Perinatal Outcome and Factors Associated with Hypertensive Disorders in Pregnancy in Yaoundé-Cameroon: A Retrospective Case-Control Study
Abstract
Background: Hypertension is the most common medical problem encountered during pregnancy complicating 10% of pregnancies. It is the third leading cause of maternal mortality and the first leading cause of perinatal mortality.
Objective: To determine the perinatal outcome and factors associated with hypertensive disease in pregnancy in Yaoundé
Materials and methods: A retrospective case-control study was carried out at the Yaounde Central Hospital. Data were extracted from files of women who presented with high blood pressure and those who had normal blood pressure during pregnancy from January 2018 to January 2019 using a structured questionnaire. A multi varite logistic regression analysis was done to determine risk factors of hypertension during pregnancy and Odds Ratio (OR), and their confidence intervals (CI) were obtained. Data were analyzed using SPSS version 20 softwares and level of significance was set at p < 0.05.
Results: We identified 147 cases of hypertension, a prevalence of 7.7%; and 147 cases with no hypertension, giving a total of 294 participants recruited. The proportion of preterm births was found to be 66% (97/147) in the hypertensive group compared to 19% in the non hypertensive group. There was a s statistically significant association between hypertension and age between 13-19 years-old (OR:2.15 [1.16-3.96], p = 0.014), nulliparity (OR:2.48 [1.36-4.50], p = 0.003), grand multiparity (OR: 3.92 [1.24-12.39], p = 0.02), low socioeconomic status (OR:3.24 [1.29-8.13], p = 0.012), low level of education (OR: 2.08 [1.03-4.17], p = 0.039), History of preeclampsia (OR: 19.02 [2.41-147.96], p = 0.005) and gestational age between 20-23 weeks at onset of Antenantal Care (OR:2.55 [1.25-5.19], p = 0.01).
Conclusion: The proportion of preterm births was high in hypertensive women compared to non hypertensive women during pregnancy. Hypertensive disease risk factors in pregnant women include: teenage, nulliparity, grand multiparity, lowsocioeconomic status, lowlevel of education, history of preeclampsia and advanced gestational age at onset of Antenatal care.
Keywords
Pregnancy, Hypertension, Prematurity, Yaoundé
Background
Pregnancy, although being a physiological phenomenon, can have a significant impact on the prognosis of the mother and/or the newborn when it is associated with certain pathologies. This is the case with hypertension during pregnancy. According to the World Health Organization (WHO), hypertension in pregnancy is defined as Systolic Blood Pressure (SBP) ≥ 140 mmHg and or DBP ≥ 90 mmHg [1]. Association of hypertension and pregnancy represents in black Africa the leadinggroup for cardiovascular pathology during pregnancy [2]. Due to the maternal-fetal complications that it causes and the complexity of its management, it is the third cause of maternal mortality (after hemorrhages and infections) and the first leading cause of perinatal mortality [3,4]. It is a real public health problem, with great variability in the figures reported around the world. The frequency of hypertension during pregnancy is similar in most western countries; 9.3% in France, 10.8% in the United Kingdom, 10 to 15% in the United States and 10% in Australia [5,6]. In China, a national survey reported a rate of 9.4% in 1994 [7]. There is also a great disparity inoccurence in African countries: 8.90-9.66% in Guinea Conakry; 17.05% in Niger, 3% in Dakar and 2.8% in Libreville [8,9]. The rates were 4.91% in 2012 in Fomba Nianankoro hospital (Mali) and 8.2% inYaounde Gynaeco-Obstetric and Pediatric Hospital in 2006 (Cameroon) [10,11].
The main objective of the study was to determine the perinatal outcome and factors associated with hypertensive disease in pregnancyin Yaoundé.
Materials and Method
Study design
The studywas a case-control study.
Study duration
We carriedout this study from January 2018 to January 2019.
Study setting
Presentation of the study location
History: The study took place atthe Obstetrics and Gynecology unit of the Yaounde Central Hospital (YCH), which is a referral category II hospital, in the pyramid of the health system in Cameroon. It is a social hospital which receives disadvantaged social strata. The Obstetrics and Gynecology unit has qualified staff and an adequate technical platform for the overall management of pregnancy complications.
Study population
Study population: Consist of all pregnant women followed-up at the maternity of the YCH.
Target population: Consisted of all pregnant women followed-up at the maternity between January 2018 and December 2018 who developed high blood pressure.
