Intravascular Leiomyomatosis with Extension to Right Atrium: A Case Report
Abstract
Intravascular leiomyomatosis is an infrequent benign neoplastic disorder characterized by the proliferation of smooth muscle cells within the venous system, often extending from the iliac or gonadal veins into the inferior vena cava. In rare instances, it may infiltrate cardiac cavities or pulmonary vasculature, manifesting as intracardiac leiomyomatosis.
This condition typically affects premenopausal women in their fifth decade, with the majority having a history of hysterectomy and being characterized by symptoms of right heart failure. Imaging techniques such as echocardiography, computed tomography, and magnetic resonance imaging are used to establish the diagnosis, with confirmation through histopathology. Due to its tendency to spread to the heart and progress to heart failure, intracardiac leiomyomatosis can lead to sudden death due to blood flow obstruction.
This case report presents a 45-year-old Latin woman with a history of uterine myomatosis. The diagnosis was established through imaging modalities such as echocardiography, computed tomography and histopathological verification. The case underscores the importance of comprehensive imaging assessment and histopathological confirmation in guiding therapeutic decisions and optimizing patient outcomes.
Keywords
Case Report, Intravascular leiomyoma, Cardiac tumor, Perimenopause, Imaging
Introduction
While leiomyoma is the most common benign neoplastic condition in premenopausal women, intravascular leiomyomatosis is considered an infrequent pathology [1], with intracardiac involvement observed in 10 to 40 percent of studied cases [2]. Despite its benign nature, it shows a high rate of recurrence and metastasis, frequently leading to heart failure and sudden death [3].
