Basal Cell Carcinoma Arising within a Fibroepithelial Polyp: A Case Report
Keywords
Basal cell carcinoma, Skin cancer, Fibroepithelial polyp, Skin tag, Acrochordon
Abbreviations
BCC: Basal Cell Carcinoma; FEP: Fibroepithelial Polyp
Introduction
Basal cell carcinoma (BCC) is the most common cancer both worldwide and in the United States. Approximately 4.3 million cases of BCC are diagnosed in the United States each year [1]. It typically arises on sun-damaged skin, the majority being on the head and neck, though cases on the trunk and lower extremities are not uncommon. Independent risk factors for developing BCC include ultraviolet light exposure, light-colored skin, age, male sex, exposure to arsenic, radiation, previous skin cancer, and inherited conditions such as xeroderma pigmentosum and basal cell nevus syndrome [1]. Two main characteristics distinguish superficial BCC on histology: Basal cell buds with peripheral palisading arising from the basal layer of the epidermis, and retraction artifact [2].
Fibroepithelial polyps (FEPs), also known as “skin tags” or “acrochordons,” are common cutaneous lesions formed from soft excrescences of skin. FEPs are generally considered benign and have low rates of containing other pathology. In a comparative study from 1996, 1335 unsuspicious FEPs were examined and only 5 showed malignant tumors on histology, three of which were BCC [3].
Despite the high prevalence of both BCC and fibroepithelial polyps, BCC has only been reported five times as occurring in a FEP [3-5]. Herein, we describe such a case.
Methods
We conducted a literature review in PubMed using combinations of the terms “basal cell carcinoma,” “basaloid induction,” or “basaloid follicular induction” combined with “fibroepithelial polyp,” “acrochordon,” or “skin tag”.
Case Report
A 55-year-old male presented to an outpatient clinic for removal of a fibroepithelial polyp on the left lateral inferior chest (Figure 1). The patient’s history includes previous work as a truck driver and no personal or family history of melanoma. A 0.6 by 0.5 by 0.4 cm, tan, polypoid piece of skin was removed by shave biopsy and submitted for histologic evaluation.
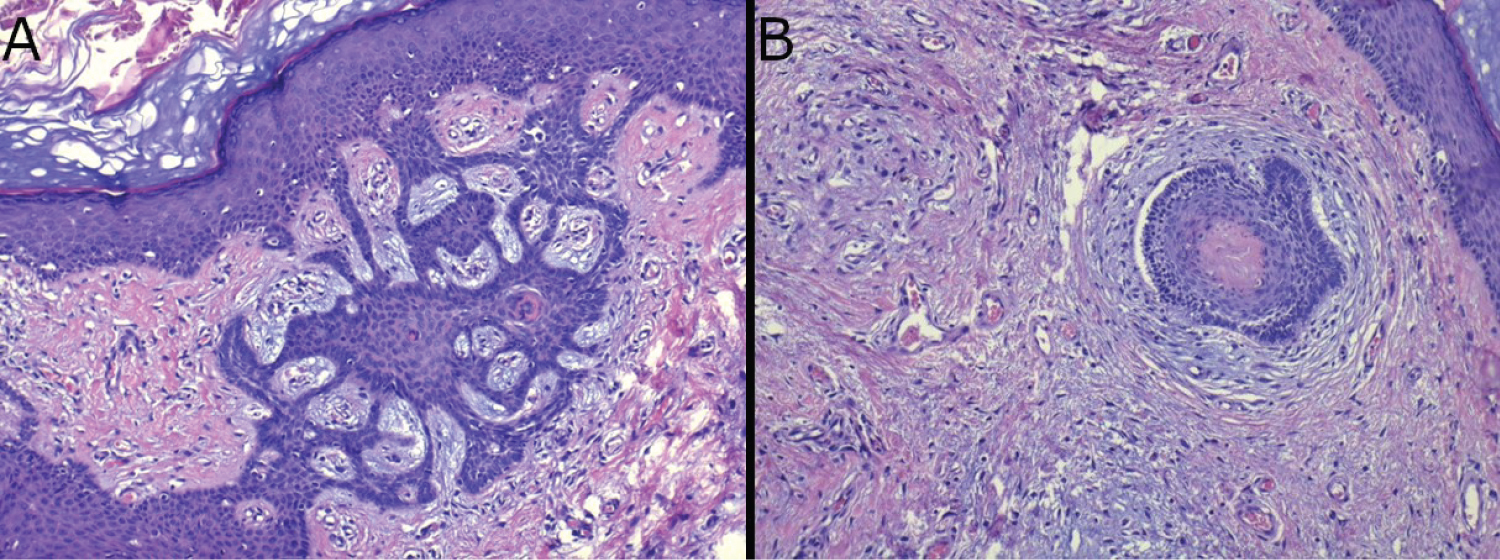
Histological evaluation revealed papillomatosis, acanthosis, loose connective tissue, and lymphocytic infiltrate. These findings were characteristic of an inflamed fibroepithelial polyp. There were also islands of atypical basaloid cells with peripheral palisading and retraction artifact from the surrounding superficial stroma that were attached to overlying epidermis, which was consistent with superficial BCC (Figure 2). The examined margins appeared free of BCC, but this was difficult to determine definitively given the plane of sectioning. The differential diagnosis also included basaloid follicular induction; however, the retraction artifact and stroma were more consistent with that of BCC.