Inclusion and Exclusion criteria
Inclusion criteria:
Case: All pregnant women followed-up at the Yaoundé Central Hospital between January 2018 and January 2019 who developed hypertension.
Control: All pregnant women followed-up during the same period that did not develop high blood pressure.
Exclusion criteria
• Incomplete files.
• Files of pregnant women who had still born babies.
• Files of pregnant women who delivered babies within trauterine growth retardation.
Sample size determination
The sample size was determined by using Schlesselman formula. Therefore, the minimum sample size required for this study was 294 (147 cases, 147 controls).
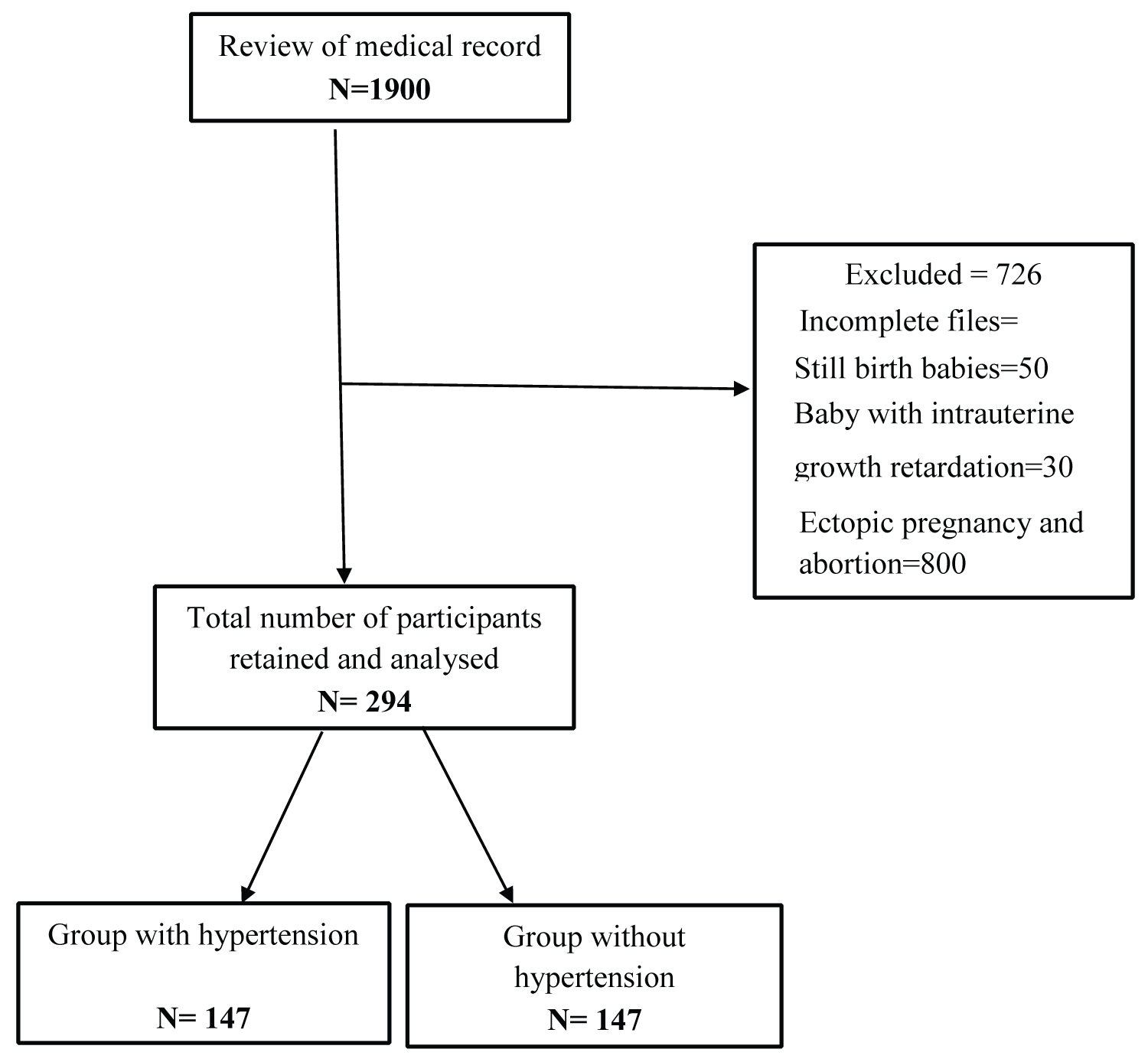
Recruitment process flow chart
A total of 1900 files were found among which 294 were selected. Out of the 294 files selected, 147 were hypertensive and 147 were non hypertensive (Figure 1).