Here, we present the case of a 45-year-old woman, previously asymptomatic, with a history of type 2 diabetes, and uterine myomatosis. We outline our approach to diagnosis through imaging and histopathologic methods, treatment, and outcomes.
Case Report
Our patient was a 45-year-old female who reported dyspnea associated with long COVID. She had a history of type 2 diabetes mellitus for 10 years. Additionally, she was diagnosed with uterine myomatosis in 2020 and had undergone one cesarean section and two abortions. Her family history included breast cancer in her mother.
She presented to the Emergency Department after experiencing syncope accompanied by loss of consciousness, facial contusion, and subsequent epistaxis. She reported dizziness and blurred vision preceding the event. Upon admission to the hospital, a protocol for a nasal surgical intervention was initiated due to a Lefort I fracture. On July 12, 2023, she suffered a new episode of dizziness, nausea, syncope, tonic-clonic movements, and diabetic ketoacidosis type hyperglycemia crisis, along with mixed shock, necessitating advanced airway management. She was evaluated by the intensive care department, where a thrombus in transit was identified via echocardiography. As a result, the decision was made to transfer her to a higher level of care.
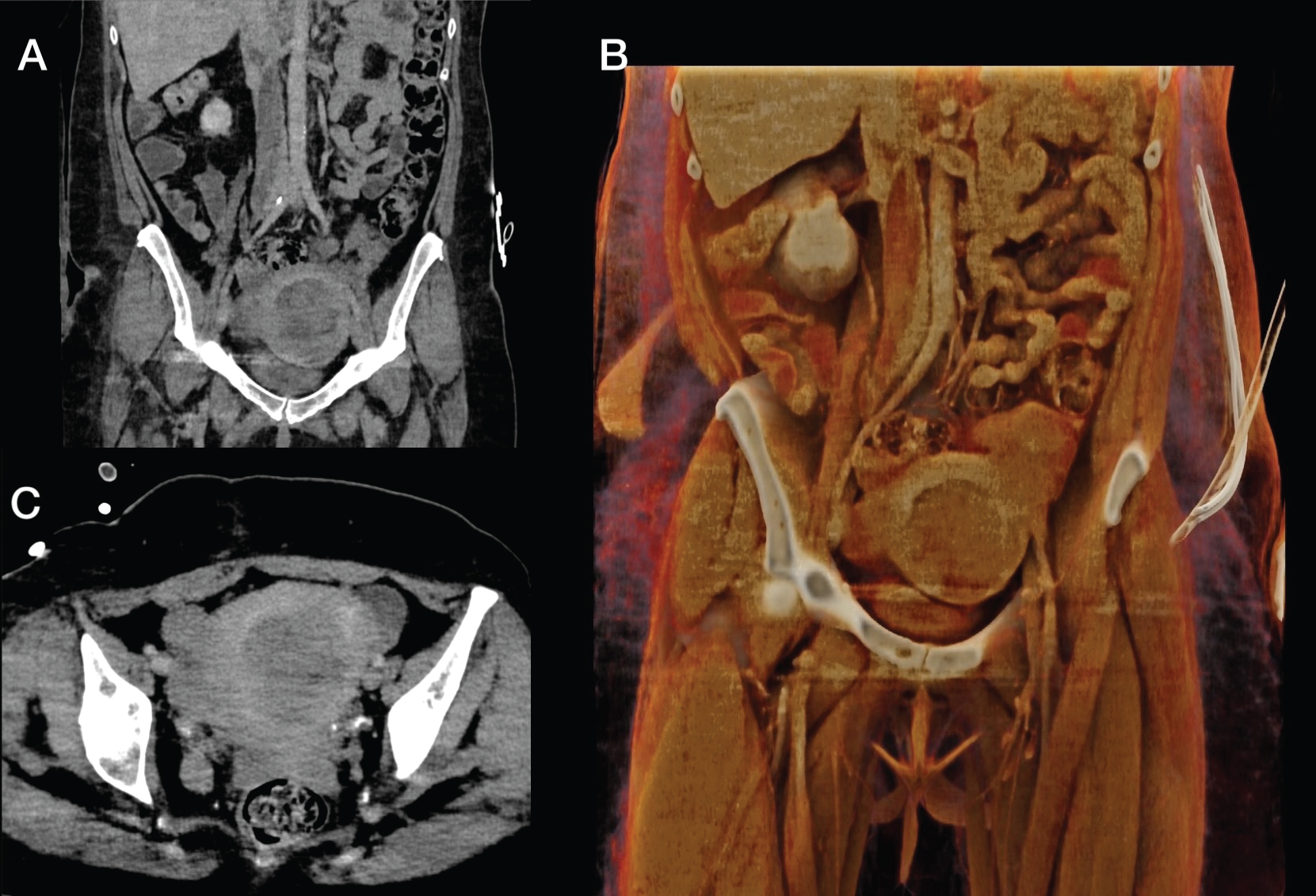
Upon admission to our institution on July 13, 2023, with a diagnosis of intracardiac thrombosis, a computed tomography (CT) scan was performed. The scan revealed a significant thrombotic burden extending from the right atrium to the inferior vena cava, further extending to the right iliac region and pelvic region. Additionally, a uterine lesion suggestive of myomatosis was identified.
• Skull CT scan: No lesions were identified at the skull base or parenchyma; a probable fracture of the right nasal pyramid was noted.
