Barriers and Facilitators of Cervical Cancer Screening among Tanzanian Women: A Systematic Review
Abstract
Background: Cervical cancer is a major concern in Tanzania, with one of the highest global prevalence rates and the highest in East Africa. Despite this, a low percentage of Tanzanian women undergo screening. This systematic review seeks to identify the factors affecting access to cervical cancer screening, focusing on the perspectives of Tanzanian women, healthcare workers, and key informants. The objective is to use this insight to develop initiatives that increase screening rates and ensure timely diagnosis for women with precancerous lesions.
Methods: This analysis included 17 studies (12 quantitative, 4 qualitative, and 1 mixed-method), involving 9698 women, 55 healthcare professionals, and insights from 35 key informants. These studies were published between 2012 and 2023. Data collection was conducted by two reviewers, categorizing findings by study characteristics, quality, facilitators, and barriers.
Results: In the comprehensive study spanning all regions of Tanzania, 28 barriers and 19 facilitators were uncovered. Notably, barriers often revolved around limited knowledge, stigma, resource constraints, and access challenges. Conversely, facilitators encompassed positive attitudes, education level, social support, and healthcare worker endorsements, with variations in study quality.
Conclusion: Gaining a deeper understanding of the factors affecting cervical cancer screening in Tanzanian women is crucial for increasing screening rates. To achieve this, conducting more precise and reliable research is essential to enhance data credibility. This, in turn, will enable informed interventions to eliminate barriers and support screening-promoting factors.
Keywords
Cervical cancer, Cervical cancer screening, Barriers, Facilitators, Tanzania
Background
Cervical cancer (CC) primarily results from persistent infection with the human papillomavirus (HPV), particularly the high-risk subtypes 16 and 18 [1]. HPV is found in 99.7% of reported CC cases [2]. The most prevalent CC types are squamous cell 70% and adenocarcinoma 25%. Globally, CC ranks as the fourth most prevalent cancer among women, resulting in approximately 500,000 new cases and an estimated 250,000 fatalities annually [3]. Notably, the heaviest burden of CC falls upon developing nations, which bear 85% of the global cases and nearly 90% of the associated deaths [3,4]. Tanzania, among the world's poorest nations, experiences a CC incidence rate 1.6 times higher than the East African regional average, which holds the highest incidence rate globally [5]. CC is the primary cause of female cancer in Tanzania, resulting in 9772 new cases and 6695 fatalities annually [6].
In 2020, Tanzania stood as the fourth highest globally in CC incidence, with 62.5 new cases per 100,000 women, age-standardized to the global population [7]. This rate far exceeded the figures in North America (6.6) and Australia/New Zealand (5.5) [8]. Additionally, CC mortality in Tanzania was notably high, with 42.7 deaths per 100,000 women in the same year [7], compared to the global age-standardized mortality rate of 6.8 [8]. Given the substantial disease burden, these numbers emphasize the pressing need for effective CC prevention and control measures in Tanzania.
Detecting and treating pre-cancerous lesions is a vital secondary step in the World Health Organization's (WHO) four-pronged strategy to prevent CC [9]. CC has an extended pre-invasive phase, allowing for the identification of precancerous changes through screening before they develop into invasive disease. This early intervention is key to reducing the impact of CC. The utilization of Pap smears for screening has been successful in preventing up to 80% of CC cases in well-resourced countries [10]. In Tanzania, limited infrastructure and personnel impede Pap smears. As an alternative, visual inspection with acetic acid (VIA) followed by cryotherapy for precancerous lesions (screen and treat), offered at no cost in government and faith-based hospitals at various care levels, is widely endorsed for early CC detection [11].
Comprehending the factors that drive or hinder women's participation in CCS is essential for enhancing preventive measures and reducing the occurrence of invasive CC and related mortality. While a few systematic reviews have explored barriers and facilitators to CCS uptake in Sub-Saharan Africa (SSA), to our knowledge, this is the first systematic review concentrating on this matter within Tanzania.
CC affects women during their most productive years, resulting in significant social and economic repercussions for families and communities. The high incidence and fatality rates in Tanzania, despite the preventable nature of the CC, are unacceptable. This study aims to systematically review existing research on factors influencing CCS uptake among Tanzanian women and offer informed guidance for future public health efforts. The insights gained will shape the development of CCS promotion and educational programs to boost screening among asymptomatic women and facilitate the early detection of CC symptoms.
