Why Choose Jaydess® Anymore?
There are currently five types of levonorgestrel intrauterine devices (LNG-IUD) available in the UK; Benilexa® (52mg LNG), Jaydess® (13.5mg LNG), Kyleena® (19.5mg LNG), Levosert® (52mg LNG) and Mirena® (52mg LNG) [1]. Jaydess ® and Kyleena ® have an identical frame size, but Jaydess ® has a lower dose of levonorgestrel and a shorter licenced duration of three years. With the availability of Kyleena®, since 2018, ® , we aimed to establish if there is still a need for Jaydess ® .
We performed a retrospective case note review of patients who had Jaydess ® fitted between 2018 and 2022 in a Sexual Health Service in England. The records were reviewed to ascertain the reasons for choosing Jaydess ® . Clinician’s views on choosing Jaydess ® were sought via a qualitative survey.
58 Jaydess ® fittings in 42 patients were identified: age range 17 to 51. Ethnicity: 28(28 (66.7%) White-British, 2 (4.8%) White-Other, 4 (9.5%) Asian or Asian British-Pakistani, 1 (2.4%) Asian or Asian British-Other, 3 (7.1%) Black or Black British-African and 4 (9.5%) ethnicity not documented.
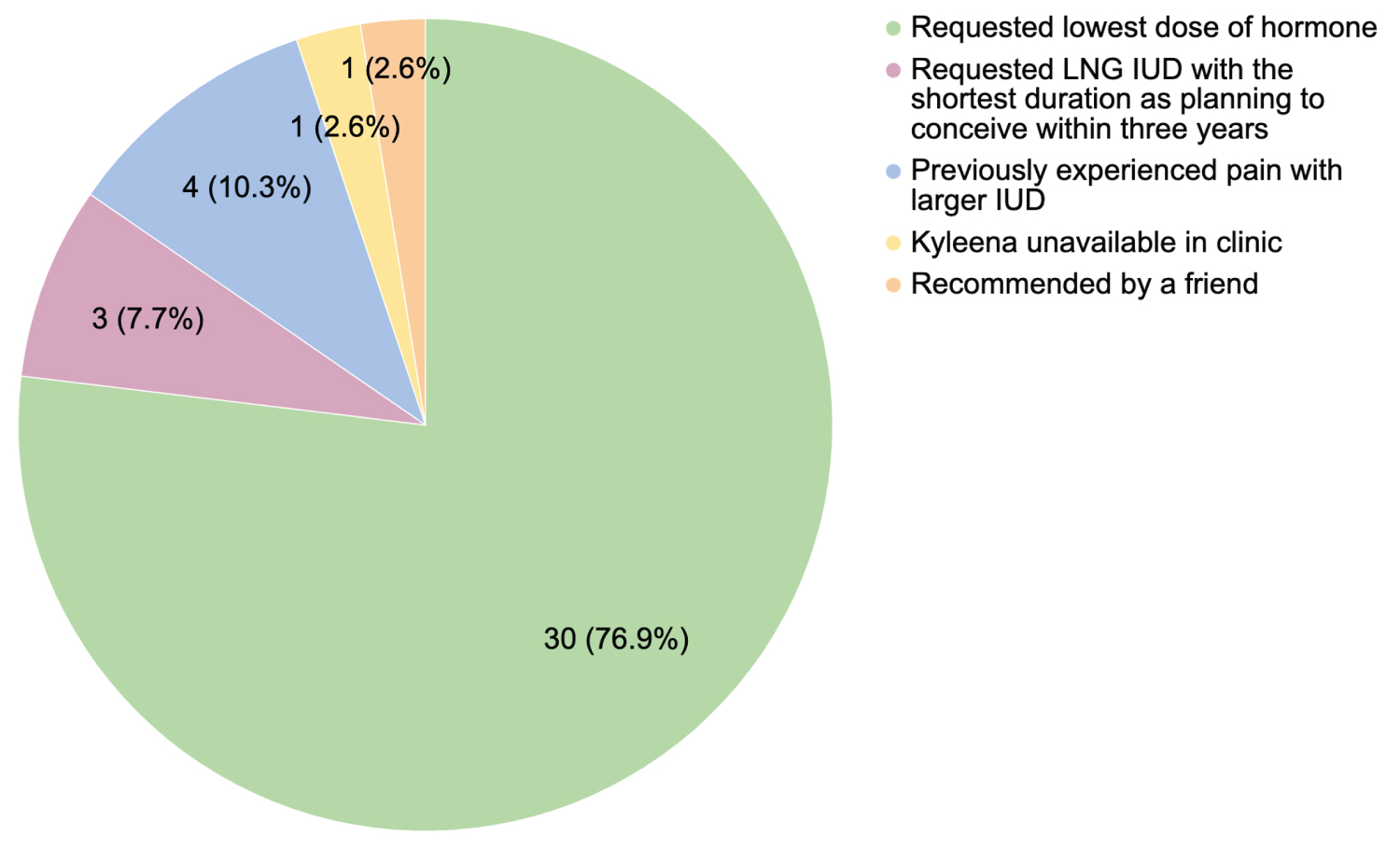
Reasons for specifically choosing Jaydess ® were documented in 31 patients, as seen in Figure 1.
30 patients specifically requested the lowest dose LNG-IUD (Jaydess®), of which 5 (16.7%) stated this was because they did not want their periods to stop. 15 (50.0%) initially requested a copper IUD to avoid hormones or to continue to menstruate, however, a copper IUD was deemed inappropriate due to history of heavy menstrual bleeding. 15 (50.0%) had prior negative experiences of hormonal contraception.
8 (21.1%) patients with ethnicity documented were from minority ethnic groups. Two of these patients specifically requested an LNG-IUD that would be least likely to cause amenorrhoea due to cultural beliefs about menstruation.
No pregnancies, including ectopic pregnancies, occurred with Jaydess ® in-situ.
