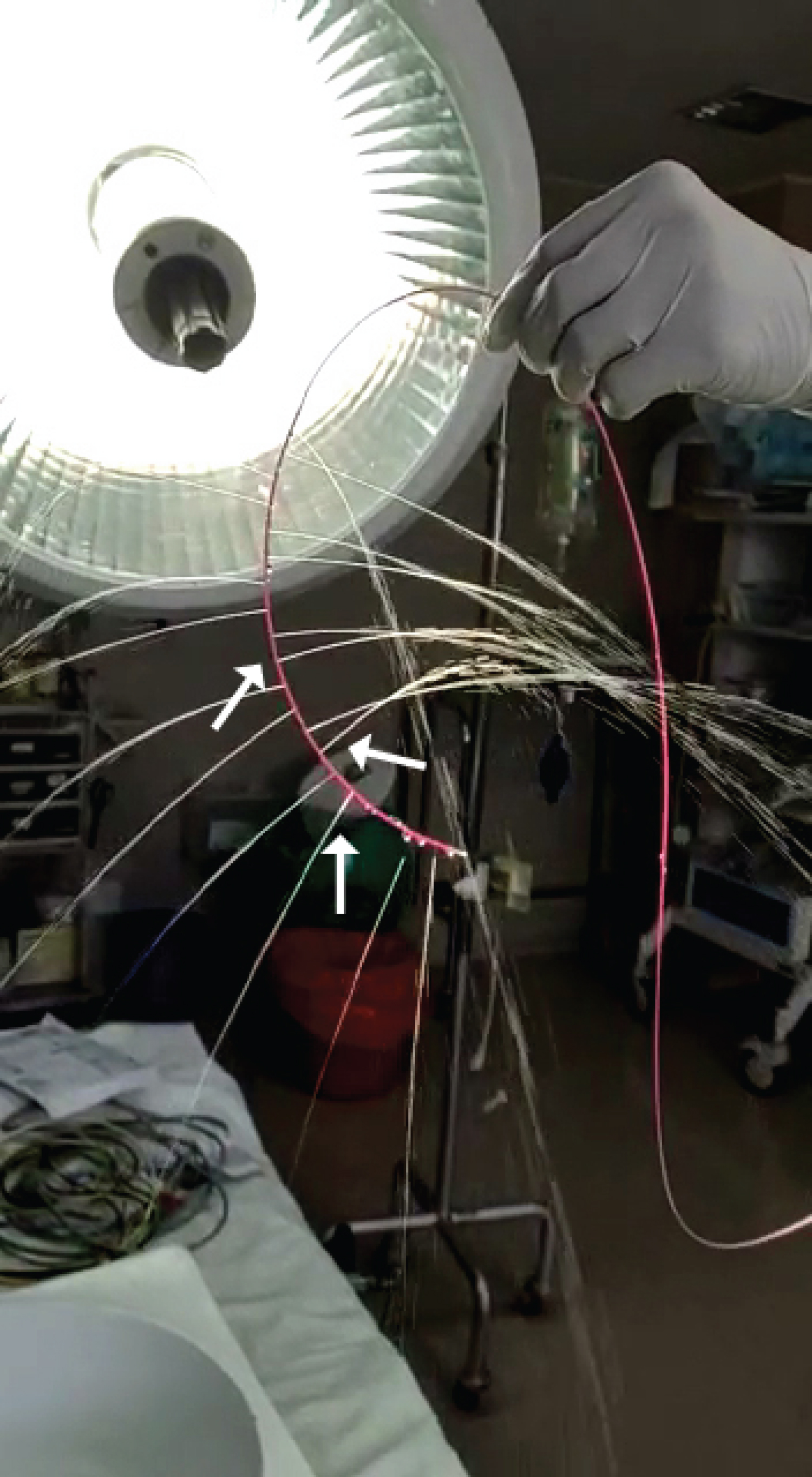
She underwent an emergency catheter directed thrombolysis (CDT) through a sheath and catheter via the left popliteal vein and a CDT of the PE via a catheter from the right femoral vein (Figure 3). Recombinant Tissue Plasminogen Activator-Reteplase (Abbott) was used. A spray bolus of 3 mg each was given at both sites followed by 1 mg/hour over 24 hours by an infusion pump. Unfractionated heparin was given in both sheaths at 500 units/hour. An IVC filter was thought of but not deployed in view of an already present PE and plan to treat by CDT. Her PA pressure was ¾ systemic. A pig tail catheter was used to fragment the clot in the MPA and tPA started by a multihole Cragg-McNamara catheter (Figure 4). The iliac vein clot was also fragmented and tPA started via a separate Cragg McNamara catheter. In between aspiration of clots was also done from both sides (Figure 5).
Results
The clinical condition of the patient improved rapidly, and the PA pressure fell initially to ½ and by next day to 1/3 systemic. A check venogram revealed a complete resolution of the clot in the lower limb with no iliac vein stenosis. A PA angiogram showed a major reduction in the clot load with a good flow in both pulmonary arteries. The patient was discharged on long term Rivoraxaban and is on follow up for a year now with 6 monthly Duplex scans. She is asymptomatic.
