A Challenging Diagnosis: Primary Cutaneous Leiomyosarcoma, Initially Resembling a Dermatofibroma
Abstract
We present a case of primary cutaneous leiomyosarcoma misdiagnosed as a benign tumor. Primary cutaneous leiomyosarcomas are very difficult to diagnose preoperatively because clinical presentation and imaging studies are nonspecific and do not allow an adequate differential diagnosis with other skin lesions. Therefore definitive diagnosis is based on the pathology report. The best treatment consists of complete surgical removal of the lesion with safety margins. The prognosis is difficult to predict and adjuvant therapy may be helpful in cases of positive or borderline surgical margins, or metastatic disease.
Keywords
Leiomyosarcoma, Mesenchymal neoplasm, Soft tissue sarcoma, Skin cancer
Case Report
Introduction
Leiomyosarcomas (LMS) are uncommon malignant neoplasms derived from smooth muscle cells. They can present in a wide variety of soft tissues and visceral locations such as the retroperitoneum, gastrointestinal tract, blood vessels, uterus, subcutaneous tissue and dermis.
Case presentation
A 54-year-old man presented to our department with an asymptomatic nodule located at left thigh. The patient had no relevant medical history. Physical examination revealed a 1.5 cm exophytic lesion, well-delimited with an irregular surface and a firm elastic consistency. There were no signs of skin infection such as warm, erythematosis, edema or tenderness. There was no history of external injury or infection was present. Routine laboratory blood tests were within normal limits.
He underwent surgery with a presumptive diagnosis of dermatofibroma. Under local infiltration anesthesia, a complete surgical excision of the tumor was performed with safety margin of 1 cm.
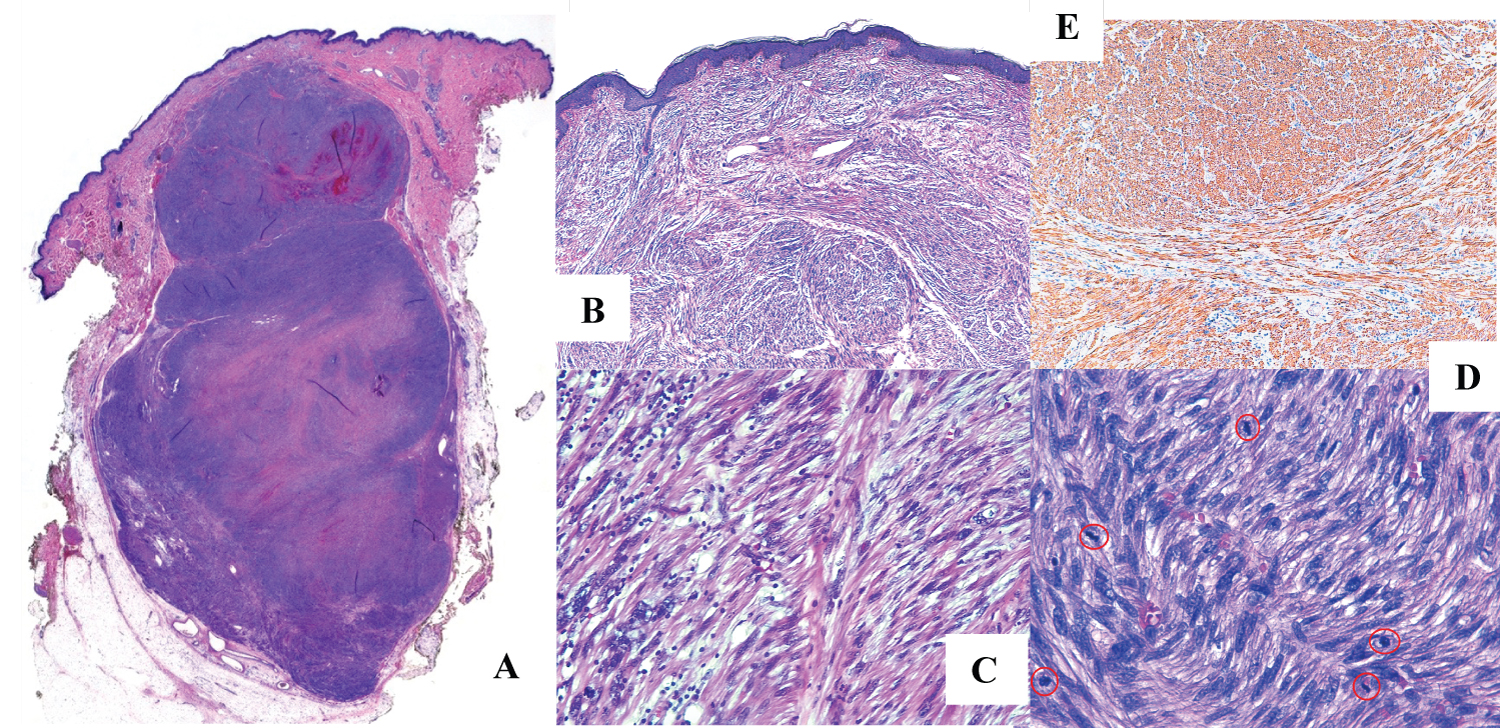
Histological examination revealed a high-grade mesenchymal tumor with a nodular growth pattern and an infiltrative growth pattern up to the upper reticular dermis. It measured 3 × 2 × 2.2 cm. Negative margins, areas of necrosis, eosinophilic cytoplasms, pleomorphic nuclei, severe nuclear atypia and a mitotic index of 20 mitoses per 10 high-power fields, were also described. Immunohistochemical analysis revealed that tumor cells stained positive for actin, h-caldesmon, desmin and CAM 5.2. Immunohistochemical markers were negative for S100, CD117, CD 34, CD 10, p63, MIB-1 Y Phosphohistone-H3. Therefore, the tumor was diagnosed as a primary cutaneous leiomyosarcoma (Figure 1A-Figure 1E).