Objectives of the Study
i. To systematically identify and analyze the barriers preventing Tanzanian women from accessing cervical cancer screening.
ii. To use the gathered insights to develop evidence-based initiatives that will lead to a significant increase in cervical cancer screening rates in Tanzania.
Methods
This systematic review followed the PRISMA guidelines [12]. In July 2023, an extensive literature search was carried out across Ovid MEDLINE, PUBMED, EMBASE, PsycINFO, and SCOPUS. Both subject-specific and keyword searches were performed individually in each database and then combined using 'OR' and 'AND' operators. The search terms included MeSH terms like 'cervical cancer,' 'cervical neoplasms,' 'cervical cancer screening,' 'HPV testing,' 'pap smear,' 'visual inspection with acetic acid,' as well as keywords related to 'barriers,' 'facilitators,' 'utilization,' 'Tanzania,' 'East Africa,' and 'Sub-Saharan Africa.' The search was restricted to articles published from 2012 onwards and written in English. In addition to the database searches, the review encompassed investigations on Google Scholar, the ProQuest. Theses and Dissertations database, manual scrutiny of reference lists from included articles, and consultations with experts in the field. The final search update was performed on October 15, 2023, and any newly discovered results meeting the specified criteria were included.
Data selection and synthesis
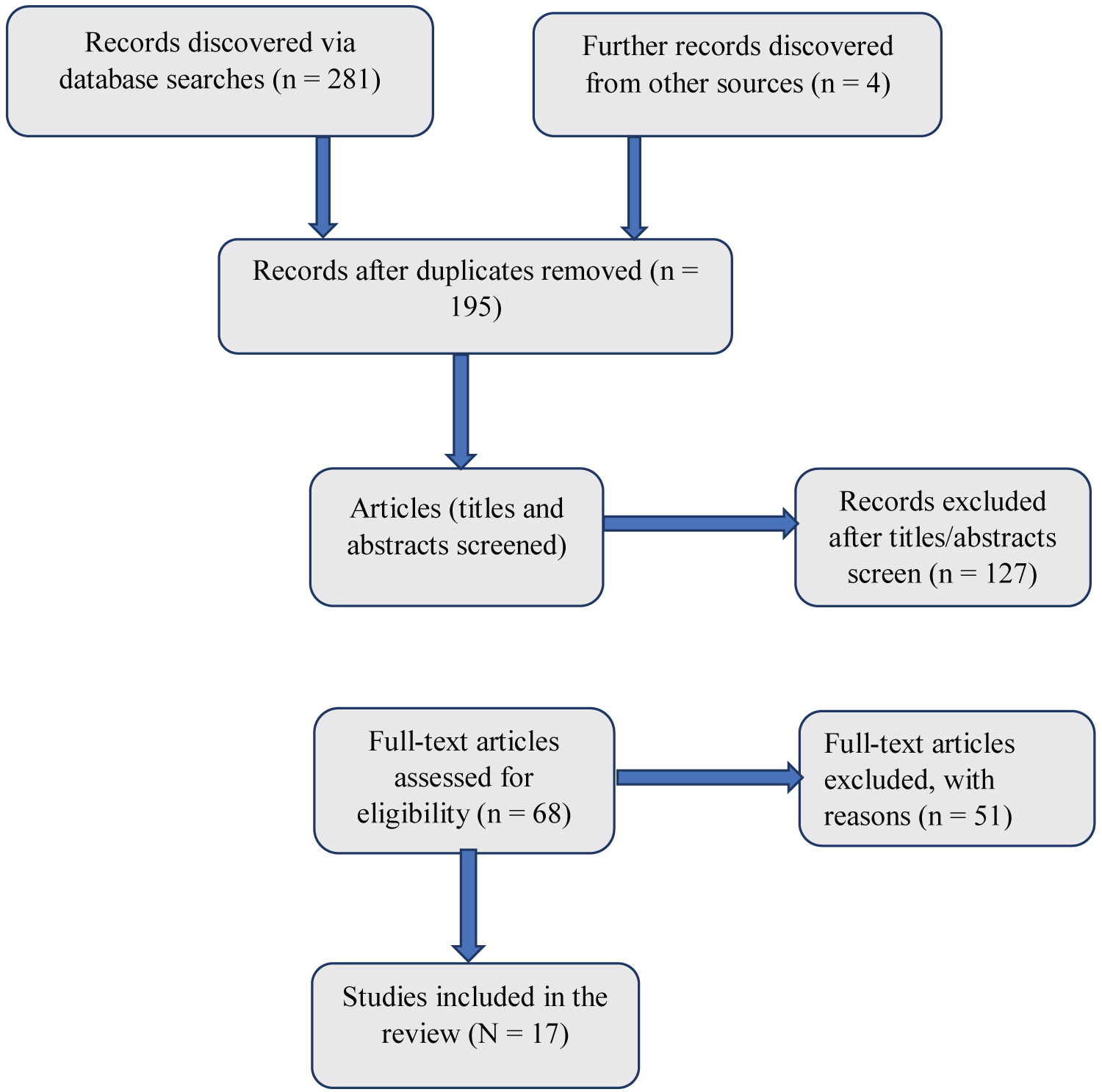
The initial database search yielded 281 articles, and an additional 4 articles were found through Google Scholar. After removing 86 duplicates and evaluating 195 abstracts, 127 studies were excluded for not meeting the inclusion criteria. Subsequently, a full-text review resulted in the exclusion of 50 more articles that did not specifically address enablers or barriers related to CCS in Tanzania (Figure 1).