Discussion
The American Heart Association and the European Society of Cardiology stratify pulmonary embolism into three risk categories: High risk or massive, intermediate risk or submassive, and low risk [2,3]. High-risk pulmonary embolism is defined as acute pulmonary embolism with sustained hypotension, a requirement for vasoactive drugs, or need for cardiopulmonary resuscitation [2,3]. For patients with acute pulmonary embolism who are initially hemodynamically stable, the in-hospital mortality rate is 3.4%, compared with 31.8% for patients who are hemodynamically unstable at presentation [4]. For the latter group, the all-cause mortality rate increases to 58.3% at 90 days [4,5]. Catheter-directed thrombolysis (CDT) is one of the relatively new treatment options for massive and submassive pulmonary embolisms with hemodynamic instability [6-8]. CDT involves the infusion of a thrombolytic agent directly into the clot burden through a percutaneous transcatheter. Multiple studies have demonstrated that CDT is effective at restoring venous patency and reducing symptoms in the setting of acute DVT [9]. The CaVENT trial [9] and to some extent the ATTRACT trial [10] have documented the efficacy of CDT specifically for acute iliofemoral DVT. The American Heart Association (AHA) recommends CDT for first-line treatment of carefully selected patients with acute ilio-femoral DVT (< 21 days within onset of symptoms), limb-threatening compromise, and/or rapid thrombus extension or symptomatic progression despite anticoagulation [2]. The Society of Interventional Radiology (SIR) also has similar recommendations [11]. Currently, CDT is a class 2C recommendation by the American College of Chest Physicians for the management of acute PE associated with hypotension and who have contraindications to thrombolysis, failed thrombolysis, or shock that is likely to cause death before systemic thrombolysis can take effect (eg, within hours), and if appropriate expertise and resources are available [8,12]. This includes massive and intermediate-high submassive risk groups.
So CDT is a recommended for selected cases of DVT and PE. There are not many cases of documented DVT and PE detected concurrently, probably because the DVT clot has already embolsied and is no longer visible on imaging. Surprisingly there is no case reported of a simultaneous CDT of a DVT and a PE in the same patient.
Conclusion
We present a first documented case of successful simultaneous CDT of a massive PE and a massive ilio-femoral proximal DVT with 1 year follow up.
Authors Declaration
The authors declare no conflict of interest.
The patient's consent has been taken for publication of the details of the case.
The paper is not under consideration by any other journal.
References
- Fleck D, Albadawi H, Shamoun F, et al. (2017) Catheter-directed thrombolysis of deep vein thrombosis: Literature review and practice considerations. Cardiovasc Diagn Ther 7: S228-S237.
- Jaff MR, McMurtry MS, Archer SL, et al. (2011) Management of massive and submassive pulmonary embolism, iliofemoral deep vein thrombosis, and chronic thromboembolism pulmonary hypertension: A scientific statement from the American heart association. Circulation 123: 1788-1830.
- Torbicki A, Perrier A, Konstantinides S, et al. (2008) Guidelines on the diagnosis and management of acute pulmonary embolism: The task force for the diagnosis and management of acutepulmonary embolism of the European Society of Cardiology (ESC). Eur Heart J 29: 2276-2315.
- Casazza F, Becattini C, Bongarzoni A, et al. (2012) Clinical features and short term outcomes of patients with acute pulmonary embolism: The Italian Pulmonary Embolism Registry (IPER). Thromb Res 130: 847-852.
- Goldhaber SZ, Visani L, De Rosa M (1999) Acute pulmonary embolism: Clinical outcomes in the international cooperative pulmonary embolism registry (ICOPER). Lancet 353: 1386-1389.
- Kearon C, Akl EA, Ornelas J, et al. (2016) Antithrombotic therapy for VTE disease: CHEST guideline and expert panel report. Chest 149: 315-352.
- Kuo WT, Gould MK, Louie JD, et al. (2009) Catheter-directed therapy for the treatment of massive pulmonary embolism: Systematic review and meta-analysis of modern techniques. J Vasc Interv Radiol 20: 1431-1440.
- Furfaro D, Stephens RS, Streiff MB, et al. (2018) Catheter-directed thrombolysis for intermediate-risk pulmonary embolism. Ann Am Thorac Soc 15: 134-144.
- Enden T, Haig Y, Klow NE, et al. (2012) Long-term outcome after additional catheter-directed thrombolysis versus standard treatment for acute iliofemoral deep vein thrombosis (the CaVenT study study): A randomised controlled trial. Lancet 379: 31-38.
- Comerota AL, Kearon C, Gu CS, et al. (2019) Endovascular thrombus removal for acute iliofemoral deep vein thrombosis analysis from a stratified multicenter randomized trial. Circulation 139: 1162-1173.
- Watson L, Broderick C, Armon MP (2014) Thrombolysis for acute deep vein thrombosis. Cochrane Database Syst Rev 11: CD002783.
- MA de Winter, Vlachojannis GJ, Ruigrok D, et al. (2019) Rationale for catheter-based therapies in acute pulmonary embolism. Eur Heart J Suppl 21: I16-I22.
Corresponding Author
Harinder Singh Bedi MCh, FIACS, Department of Cardio Vascular Endovascular & Thoracic Sciences, Ivy Hospital, Sector 71, Mohali, Punjab, India, Tel: 981-406-0480
Copyright
© 2023 Bedi HS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.