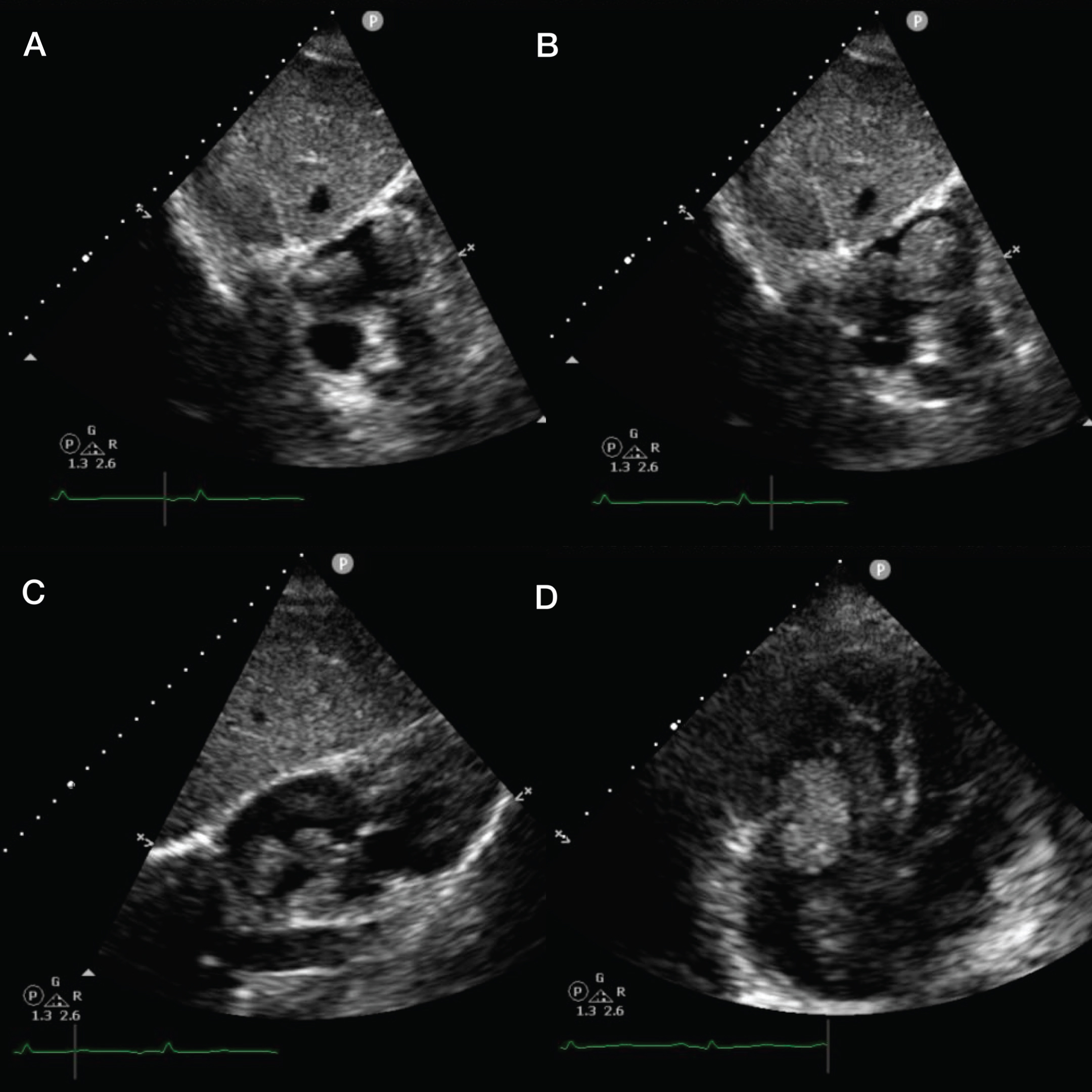
• Echocardiography: Reported filling defects in the right atrium suggestive of thrombi, increased contractility, and the presence of the Kissing wall sign. The vena cava was measured at 1.6 cm, with collapse exceeding 50%, demonstrating a pulmonary A pattern (Figure 1).
• The pulmonary angio CT revealed the following findings: The diameter of the inferior vena cava reached up to 30 mm in the intrahepatic segment, displaying multiple intraluminal filling defects with an oval tubular morphology, extending from the right common iliac vein. The largest defect, measuring 71 mm in length, was situated in the infrarenal segment of the inferior vena cava and exhibited soft tissue density (30 HU). Additionally, the left ovarian and renal veins were prominent, with acentral filling defect evident in the latter middle third. No additional intraluminal filling defects were identified. The heart showed mild enlargement, particularly affecting the right chambers. Furthermore, four ovoid intracavitary filling defects, characterized by soft tissue density (46 HU), were observed within the atrial chambers. One of these defects, originating from the intrahepatic segment of the inferior vena cava, extended into the ipsilateral ventricle through the tricuspid valve ring during the venous phase of acquisition (diastole) (Figure 2 and Figure 3).
Emergency surgery was conducted on July 14, 2023, to excise solid tumors located in the right cavum-atrial area. Three pieces, each approximately 12 × 3 cm in size, were protruding from the inferior vena cava. The tricuspid valve was examined during the procedure without encountering any complications. Specimens were subsequently sent for pathological study.