Five clinicians completed a qualitative survey on the use of Jaydess ® . Clinicians agreed that patients are unlikely to ask for, or be aware of, specific types of LNG-IUD. The primary reason the clinicians would suggest a Jaydess ® to patients is if they requested a method with the lowest dose of hormone. One clinician stated that Jaydess ® is ideal for those who are reluctant to use any hormonal methods or who prefer to avoid amenorrhoea, despite attempts to reassure that amenorrhoea is not harmful. The clinician stated that some women with menorrhagia who initially request a copper IUD, specifically to avoid any hormones, often find Jaydess ® acceptable once advised that there is very little systemic absorption of hormone or that amenorrhoea is less likely. Three clinicians expressed that they favour Kyleena ® over Jaydess ® . One clinician stated that “Kyleena ® has surpassed the need for Jaydess”. Another said that they would “rarely even suggest Jaydess ® ” unless there is no other alternative.
Data from service users has highlighted that there is still both a need and demand for Jaydess ® , particularly in patients who feel strongly about having the lowest dose LNG-IUD. Clinicians noted that service-users are unlikely to be aware of Jaydess ® or the different LNG-IUD options. This survey also suggests a bias from clinicians themselves, who seem to favour other LNG-IUDs over Jaydess, which may mean fewer women are given the full complement of options available. An individualised, patient-centred discussion is important to address any beliefs or misconceptions regarding menstruation, whilst also recognising that the chance of amenorrhoea with LNG-IUD use isn’t always seen as a benefit by everyone. Detailed counselling, including an explanation of the different types of LNG-IUD is imperative for patients to make a fully informed choice. There is much evidence and guidance on who should be recommended a 52 mg LNG-IUD, in relation to gynaecological conditions [1]. However, little guidance exists regarding who should be recommended the lower dose LNG-IUDs.
References
Corresponding Author
Holly Mead, The Medical School, University of Sheffield, Beech Hill Road, Sheffield, S102RX, United Kingdom.
Copyright
© 2023 Mead H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.