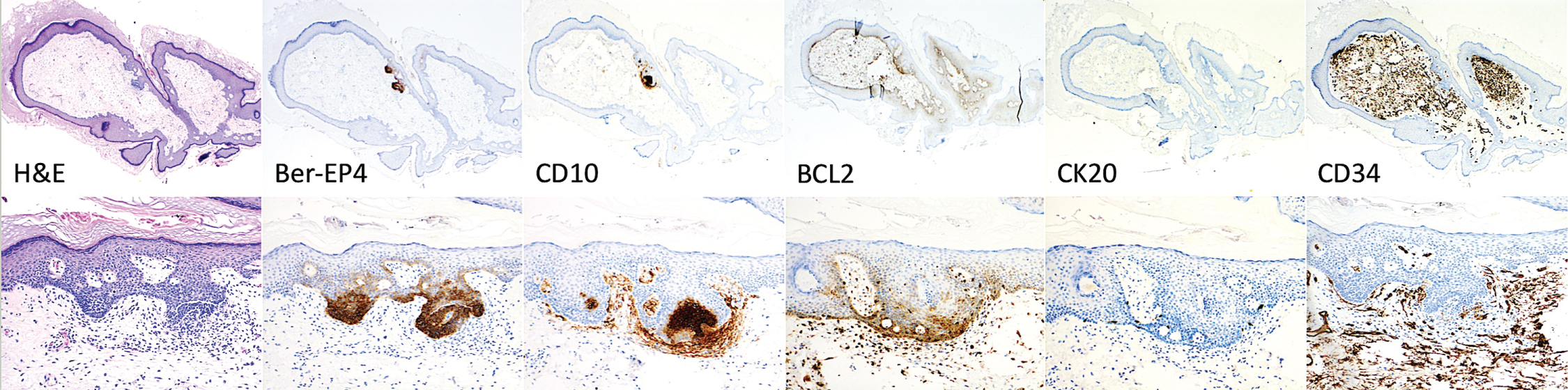
Immunohistochemistry stains further supported characterizing the lesion as BCC. Figure 3 and Table 1 show Ber-EP4, CD10, BCL2, CK20, and CD34 immunohistochemistry stains. The staining pattern of the case matches that of BCC and is distinct from other potential histological mimics, such as trichoepithelioma, squamous cell carcinoma, Merkel cell carcinoma, and a tumor of follicular infundibulum [6-8]. Our case stained positively for Ber-EP4, CD10, BCL2, and negative for CK20 and CD34. This matches the staining profile found in BCC, and notably differs from trichoepithelioma, SCC, Merkel cell carcinoma, and tumor of follicular infundibulum.
Another lesion that was in the differential was Fibroepithelioma of Pinkus [9]. This is a malignant fibroepithelial tumor, historically classified as a variant of BCC, that is characterized by numerous cords of basaloid cells that extend into dermis. It often appears on the trunk and can appear clinically to mimic a FEP. The absence of Merkel cells on IHC removes suspicion that this lesion is actually fibroepithelioma of Pinkus.