Two authors (MMS and RRK) independently extracted data from the 17 remaining papers. Quantitative studies provided data on significant barriers and enablers related to CCS, along with participant proportions. Qualitative studies contributed to all the reported obstacles and enablers. Disagreements were settled by debate and agreement.
A meta-analysis was not possible due to diverse study designs, participants, and outcomes. Instead, the study data were used for narrative analysis, focusing on emergent themes related to barriers and facilitators in CCS.
Eligibility criteria
We included quantitative and qualitative studies that investigated barriers and/or facilitators to CCS uptake among women in Tanzania of any age. Quantitative studies were included to uncover associations between factors and screening uptake, while qualitative studies were included to explore barriers and facilitators reported by women, key informants and health care workers (HCWs). Studies involving HCWs and key informants were included as they could offer insights related to health system and resource factors.
Exclusion criteria
We excluded studies published before 2012, studies not in English or lacking full-text availability, and those that did not specifically address barriers or facilitators to CCS uptake among Tanzanian women. Studies focusing on women with HIV were also excluded as they encountered unique challenges in accessing screening services.
Quality assessment and analysis
To assess the quality of the research we included, we utilized a 16-item scale created by Sirriyeh, et al. [13]. This scale is adaptable and can be used for a variety of study designs. It employs a four-point grading system to assess the overall quality of research containing both qualitative and quantitative data. Given the fact that we had a limited number of research, we decided not to reject any based on their quality scores.
Results
Study characteristics
Inclusive of data from 2012 to 2023, our analysis encompassed 17 studies, which collectively examined urban and rural populations, as detailed in Table 1. Among these, 13 were cross-sectional, four employed qualitative methods like focus group discussions and key informant interviews. These studies encompassed 9698 women, 55 healthcare professionals, and input from 45 key informants.
When measuring the proportion of women screened, findings varied from 2.6% to 75.6% [20,31]. Significantly, studies that recruited participants from healthcare clinics exhibited elevated screening rates, potentially attributed to active encouragement or referrals by HCWs, but these results may not accurately reflect the broader Tanzanian population. In contrast, studies conducted at the household level and or using multi-stage sampling reported lower screening rates [15-17,20,28].
We acknowledges the potential risk of bias due to missing results, primarily arising from publication bias, which could skew the overall assessment of the effectiveness and challenges associated with CCS in Tanzania. Efforts were made to minimize this bias by including a diverse range of sources, including gray literature and unpublished studies, to ensure a more comprehensive evaluation of the available evidence.
Studies and evaluation of quality
Table 2 outlines the quality assessment findings. Quantitative study scores ranged from 22 to 39, while qualitative study scores ranged from 26 to 37. Four studies applied a theoretical framework, and 16 studies clearly defined their research settings and aims/objectives. In 12 studies, the sample represented the target population well. Seven studies offered comprehensive descriptions of data collection procedures, but only a few quantitative studies reported on survey tool reliability and validity. Most studies adequately explained their choice of analysis method. Several qualitative studies assessed reliability through various methods, while three studies did not report on this aspect.
Evaluation of the studies included
Barriers and facilitators towards CCS: Individual, Social and Structural. For this review, we classified barriers and enablers into three primary distinct groups: individual, socio cultural and structural factors.