Pathology report (dated July 20, 2023):
• Macroscopic Description: A white mass with a fibrous consistency, resembling a cord, measuring 20 cm in length. At one end, it widens and measures 2.8 × 2 cm, while at the other end, it bifurcates into two cords approximately 6 × 5 mm in size (Figure 4).
• Microscopic Description: The examination reveals a benign neoplasm of muscular lineage, characterized by bundles of smooth muscle fibers. These fibers stain red when subjected to Masson's trichrome technique, resembling the staining pattern observed in the muscular walls of venous and arterial blood vessels. The tumor stroma consists primarily of fibrous connective tissue rich in collagen, resulting in predominantly blue staining with trichrome, indicating a neoplasm of considerable duration. The irregular intertwining of muscular bundles and collagenous connective tissue exhibits the characteristic appearance reminiscent of leiomyomas, resembling uterine leiomyomas (Figure 4).
The diagnosis of Intravascular Leiomyoma of the inferior vena cava projecting into the right atrium was confirmed.
Time line:
1 day: The patient presented to the emergency department with syncope, facial contusion and subsequent epistaxis.
2 days: She went into mixed shock, tonic-clonic seizures and sudden deterioration of consciousness.
3 days: Unremarkable head CT.
Echocardiogram with thrombus in transit
Day 0: Admission to our institute with suspicion of Pulmonary Embolism.
Angiotomography revealed multiple filling defects in the inferior vena cava, with the heart displaying mild enlargement primarily affecting the right cavities. Additionally, at least four ovoid filling defects were identified intra-auricularly, exhibiting soft tissue density.
1 day: The patient underwent a surgical procedure involving the excision of a right atrial tumor and examination of the tricuspid valve, with no reported complications.
2 days: Admission to the Intensive Care Unit (ICU).
7 days: Histopathology: Intravascular leiomyoma of the inferior vena cava projecting into the right atrium.
Tracheostomy is performed.
8 days: A gastrostomy is performed, and continues with no recovery of alertness.
11 days: Removal of mechanical ventilation.
18 days: Discharged from the Intensive Care Unit and transferred to the cardiology ward for palliative care.
25 days: Persistent vegetative state and uncontrolled hyperglycemia.
41 days: Deceased.
Discussion
Intravenous leiomyomatosis (IVLM) is characterized by the neoplastic extension of smooth muscle into venous pathways. Its progression to intracavitary leiomyoma is extremely rare and can consequently lead to heart failure and death [4]. From 1974 to September 2012, a total of 194 cases have been reported, with an increase in recent years despite the certainty of underreporting due to a lack of clinical suspicion and consequently diagnosis [5]. The last reported case in our country was in October 2012 [6].
According to Bin Li, et al., intracardiac leiomyomatosis (ICLM) primarily manifests through clinical symptoms such as dyspnea, syncope, lower extremity edema, palpitations, and, to a lesser extent, fatigue, ascites, jugular distension, chest, and abdominal pain. Nonetheless, a significant proportion of cases remain asymptomatic. The extension of ICLM typically aligns with symptoms of right heart failure, predominantly affecting the right atrium and ventricle [7].
Although IVLM is histologically benign, its clinical behavior is notably aggressive. Imaging modalities such as CT, MRI, and echocardiography are pivotal in assessing the extent of venous pathway involvement and in devising treatment strategies [8]. In the case at hand, echocardiography initially raised suspicion of a thrombus in transit, prompting further investigation by CT to delineate its origin and extent. The subsequent CT scan revealed intracavitary soft tissue suggestive of myomas. Consequently, after the surgical procedure, the identified thrombi originally diagnosed in the initial echocardiogram study were finally revealed as a tumor.
The tumor, extending from the uterus through the vena cava and confined to the right atrium, was classified as stage III according to the clinical staging system proposed by Ma, et al., This system comprises four stages: stage I involves the pelvic cavity, stage II extends beneath the renal vein (iliac vein/inferior vena cava), stage III encompasses cardiac chambers, and stage IV involves the pulmonary artery [9].