Data analysis
Data were enterred in SPSS version 20 software, where a page wascreatedfor the study. Categorical variables were presented as frequencies and percentages, while continuous variables were presented as means and standard deviations (SD). Chi-square test was used to compare categorical variables. Finally, multi variate analysis was performed via multiple logistic regression and resoflogistic regression was expressed as adjusted odds ratio and 95% CI. A two-sided p < 0.05 was considered as statistically significant. The Microsoft excel 2016 software wasused to design the different tables and figures for the presentation of the results.
Ethical considerations
Ethical clearance was obtained from the institutional Review Board of the Faculty of Health Sciences, University of Bamenda.
Authorization to carry out the study at Yaounde Central Hospital wasacquiredfrom the director of the hospial.
Patients confidentiality was respected as participant identity (name, phone number, identity card number) wasn't revealed and the information collected was kept secret.
Results
Proportion of preterm birth
The hypertensive women were 4.8 time at risk of delivering premature babies (Table1).
Classification of differents types of hypertensive diseases
Preeclampsia was the most frequent pathology, representing 73.5% of cases, and a total 5.6% of deliveries (Table 2).
Factors associated with hypertensive disease in pregnancy
Sociodemo graphics characteristics and gestational age: Sociodemographics characteritics associated with hypertensive disease are: Adolesecent (teenage) group, primary and secondary level of education and the self-employed group (Table 3).
Obstetrical and family history
The frequency of primigravid a was much higher in the hypertensive group compared to non hypertensive.
The nulliparous and grand multiparous women were more at risk of developing hypertension,
Women with obstetrical history of preeclampsia were more at risk of developing hypertension during pregnancy (Table 4).
Follow up of the pregnancy
The majority of patients in the two groups had more than four Antenatal Clinic (ANC) contacts.
The most frequent pathology in our study population was malaria with occurrence of 13.6% in the hypertensive group and 46.2% in the non hypertensive group (Table 5).
Characteristics of preterm birth
There was no statistically difference in the two groups according to the characteristics of the preterm birth (Table 6).
Discussions
Proportion of preterm birth
Following our analysis, the proportion of preterm birth was found to be 66% in the hypertensive group compared to 19% in the non hypertensive group. Thus, Hypertensive women were more at risk of delivering premature babies and the risk was statistically significant. This can be explained by the fact that Yaoundé Central Hospital is a Referral hospital that receives patients from the city of Yaoundé and its environs. This is close to the results of Iouta, et al., study in Congo who reported 45% of premature babies in hypertensive group compared to 16.7% in the non hypertensive group [12]; with hypertension being a risk factor for prematurity which was statistically significant. Lower figures were reported in a 2016 publication by Davies, et al. in the United Kingdom [13]. The aim of their study was to determine the contribution of preeclampsia to preterm birth in primiparous women. The values observed were: 78.5% of premature babies in the hypertensive group compared to 85% in the non hypertensive group and this difference was statistically signifiacant (p value = 0.001).
Factors associated of hypertension disease
During the course of our study we found that adolescents were more at risk of developing hypertension during pregancy and the risk was statistically significant (OR: 2.15, and p value = 0.014). This is close to the results obtained by Dao, et al. in mali who found a statistically significant associattion between adolescence and hypertension during pregnancy [14]. Similarity was also seen in the 2013 study by Iouta, et al. in Congo [15], where adolescents were at risk of developing hypertension and the risk was statistically significant (OR: 2.44, p value = 0.0032). This can be explained by the concept of duration of exposure to sperm and paternal antigens, which can modify the immunological response. In fact, the shorter this duration, the higher the risk of hypertension in pregnancy and preeclampsia [15].
From our analysis, there was a statistically significant association between hypertension and lowlevel of education (OR: 2.08 p value = 0.039). This is close to the results of Iouta, et al. in Congo who found a statistically significant association between hypertension and lowlevel of education (OR: 5, p value = 0.001) [12]. In a study by Mboudou, et al. In Cameroon, participants with lowlevel of education were the most represented in the two groups; There was a statistically significant association between hypertension and lowlevel of education (p value = 0.001) [16].
