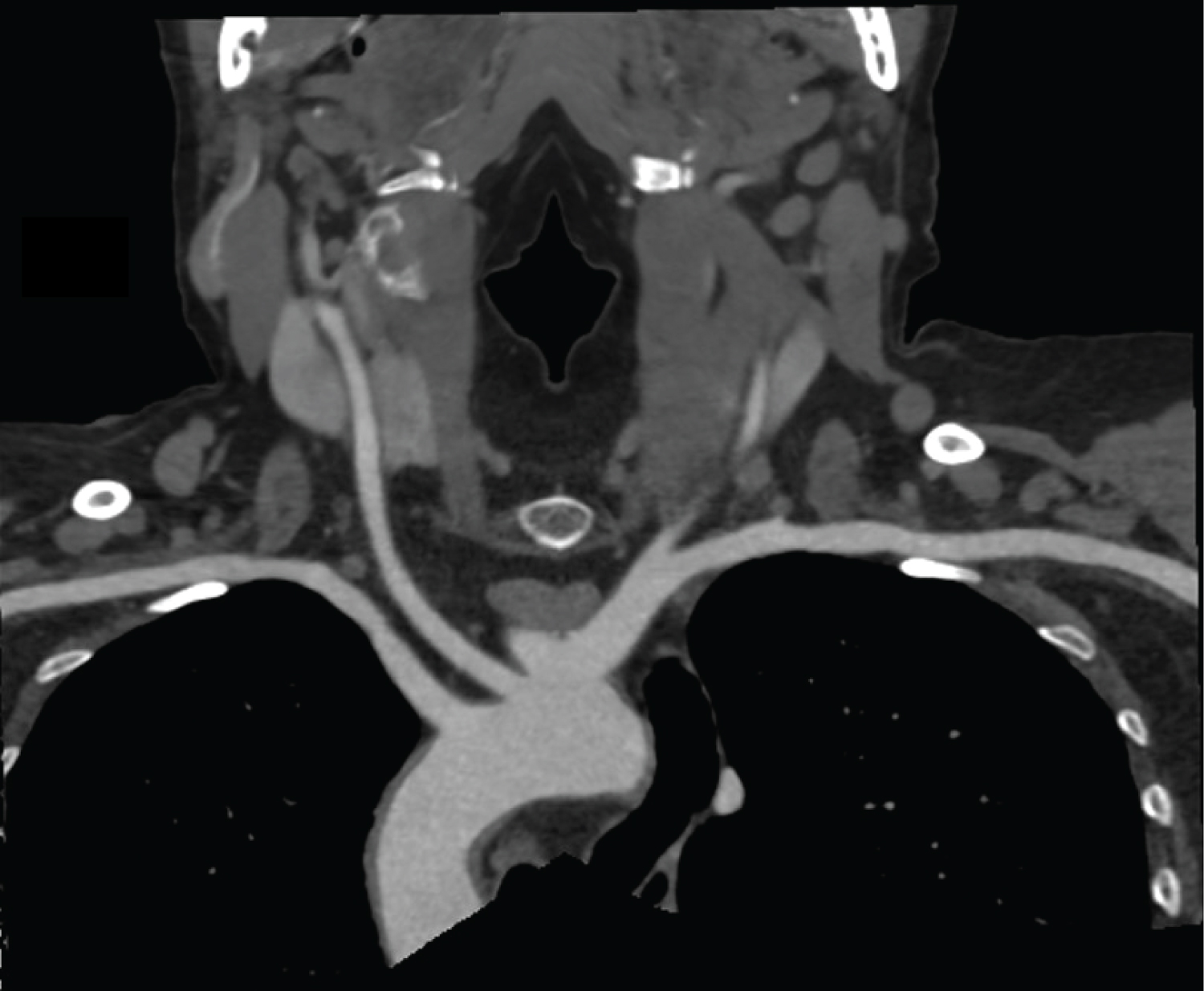
Bilateral Subclavian CT Angiography via Lower Limb Contrast Injection
Abstract
After a review of the relevant literature a novel injection protocol for CT Angiography (CTA) of the bilateral subclavian arteries is proposed. Images illustrating the use of this method are presented and a discussion of the existing methods and the novel alternative is provided.
Keywords
CT Angiography, Bilateral, Subclavian, Lower limb injection.
Introduction
The protocol for unilateral CTA of the upper limb is well documented. The advantage of CTA is that it provides a non-invasive method of reliably identifying anatomical variants and pathologies of the arteries. Bilateral subclavian artery CTA is inherently more difficult due to hyper dense venous iodine contrast causing artefact in the scan plane.