Individual factors
A: Knowledge of CC/CCS
Inadequate knowledge and awareness of CCS were key barriers, as evidenced by qualitative [25,29,30] and quantitative studies [15,16,19-21,23,24,28,31,32]. Some women lacked knowledge of CC causes and screening methods, while HCWs struggled with confidence owing to insufficient training [21,22,29]. Addressing these impediments is critical for improving CC prevention and early identification, as well as lowering its impact.
Attitude towards CC/CCS: Four quantitative studies [16,18,26,27] demonstrated that positive attitudes toward CCS significantly facilitate women's participation. Those with a favourable perception and good understanding of CC are more likely to attend CCS.
Embarrassment: Embarrassment due to the intimate nature of VIA/pap smears deterred screening in three quantitative [16,19,24] and one qualitative study [25]. Screening location and privacy also played a significant role in influencing people's willingness to undergo screening, as found in three studies [14].
Concern about the examination technique: Fear of the screening procedure, often linked to the fear of pain, was a common concern in three qualitative [18,25,30] and two quantitative studies [19,24]. Additionally, a study by Lidofsky and colleagues found that fears that the speculum could cause infertility or injury to the bowel add to the barriers in CCS [30].
Experiencing CC signs/symptoms: Experiencing signs and symptoms of CC was found to be a trigger for seeking CCS in three qualitative studies [23,25,30] and one quantitative study [21]. However, the belief that women didn't need to be screened due to being asymptomatic remained an ongoing barrier, even after educational efforts were made [30]. This highlights the complex interplay of factors influencing CCS uptake.
Personal or family experiences with CCS/CC: A quantitative study by Moshi, et al. found that a personal connection or history of CC significantly encourages women to undergo CCS [16]. This link enhances their understanding of CC/CCS, motivating them to prioritize and participate in screening.
Health literacy: Health literacy facilitates CCS among women. In five quantitative studies [15,19,20,24,31], and one qualitative study [30] it was clear that health education and outreach efforts aimed at improving cancer prevention literacy are vital for increasing screening participation. Regular radio and social media users are more likely to attend screenings, underscoring the importance of health communication and education for women's empowerment in CCS.
Age of a woman: In quantitative studies [16,19,20], age was found to be a key factor promoting CCS among women, with the highest attendance rates among those aged 35-49. This suggests that as women get older, they are more likely to participate in CCS, possibly due to increased health awareness as they approach middle age.
Self-Intention to access CCS: Documented by Mboineki, et al. [28], individual motivation to undergo CCS has surfaced as a facilitator, signifying a proactive and self-driven intention among women to participate in CCS.
Multiparity: One study shows that being a multipara can encourage CCS among women [22]. Multipara women with more pregnancies tend to utilize CCS services more often, possibly due to increased health education exposure and greater awareness of the importance of screening related to their reproductive health knowledge.
The number of lifetime sexual partners: In a study conducted by Kileo, et al. [22], an interesting correlation was discovered concerning women's utilization of CCS services. The research indicated that women with a larger number of lifetime sex partners were more likely to utilize CCS services when compared to those with fewer lifetime sex partners.
Quality of life: Perng, et al.'s study suggests that women with lower quality of life scores are more likely to attend CCS [31]. This is because those with lower quality of life may prioritize their health and participate in CCS, making QOL a potential facilitator for screening among this group.
Concern of outcomes or fatality: In two separate qualitative studies [18,25], a prominent barrier to CCS was identified as the fear of receiving a diagnosis of CC, which was frequently coupled with a sense of fatalism regarding the potential prognosis and implications of such a diagnosis. These findings underscore the psychological complexities and emotional factors that play a pivotal role in influencing women's decisions regarding CCS behaviours.
Financial barriers to accessing medical care: In a quantitative study [31], it was found that women who encountered financial barriers to accessing medical care in the past year were more likely to attend CCS services. In a healthcare system where patients are often responsible for purchasing their own supplies, this suggests that women who regularly seek healthcare services may be more accustomed to facing cost barriers. This experience could make them more open to participating in CCS, as they are already accustomed to navigating potential financial obstacles.
B: Cultural and Social Aspects
Discrimination and stigma: Two qualitative studies identified concerns about how CCS was perceived by community members and families as a significant barrier [21,29]. Participants are commonly worried that CCS might inadvertently reveal their HIV status, potentially resulting in societal rejection. In these studies, women expressed concern that their spouses might abandon them if diagnosed with CC, based on unfounded accusations of infidelity [21,29]. These findings highlight the complex social dynamics and stigma associated with CCS within the context of women's lives and relationships.