Low socioeconomics status was also identified as a risk factor of hypertension during pregnancy in our study, and the risk was statiscally significant (OR: 3.24 p value of 0.012). This is close to the results obatined by Iouta, et al. in Congo who found an (OR: 2.04, and p value of 0.001). The same result hadbeen found by Mboudou, et al. in Cameroon in 2009 [16]. This can be explained by the lack of financial support necessary for the proper monitoring of pregnancy and probably the lack of insurance coverage.
Indeed, in our study, nulliparas were the most affected in the two groups, 73 (49.7%) in the hypertensive group and 52 (35.4%) in the non hypertensive group. There was a statistically significant association between hypertension in pregnancy and nulliparity (p value of 0.001). This is sligtly different from the results obtained by Mboudou, et al. Who found 38.01% in the hypertensive group and 34.3% in the non hypertensive group [16]. There wasn't a statistically significant association between hypertension in pregnancy and nulliparity (p value of 0.713). This can be explained by the difference in sample size of the case group 147 in this study versus 121 in their study. Added to this, in our study, grand multiparas were also at risk of developing hypertension during pregnancy and the risk was statistically significant (OR:2, p value of 0.02). This is close to the results of Iouta 2013 in congo who found a statistically significant association between hypertension and grand multiparity (OR:3.29, and p value of 0.001).
In our study, a statistically significant association was found between hypertension and history of preeclampsia (OR: 19, p value of 0.005). A similar observation was made in a 2007 study by Dao, et al. in Mali [14].
Characteristics of preterm birth
In our study, most premature babies delivered from women who developped hypertension during pregnancy were 61.9% male; while 38.1% were female. This is close to the results obtained by Naha, et al. in their 2020 study [17]. In their study, which aimed to investigate and analyze the clinical, and the rapeutic characteristics of new borns from preeclampticm others with premature delivery, 35 were male (58.5%) and 25 (41.7%) werefemale. Severalstudies have examined the relationship between fetal sex and preeclampsia, but their results have led to conflicting conclusions. Some studies found that the risk of preeclampsiais higher in mothers with a male fetus [18,19], while other studies found the contrary [20-23]. Most research could not find a relationship after multi variate analyses [18,20,21]. The Apgar score of preterm babies at the first minute of life waslowin 11.3% of cases, while in 88.7% cases, it was normal. The severity of the condition at birth could be explained by: the severity of hypertension (73.5% of preeclampsia in our study) and the decision to rescue a mother in danger (eclampsia or HELLP Syndrome). In El Mhamdi'sseries, 6% of new borns had an Apgar score lessthan 7 [24] and 94% of new borns who had an Apgar score greaterthan or equal to 7. In the Mabaga study it was reported that 37.9% of new borns from hypertensive women, had a low Apgar score during the first minute. These statements are consistent with the data demonstrated by the Schneider study: Low Apgar scores were a significant complication during child birth in hypertensive women [25].
Conclusion
• The proportion of preterm births in women with hypertensive disdorders in Yaoundé Central Hospital was found to be 66%.
• Risk factors for hypertensive disorder in pregnant women include: Age from 13 to 20 years, nulliparity, grand multiparity, low socioeconomic status, low level of education, history of preeclampsia and gestational age at onst of ANC from 11 to 23 weeks.
• The majority of premature babies born to hypertensive women had a weight ranging from 1600 grams to 2100 grams where as those born to non hypertensive women had a weight ranging from 2200 grams to 2500 grams. Most of the babies born to hypertensive women were male where as babies born to non hypertensive women were majority female. The majority of new borns in our study had an APGAR score less than 7.
• Premature baby's born from women who developed hypertension during pregnancy were at greater risk of having a poor Apgar score at birth.
Competing Interests
The authors have no conflicts of interest to declare for this study.
References
- Chamberlain G (1995) Obstetrics by tenteachers: Normal pregnancy. (16th edn), London: Edward Arnold.
- Priya SP, Piercy CN, Heli T, et al. (2016) Physiological changes in pregnancy. Cardiovasc J Afr 27: 89-93.
- Conrad KP (2011) Emergingrole of relax in in the maternal adaptations to normal pregnancy: Implications for preeclampsia. Semin Nephrol 31: 15-32.
- Cheung KL, Lafayette RA (2013) Renal physiology of pregnancy. Adv Chronic Kidney Dis 20: 209-214.