Given the pathological results, the multidisciplinary oncology team decided to perform re-excision with wide surgical margins (> 1.5 cm), enlarged to the fascial tissue. Pre-operative staging computed tomography (CT) scan showed a lytic lesion in the D11 vertebral body, but Tc-99 radionuclide bone scan did not show metastatic disease.
Finally, a local re-excision (9 × 5 × 2 cm) was performed to obtain wider margins under general anesthesia. The pathology report found no tumor tissue in the sample received. The postoperative period was uneventful and he was discharged the day after surgery.
After 5 years of follow-up, the patient remains asymptomatic and there is no clinical or radiological sign of recurrent or metastatic disease.
Discussion
Primary cutaneous leiomyosarcomas (PCL) are an extremely rare subtype of leiomyosarcomas, which have been described in small series and case reports. PCL arise from the arrector pili muscle of the skin and represent 1%-3% of all sarcomas [1]. They are frequently diagnosed in middle-aged men [2]. The etiology is unknown, but a history of radiation therapy, genetic syndromes, and the Epstein Barr virus may be predisposing factors [3]. PCL present mainly as a solitary, firm, slow-growing nodule [4]. The clinical presentation is usually nonspecific or indolent, so it can sometimes be difficult to distinguish it from other tumors such as dermatofibromas. In this case, the previous misdiagnosis of the tumor is interesting. Since it can cause a delay in tumor resection that can lead to oncological progression. Therefore, the definitive diagnosis is based on histopathological and immunohistochemical examinations. There are two growth patterns: Nodular and diffuse. The first is characterized by high cellularity, nuclear atypia and mitotic figures. Whereas the diffuse growth pattern is characterized by low cellularity and less mitotic figures [4].
A preoperative biopsy is a controversial issue, because small biopsy samples sometimes provide inaccurate results. We did not perform a biopsy in this case because we thought it was a benign tumor.
PCL are great mimickers, so differential diagnosis includes granulomatous lesions, benign soft tissue tumors and malignant cutaneous tumors [5]. Although the diagnosis of PCL may be suspected on imaging studies, pre-operative staging is not usually necessary. However, a CT scan, Magnetic resonance imaging (MRI) or Positron emission tomography (PET) imaging may be useful to show metastatic disease.
Complete surgical excision with negative margins is the treatment of choice. Recurrence or metastasis can occur in tumors with incomplete resection or positive surgical margins. There are no standard guidelines. However, radiation and chemotherapy may provide variable outcomes [6].
The malignant potential of PCL is difficult to predict, although small series suggest an intermediate risk of aggressive behavior. Aneiros-Fernandez, et al. [7] reported a recurrence rate of 24%, low metastatic potential (4%) and mortality of 3%. Long-term clinical follow-up with imaging exams is strongly recommended, given the unpredictable behavior of PCL and the possibility of late relapses.
In conclusion, a primary cutaneous leiomyosarcoma is an extraordinary finding, and preoperative diagnosis can be a challenge. Surgery resection with negative margins seems to be the only curative treatment. Due to the lack of knowledge and high-quality evidence, the malignant potential and prognosis of PCL remain unknown. Furthermore, we suggest that postoperative long-term follow-up should be mandatory, and further high-quality studies are needed to understand the behavior of these type of sarcomas.
Author Disclosure Statements
Nothing to disclose.
Financial Disclosures
The authors report no conflict of interest.
References
- Deneve JL, Messina JL, Bui MM, et al. (2013) Cutaneous leiomyosarcoma: A single institution experience of treatment and outcomes with a standardized margin of resection. Cancer Control 20: 307-312.
- Sleiwah A, Clinton A, Herbert K (2018) Delayed diagnosis of dermal leiomyosarcoma mimicking keloid scar. BMJ Case Rep.
- Mangla A, Yadav U (2019) Leiomyosarcoma. StatPearls Publishing.
- Llombart B, Serra-Guillén C, Requena C, et al. (2019) Leiomyosarcoma and pleomorphic dermal sarcoma: Guidelines for diagnosis and treatment. Actas Dermo-Sifiliográficas 110: 4-11.
- Vestita M, Filoni A, Ingravallo G, et al. (2015) Recurrent cutaneous leiomyosarcoma of the inner thigh. Indian J Dermatol Venereol Leprol 81: 309.
- Massi D, Franchi A, Alos L, et al. (2010) Primary cutaneous leiomyosarcoma: Clinicopathological analysis of 36 cases. Histopathology 56: 251-262.
- Aneiros-Fernandez J, Antonio Retamero J, Husein-Elahmed H, et al. (2016) Primary cutaneous and subcutaneous leiomyosarcomas: Evolution and prognostic factors. Eur J Dermatol 26: 9-12.
Corresponding Author
Sara Alonso Batanero, M.D, Department of General and Gastrointestinal Surgery, El Bierzo Hospital, Médicos Sin Fronteras, 7, 24411 Fuentesnuevas (León), Spain, Tel: +34-987455200, Fax: 987-45-53-00.
Copyright
© 2021 Alonso-Batanero S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.