Lack of social support: Lack of social support can be a significant barrier for CCS among women. This barrier becomes apparent when women are reluctant to visit screening clinics alone, especially when faced with the need to travel long distances for access [15]. The absence of supportive companionship may deter women from seeking CCS services.
Partner involvement: Partner involvement significantly impacts CCS. In two qualitative studies [18,25], men's lack of knowledge about CC until their partners' diagnosis led to misunderstandings and abandonment fears. Well-informed men provided more support, influencing screening utilization, as shown in a quantitative studies [19,22].
Recommendation for CCS: In Mrema, et al.'s study, being recommended to attend screening by HCWs emerged as a significant facilitator [26]. Women who had received such a recommendation were more likely to have undergone CCS compared to their counterparts. This highlights the influential role of HCWs in promoting CCS.
Cancer misconceptions: A study by Henke, et al. [20] revealed that 50% of women in rural areas hold misconceptions about CC, potentially leading to disbelief and neglect of CC prevention measures. Bateman, et al. [25] identified barriers to CCS among HIV-infected Tanzanian women. High misconceptions about screening and fear that diagnosis might be fatal deterred them from seeking healthcare.
Female provider preference: Two qualitative [25,29] and three quantitative [19,24,28] studies highlight the strong preference for female HCWs, which nearly all women express. This preference creates a notable barrier to CCS as women often feel uncomfortable with male doctors and prefer a female nurse's presence during examinations, potentially deterring them from seeking CCS services.
Demographic and Socioeconomic patterns: In quantitative studies, education level [16-19,27,30,32] and formal employment were associated with increased screening [17,19,25], and a monthly income above $65 was linked to stronger screening intentions [16,17,28]. Marital status varies in its impact on CCS, with partnered or married women more likely to undergo screening [17,20,28], while research by Julius and Moshi indicates that being married may predict lower uptake [21]. These findings underscore the influence of marital status on women's CCS engagement.
Religious influence: Religious influence is a powerful factor in promoting CCS among women in Tanzania, as shown in both qualitative [18] and quantitative studies [16]. Leveraging religious networks is crucial in a country where religion plays a central role, fostering trust and increasing women's participation in CCS, making it more accessible and effective.
C: Structural Components
Limited resources/infrastructure: In two qualitative studies [25,29], HCWs identified several challenges hindering their ability to maintain effective daily routines for CCS. These obstacles encompassed low staffing levels, equipment malfunctions, crowded workspaces, and unreliable power supplies. Additionally, another qualitative study highlighted the significant barriers posed by limited financial and human resources in the efforts to increase CCS and treatment [18].
Time constraints and task shifting: Both qualitative and quantitative studies identified task shifting and time constraints as major obstacles to CCS among women [21,32]. Limited space led to extended wait times as HCWs waited for available rooms, causing some patients to leave without getting screened. Overworked HCWs, often operating outside their specialities and enduring long shifts, had limited time for rest, affecting the quality and accessibility of CCS services for women.
HCW qualities: A quantitative study by Kimambo, et al. revealed that HCW attitudes, especially those conducting CCS, significantly impact women's willingness to participate [23]. Nurses are key educators in promoting CCS, and the demeanour of screening personnel influences women's trust and future attendance. Negative perceptions of those conducting screening can be a substantial barrier to women seeking CCS.
Access to CCS: Rural areas present substantial challenges for women seeking CCS, despite their prior knowledge and health insurance [15,30]. Access issues to healthcare facilities providing CCS services can also impact urban residents [19,26].
Lack of motivation among HCWs: Lack of staff motivation, highlighted in one qualitative [25] and one quantitative study [27], is a significant barrier to CCS. When screening is considered an additional task beyond job descriptions, it can diminish HCWs' morale and hinder CCS program efficiency, impacting women's access to CCS.
Donor-dependent funding: One qualitative study identified that depending on foreign donors for funding in the National Cervical Cancer Prevention Program (CECAP) leads to sustainability problems [29]. This, in turn, results in delayed implementation, restricted access to screening services, and a lack of essential tools, ultimately affecting women's ability to access CCS.