- Glinoer D (1997) The regulation of thyroid function in pregnancy: Pathways of endocrine adaptation from physiology to pathology. Endocr Rev 18: 404-433.
- Dorr HG, Heller A, Versmold HT (1989) Longitudinal study of progestins, mineralocorticoids and glucocorticoids throughout human pregnancy. J Clin Endocrinol Metabol 68: 863-868.
- Elsheikh A, Creatsas G, Mastorakos G, et al. (2001) The renin-aldosterone system during normal and hypertensive pregnancy. Arch Gynecol Obstet 264: 182-185.
- Gordon MC (2012) Maternal physiology in obstetrics: Normal and problem pregnancies. (6th edn), Philadelphia: Saunders, Elsevier.
- Linheimer MD, Barron WM, Davison JM (1991) Osmotic and volume control of vasopressin release in pregnancy. Am J Kidney Dis 17: 105-111.
- Yazbeck C, Thiebaugeorges O, Charles Aline M, et al. (2009) Maternal blood lead levels and the risk of pregnancy-induced hypertension The EDEN Cohort Study. Environmental Health Perspectives 117: 1526-1530.
- Dolea C, Abou Zahr C (2003) Global burden of hypertensive disorders of pregnancy in the year 2000, Evidence and Information for Policy (EIP) Geneva: World Health Organization.
- Itoua C, Ngounda BF, Ellenga GM, et al. (2013) Hypertension artérielle et grossesse: épidémiologie et pronostic maternofœtal au Centre Hospitalier Universitaire de Brazzaville. Medecine d'Afrique Noire 60: 21-29.
- Davies EL, Bell JS, Bhattacharya S (2016) Preeclampsia and preterm delivery: A population-based case-control study. The Journal of Hypertension in Pregnancy 35: 510-519.
- Dao ZS (2005) Hypertension artérielle et grossesse dans le service de gynéco-obstétrique du CHU Gabriel Touré à propos de 120 cas [Thèse de doctorat de médecine]. Bamako: FMPOS 72.
- Robillard PY, Hulsey TC, Perianin J, et al. (1994) Association of pregnancy-induced hypertension with duration of sexual cohabitation before conception. Lancet 344: 973-975.
- Mboudou ET, Foumane P, Belley Priso E, et al. (2009) Hypertension au cours de la grossesse: Aspects cliniques et épidémiologiques à l'Hôpital Gynéco-Obstétrique et Pédiatrique de Yaoundé, Cameroun. Clinics in Mother and Child Health 6: 1087-1093.
- Bakker R, Steegers EAP, Hofman A, et al. (2011) Blood pressure in different gestational trimesters, fetal growth, and the risk of adverse birth outcomes the generation r study. Am J Epidemiol 174: 797-806.
- Conde-Agudelo A, Belizán JM (2000) Risk factors for pre-eclampsia in a large cohort of Latin American and Caribbean women. BJOG 107: 75-83.
- Magnus P, Eskild A (2001) Seasonal variation in the occurrence of pre-eclampsia. BJOG 108: 1116-1119.
- Ros HS, Cnattingius S, Lipworth L (1998) Comparison of risk factors for preeclampsia and gestational hypertension in a population-based cohort study. Am J Epidemiol 147: 1062-1070.
- Phillips JK, Bernstein IM, Mongeon JA, et al. (2004) Seasonal variation in preeclampsia based on timing of conception. Obste. Gynecol 104: 1015-1020.
- Brettell R, Yeh PS, Impey LWM (2008) Examination of the association between male gender and preterm delivery. Eur J Obstet Gynecol Reprod Biol 141: 123-126.
- Shiozaki A, Matsuda Y, Satoh S, et al. (2001) Impact of fetal sex in pregnancy-induced hypertension and preeclampsia in Japan. J Reprod Immunol 89: 133-139.
- Dekker G, Robillard PY, Roberts C (2001) The etiology of preeclampsia: The role of the father. J Reprod Immunol 89: 126-132.
- Schneider S, Freerksen N, Maul H, et al. (2011) Risk groups and maternal-neonatal complications of preeclampsia current results from the national german perinatal quality registry. J Perinat Med 39: 257-265.
Corresponding Author
FOUEDJIO Jeanne Hortence, Department of Obstetrics and Gynecology, Unviversity of Yaoundé I; Yaounde Central Hospital, Cameroon, Tel: 00237-696818339/00237673795023.
Copyright
© 2022 Fouedjio JH, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.