As mentioned above, the literature highlights the importance of conducting thoracic imaging studies in premenopausal females with a history of hysterectomy, pelvic surgery, uterine leiomyomatosis, and nonspecific symptoms [10].
In conclusion, it is crucial to consider a range of differential diagnoses, including thrombi in systemic veins, leiomyosarcoma of the inferior vena cava, right atrial myxoma, and malignant thrombus, given the varying clinical stages of each pathology and its association with ICLM, as they can be easily mistaken on imaging [11]. Additionally, clinicians and radiologists should adhere to a vigilant protocol for the diagnosis of IVLM [12,13].
Ethical Approval and Patient Consent
As submitted to the Research Committee and Ethics Research Committee of the National Institute of Cardiology Ignacio Chavez there is no found conflict for publishing this report.
Contributions
DMRO review of information, compilation and analysis of the case, elaboration of the manuscript, VJLA description of imaging, review of manuscript, MSML initial diagnosis on imaging, AAF diagnosis and interpretation of Pathology.
Acknowledgement
The authors express their gratitude to the Oficina de Apoyo Sistemático para la Investigación Superior (OASIS) at the National Institute of Cardiology Ignacio Chavez for their editing assistance in the elaboration of this manuscript.
Conflict of Interest Statement
All the authors claim no conflict of interest or funding to disclose.
References
- Peña A, Tamaña M (2018) Intracardiac extension of intravenous leiomyoma, a rare phenomenon: A case report. Radiology Case Reports 13: 427-430.
- Hernández-Flórez C, Jojoa-Jojoa RI, García-Peña ÁA, et al. (2018) Giant intravascular leiomyomatosis with extension to the cardiac cavities. Revista Colombiana de Cardiologia 25: 239e1-239e4.
- Wu CK, Luo JL, Yang CY, et al. (2009) Intravenous leiomyomatosis with intracardiac extension. Internal Medicine 48: 997-1001.
- Bhoil R, Thakur V, Verma YS, et al. (2020) Intravenous leiomyomatosis with intracardiac extension managed by one-stage surgical excision: A case presentation. Egyptian Journal of Radiology and Nuclear Medicine 51: 39.
- Li B, Chen X, Chu YD, et al. (2013) Intracardiac leiomyomatosis: A comprehensive analysis of 194 cases. Interact Cardiovasc Thorac Surg 17: 132-138.
- Lescas Méndez OA, Cosme P, Rico H, et al. (2013) Leiomioma con extensión intracardiaca que condiciona insuficiencia cardiaca aguda Reporte de caso. Rev Fac Med 56: 33-38.
- Guillermo C, Mario V, Jaime S, et al. (2008) Leiomioma invasor a cavidades cardiacas.
- Li R, Shen Y, Sun Y, et al. (2014) Intravenous leiomyomatosis with intracardiac extension: Echocardiographic study and literature review surgical technique. Tex Heart Inst J 41: 502-506.
- Ma G, Miao Q, Liu X, et al. (2016) Different surgical strategies of patients with intravenous leiomyomatosis. Medicine 95: e4902.
- Marcia M, Alexandre A, João L, et al. (2012) Intravascular leiomyoma with heart extension. Clinics 67: 83-87.
- Zeng H, Xu Z, Zhang L, et al. (2016) Intravenous leiomyomatosis with intracardiac extension depicted on computed tomography and magnetic resonance imaging scans: A report of two cases and a review of the literature. Oncol Lett 11: 4255-4263.
- Tan Y, Han J, Wang Z, et al. (2024) Different clinical diagnosis end up in the same pathological diagnosis of intravascular leiomyomatosis: Two case reports. Medicine 103: e36887.
- Kikuchi DS, Goulbourne CA, Starbuck KD, et al. (2023) Case report: Intravenous leiomyomatosis with intracaval and intracardiac growth. Eur Heart J Case Rep 7: ytac464.
Corresponding Author
Dr. Víctor J Lara Ameca, Department of Radiology, National Institute of Cardiology Ignacio Chávez, Mexico City, 14080, Mexico, Tel: (+521)-229-230-6960.
Copyright
© 2024 Olguín DMR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.