Utilizing the health information system (HIS) inefficiently: Mugassa and Frumence [29] noted that the inefficient use of the HIS is a significant barrier to CCS for women due to HCWs' computer illiteracy and inadequate training. This limitation hampers health data management and may impede the provision of CCS services.
Poor collaboration with the private sector: Mugassa and Frumence found that the lack of collaboration between the public and private sectors at the municipal level is a significant barrier to CCS for women [29]. Insufficient planning within the district health system has hindered the establishment of valuable public-private partnerships, limiting the enhancement of CCS services.
Discussion
CCS uptake in Tanzania, as in many other countries, is influenced by a range of barriers and facilitators at multiple levels, including individual, socio-cultural and structural factors. Identifying these barriers and facilitators is essential for designing effective interventions to increase CCS uptake.
Comprehending individual-level barriers and facilitators to CCS is pivotal for developing targeted interventions. A significant obstacle identified in both qualitative and quantitative research was the insufficient knowledge and awareness of CCS [15,16,18-28]. This consistent observation aligns with findings from international studies [33,34], emphasizing the imperative for public health campaigns and educational initiatives. Conversely, positive attitudes and accurate knowledge emerged as robust facilitators for CCS uptake [16,18,26,27]. Mirroring findings from a systematic review in Southeast Asia [35]. It underscores the significance of addressing misconceptions and actively promoting a positive perception of screening to enhance participation in CCS programs.
Personal experiences with CCS [16], health literacy [15,16,20,23,26,27], and maternal age [16,19,20] were identified as facilitators. These align with international reviews [33,35,36] emphasizing the impact of prior exposure and knowledge on screening behaviour. To capitalize on these facilitators and address individual-level barriers, tailored education, awareness, and support are essential. These findings highlight the importance of personalized strategies to enhance engagement and participation in CCS programs.
Concerns about embarrassment [19,21,26,27], fear of the examination procedure [21,23,26,27,29], and misconceptions about CC [15,21] were also noted as barriers, necessitating the need for improving the patient experience and reducing anxiety. Marital status, education and employment status were found to impact CCS participation, illustrating the complex interplay of socioeconomic factors [19,20,28]. Consistent with other reviews [33,35], comprehensive strategies focusing on accessibility, education, and emotional support are crucial for overcoming these challenges and promoting widespread CCS participation.
Our study found the critical role of understanding socio cultural factors in CCS to address stigma and promote social support [21,29]. Additionally, a significant barrier identified was the lack of social support, particularly for women travelling long distances for screening [15], consistent with findings from three other studies [34-36]. Discrimination and stigma related to CCS, particularly in the context of HIV status, emerged as a significant barrier, highlighting the need for community education and reducing stigma.
Partner involvement and recommendations from HCWs were identified as facilitators, emphasizing the role of HCWs and partners in encouraging CCS. Female provider preference [18,21,22,26,27] and the influence of religion [19,29] were also found to affect screening behaviour, underscoring the importance of respecting patient preferences and engaging with religious networks. These findings align with a systematic review conducted in Uganda [33]. The consistency across studies and regions underscores the universal importance of addressing barriers and leveraging facilitators in CCS efforts.
Structural factors play a significant role in shaping CCS access and utilization. Limited resources and infrastructure, including staffing, equipment, and space, pose challenges for HCWs in providing effective CCS services [25]. Task shifting and time constraints result in extended wait times, potentially leading to missed screening opportunities [21,32]. The attitudes and qualities of HCWs conducting CCS were identified as influential, highlighting the need for supportive and well-trained personnel [23]. Access issues [20,23,26,27], especially in rural areas, and donor-dependent funding [29] were identified as structural barriers, emphasizing the importance of improving healthcare infrastructure and sustainability. These findings are consistent with reviews both within and outside Africa [33,35-38], emphasizing the universal need to enhance healthcare infrastructure and promote sustainability for effective CCS programs.
Interventions to enhance CCS uptake should consider addressing individual-level knowledge and attitudes, reducing socio cultural stigma, and improving structural components of healthcare delivery. Tailored strategies that account for the complex interplay of these factors are essential for achieving meaningful progress in CC prevention and early detection in Tanzania.
Strengths and Limitations
This systematic review is the first to focus on barriers and facilitators to CCS uptake among women in Tanzania, offering valuable insights from women, HCWs, and key informants. It has the potential to inform targeted health promotion programs. However, the limited number of studies included restricts an in-depth understanding of district-specific factors, and some barriers or facilitators may have been missed. The studies varied, emphasizing the need for more rigorous, dedicated research on this topic, including improved measurement tools.