Discussion
We present an unusual case of BCC arising in a FEP in a middle-aged white male. To our knowledge, there have only been five other cases of a BCC in a FEP present in the literature. The first was reported arising from a FEP in the axilla of a 59-year-old woman [4]. The second, third, and fourth were reported as part of survey of 1553 FEPs without further information as to their presentation [3]. The fifth was one skin tag out of five removed from the nape of a 59-year-old man [5]. He had no personal or family history of skin cancer, no precancerous lesions on dermatological exam, and had a history of exposure to sun during outdoor activities. In all five cases, as well as our own, a diagnosis of BCC was not expected by the submitting physician.
Eads and colleagues asserted that since the rate of malignant tumors in non-suspicious FEPs submitted by dermatologists was zero, FEPs need not be submitted by dermatologists to rule out malignancy [3]. While we agree that avoiding routine submission of FEPs for histological confirmation is cost saving and generally low risk, it is worth considering a patient’s risk factors for skin cancer when determining if a FEP should be submitted. It is not unreasonable to routinely submit FEPs for histological examination so that concomitant pathology, such as BCC, can be appropriately followed up. An estimated 30-50% of patients with BCC will develop another BCC within 5 years, which is a 10-fold increase in comparison to the general population [10]. The National Comprehensive Cancer Network (NCCN) recommended follow up after diagnosed BCC of skin examination every 6 to 12 months for the first five years, and then annually for life [10]. This continued surveillance, which may be overlooked in patients who are recommended for follow-up, helps mitigate tissue destruction and morbidity from more advanced cases of BCC.
To our knowledge, there are only five other cases of a superficial BCC arising in a FEP reported in the medical literature. Our case reiterates that BCC can occur in a FEP, potentially remaining undetected. Since FEPs are often discarded rather than submitted for histologic examination, the true prevalence of BCC in FEP, and the true incidence of BCC overall, may be underestimated. This also represents a missed opportunity for cancer diagnosis, follow-up, and prevention of recurrence.
Funding Statement
This article has no funding source.
Potential Conflicts of Interest
The authors declare the following potential conflicts:
• Jacob Shaner BS has no conflict of interest to disclose.
• Kristian Schafernak MD has no conflict of interest to disclose.
• Neil Fernandes MD is a paid physician speaker for Castle Biosciences, Sanofi, and Regeneron.
References
- American Cancer Society (2023) Basal and squamous cell skin cancers.
- Correia de Sá TR, Silva R, Lopes JM (2015) Basal cell carcinoma of the skin (part 2): Diagnosis, prognosis and management. Future Oncol 11: 3023-3038.
- Eads TJ, Chuang TY, Fabré VC, et al. (1996) The utility of submitting fibroepithelial polyps for histological examination. Arch Dermatol 132: 1459-1462.
- Hayes AG, Berry AD 3rd (1993) Basal cell carcinoma arising in a fibroepithelial polyp. J Am Acad Dermatol 28: 493-495.
- Aksoy B, Aksoy HM, Ustün H, et al. (2008) Basal cell carcinoma in a skin tag. Eur J Dermatol 18: 605-606.
- Smoller BR, Van de Rijn M, Lebrun D, et al. (1994) bcl-2 expression reliably distinguishes trichoepitheliomas from basal cell carcinomas. Br J Dermatol 131: 28-31.
- Heidarpour M, Rajabi P, Sajadi F (2011) CD10 expression helps to differentiate basal cell carcinoma from trichoepithelioma. J Res Med Sci 16: 938-944.
- Stanoszek LM, Wang GY, Harms PW (2017) Histologic Mimics of Basal Cell Carcinoma. Arch Pathol Lab Med 141: 1490-1502.
- Zalaudek I, Ferrara G, Broganelli P, et al. (2006) Dermoscopy patterns of fibroepithelioma of pinkus. Arch Dermatol 142: 1318-1322.
- National Comprehensive Cancer Network (2023) Basal Cell Skin Cancer. 1.2024 version.
Corresponding Author
Neil F. Fernandes, University of Arizona College of Medicine - Phoenix, 725 South Dobson Road Suite 200, Chandler, AZ, 85224, USA, Tel: 480-899-7546.
Copyright
© 2024 Shaner J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.