Conclusion
This review of CCS in Tanzania reveals a complex interplay of individual, socio-cultural, and structural factors influencing uptake. Key barriers include limited knowledge, stigma, resource constraints, and access issues, while facilitators encompass positive attitudes, social support, and HCW recommendations. To improve CCS participation, interventions must target these multifaceted challenges, emphasizing the importance of education, awareness, and healthcare system strengthening, alongside addressing societal attitudes and cultural dynamics. A holistic approach that considers the diverse factors at play is essential to advance CC prevention and early detection in Tanzania.
Acknowledge
No acknowledgments to declare.
Conflict of Interest
All authors declared no conflict of interest.
Funding Source
No funds received in this study.
Statement of Protocol Availability
The review was conducted without a formal protocol; however, the study design followed established guidelines, including PRISMA, and adhered to criteria outlined by Sirriyeh and colleagues for assessing the quality of the included studies.
References
- Small W, Bacon MA, Bajaj A, et al. (2017) Cervical cancer: A global health crisis. Cancer 123: 2404-2412.
- Zhang S, Xu H, Zhang L, et al. (2020) Cervical cancer: Epidemiology, risk factors and screening. Chin J Cancer Res 32: 720-728.
- Sung H, Ferlay J, Siegel RL, et al. (2021) Global cancer statistics 2020: Globocan estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71: 209-249.
- Thun MJ, DeLancey JO, Center MM, et al. (2010) The global burden of cancer: priorities for prevention. Carcinogenesis 31: 100-110.
- GROBOCAN (2022) cervical cancer - Google Search.
- Bruni L, Diaz M, Castellsagué M, et al. (2010) Cervical human papillomavirus prevalence in 5 continents: Meta-analysis of 1 million women with normal cytological findings. J Infect Dis 202: 1789-1799.
- IARC/WHO (2021) Tanzania human papillomavirus and related cancers, fact sheet 2021. ICO/IARC HPV Information Centre. Barcelona, Spain.
- Catalan Institute of Oncology (ICO) Information Centre on HPV and Cancer (HPV Information Centre). Human Papillomavirus and Related Diseases Report.
- World Health Organization (WHO) (2020) Cervical cancer 2019: Early diagnosis and screening of cancer.
- Mremi A, Mchome B, Mlay J, et al. (2022) Performance of HPV testing, Pap smear and VIA in women attending cervical cancer screening in Kilimanjaro region, Northern Tanzania: A cross-sectional study nested in a cohort. BMJ Open 12: e064321.
- Campos NG, Sharma M, Clark A, et al. (2016) Resources required for cervical cancer prevention in low- and middle-income countries. PLoS One 11: e0164000.
- Page MJ, McKenzie JE, Bossuyt PM, et al. (2021) The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 372: n71.
- Sirriyeh R, Lawton R, Gardner P, et al. (2012) Reviewing studies with diverse designs: The development and evaluation of a new tool. J Eval Clin Pract 18: 746-752.
- Peng Z, Wang S, Xu B, et al. (2017) Barriers and enablers of the prevention of mother-to-child transmission of HIV/AIDS program in China: A systematic review and policy implications. Int J Infect Dis 55: 72-80.
- Cunningham MS, Skrastins E, Fitzpatrick R, et al. (2015) Cervical cancer screening and HPV vaccine acceptability among rural and urban women in Kilimanjaro Region, Tanzania. BMJ Open 5: e005828.
- Moshi F, Bago M, Ntwenya J, et al. (2019) uptake of cervical cancer screening services and its association with cervical cancer awareness and knowledge among women of reproductive age in Dodoma, Tanzania: A Cross-Sectional Study. East Afr Health Res J 3: 105-115.
- Weng Q, Jiang J, Haji FM, et al. (2020) Women’s knowledge of and attitudes toward cervical cancer and cervical cancer screening in Zanzibar, Tanzania: A cross-sectional study. BMC Cancer 20: 63.
- McCree R, Giattas MR, Sahasrabuddhe VV, et al. (2015) Expanding cervical cancer screening and treatment in Tanzania: Stakeholders’ perceptions of structural influences on scale-up. Oncologist 20: 621-626.
- Lyimo FS, Beran TN (2012) Demographic, knowledge, attitudinal, and accessibility factors associated with uptake of cervical cancer screening among women in a rural district of Tanzania: Three public policy implications. BMC Public Health 12: 22.
- Henke A, Kluge U, Borde T, et al. (2021) Tanzanian women´s knowledge about Cervical Cancer and HPV and their prevalence of positive VIA cervical screening results. Data from a prevention and awareness campaign in Northern Tanzania, 2017-2019. Glob Health Action 14: 1852780.
- Julius M, Moshi FV (2019) Predictors influencing uptake of cervical cancer screening among women of reproductive age in Mara region.
- Kileo NM, Michael D, Neke NM, et al. (2015) Utilization of cervical cancer screening services and its associated factors among primary school teachers in Ilala Municipality, Dar es Salaam, Tanzania. BMC Health Serv Res 15: 552.
- Kimambo E, Mohamed N, Mikheal I (2023) Women’s knowledge, attitude and practice regarding cervical cancer screening in Mbeya Region-Tanzania. Alexandria Scientific Nursing Journal 25: 113-125.
- Koneru A, Jolly PE, Blakemore S, et al. (2017) Acceptance of peer navigators to reduce barriers to cervical cancer screening and treatment among women with HIV infection in Tanzania. Int J Gynaecol Obstet 138: 53-61.
- Bateman LB, Blakemore S, Koneru A, et al. (2019) Barriers and facilitators to cervical cancer screening, diagnosis, follow-up care and treatment: perspectives of human immunodeficiency virus-positive women and health care practitioners in Tanzania. The Oncologist 24: 69-75.
- Mrema D, Ngocho JS, Mremi A, et al. (2023) Cervical cancer in northern Tanzania-What do women living with HIV know. Front Oncol 9: 12.
- Theophil T, Balandya B, Kunambi P, et al. (2022) Knowledge, utilization, challenges and factors associated with cervical cancer screening among female doctors and nurses at a tertiary hospital in Tanzania: A cross sectional study.
- Mboineki JF, Wang P, Dhakal K, et al. (2020) Predictors of uptake of cervical cancer screening among women in Urban Tanzania: Community-based cross-sectional study. Int J Public Health 65: 1593-1602.
- Mugassa AM, Frumence G. (2019) Factors influencing the uptake of cervical cancer screening services in Tanzania: A health system perspective from national and district levels. Nurs Open 7: 345-354.
- Lidofsky A, Miller A, Jorgensen J, et al. (2019) Development and implementation of a culturally appropriate education program to increase cervical cancer screening among Maasai women in rural Tanzania. Ann Glob Health 85: 127.
- Perng P, Perng W, Ngoma T, et al. (2013) Promoters of and barriers to cervical cancer screening in a rural setting in Tanzania. Int J Gynaecol Obstet 123: 221-225.
- Mrema JD, Elisaria E, Mwanri AW, et al. (2021) Prevalence and determinants of under nutrition among 6- to 59-months-old children in lowland and highland areas in Kilosa District, Tanzania: A Cross-Sectional Study. J Nutr Metab 2021: 6627557.
- Black E, Hyslop F, Richmond R (2019) Barriers and facilitators to uptake of cervical cancer screening among women in Uganda: A systematic review. BMC Women’s Health 19: 108.
- Kirubarajan A, Leung S, Li X, et al. (2021) Barriers and facilitators for cervical cancer screening among adolescents and young people: A systematic review. BMC Women’s Health 21: 22.
- Chua B, Ma V, Asjes C, et al. (2021) Barriers to and facilitators of cervical cancer screening among women in Southeast Asia: A systematic review. Int J Environ Res Public Health 18: 4586.
- Driscoll SD (2016) Barriers and facilitators to cervical cancer screening in high incidence populations: A synthesis of qualitative evidence. Women Health 56: 448-467.
- Lim JNW, Ojo AA (2017) Barriers to utilisation of cervical cancer screening in Sub Sahara Africa: A systematic review. Eur J Cancer Care (Engl) 26: e12444.
- Robbers GML, Bennett LR, Spagnoletti BRM, et al. (2021) Facilitators and barriers for the delivery and uptake of cervical cancer screening in Indonesia: A scoping review. Global Health Action 14: 1979280.
Corresponding Author
Magnus Michael Sichalwe, Family Welfare, Primary Health and Preventive Services (FWPPS) Organization and Butiama District Hospital, P.O Box 628 Bambalawe St Morogoro, Tanzania, Tel: +255624948474.
Copyright
© 2024 Sichalwe MM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.