The accepted means of avoiding this in-plane artefact is injection via a central venous line. This may be in the form of a Peripherally Inserted Central Catheter (PICC), A Central Venous Catheter (CVC) or an Infusa Port. The insertion of these lines is invasive. They may be utilised if they are labelled as CT pressure rated and already in situ but inserting such a line for the purpose of conducting CTA adds an unfortunate risk and complexity to an otherwise simple procedure.
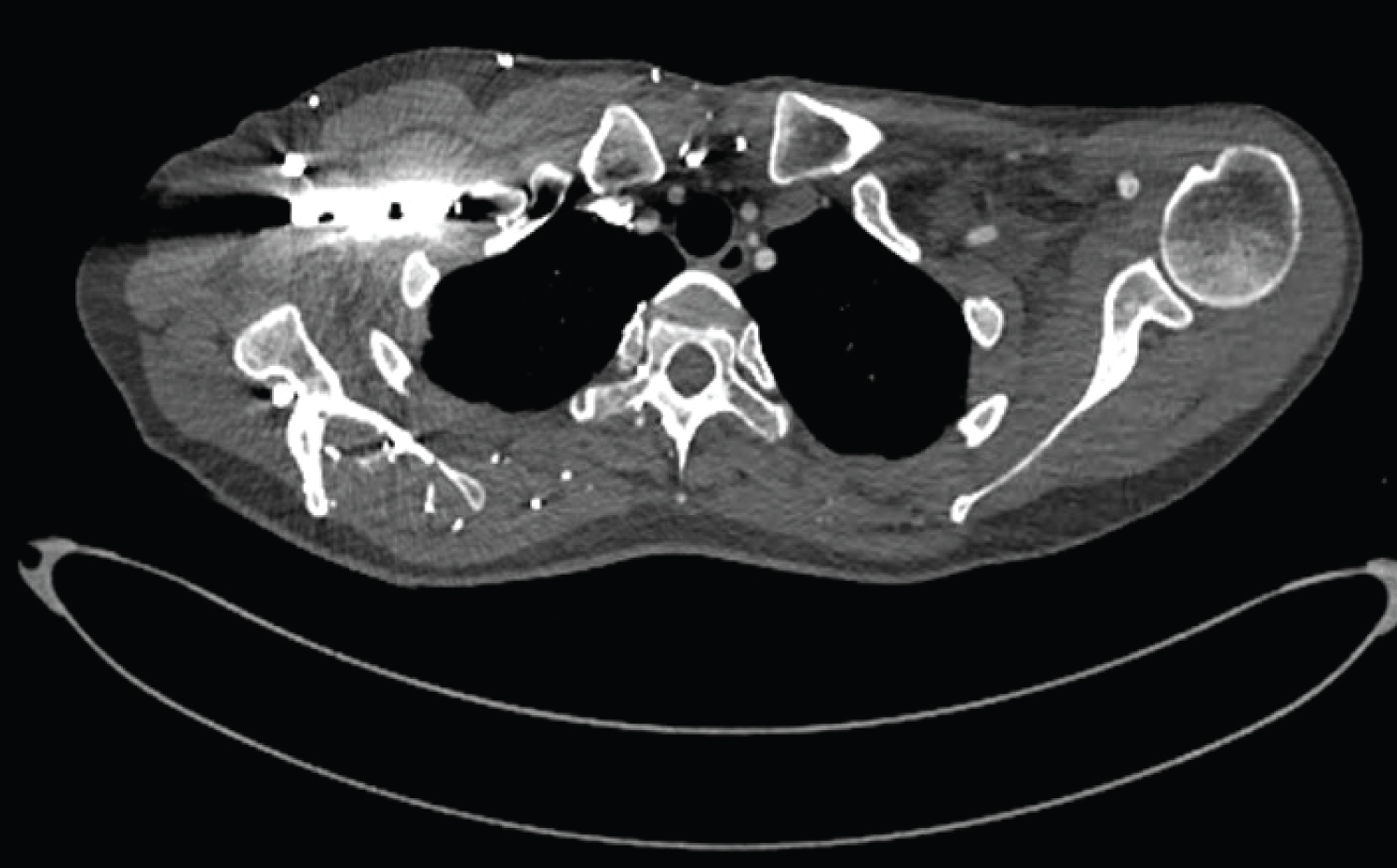
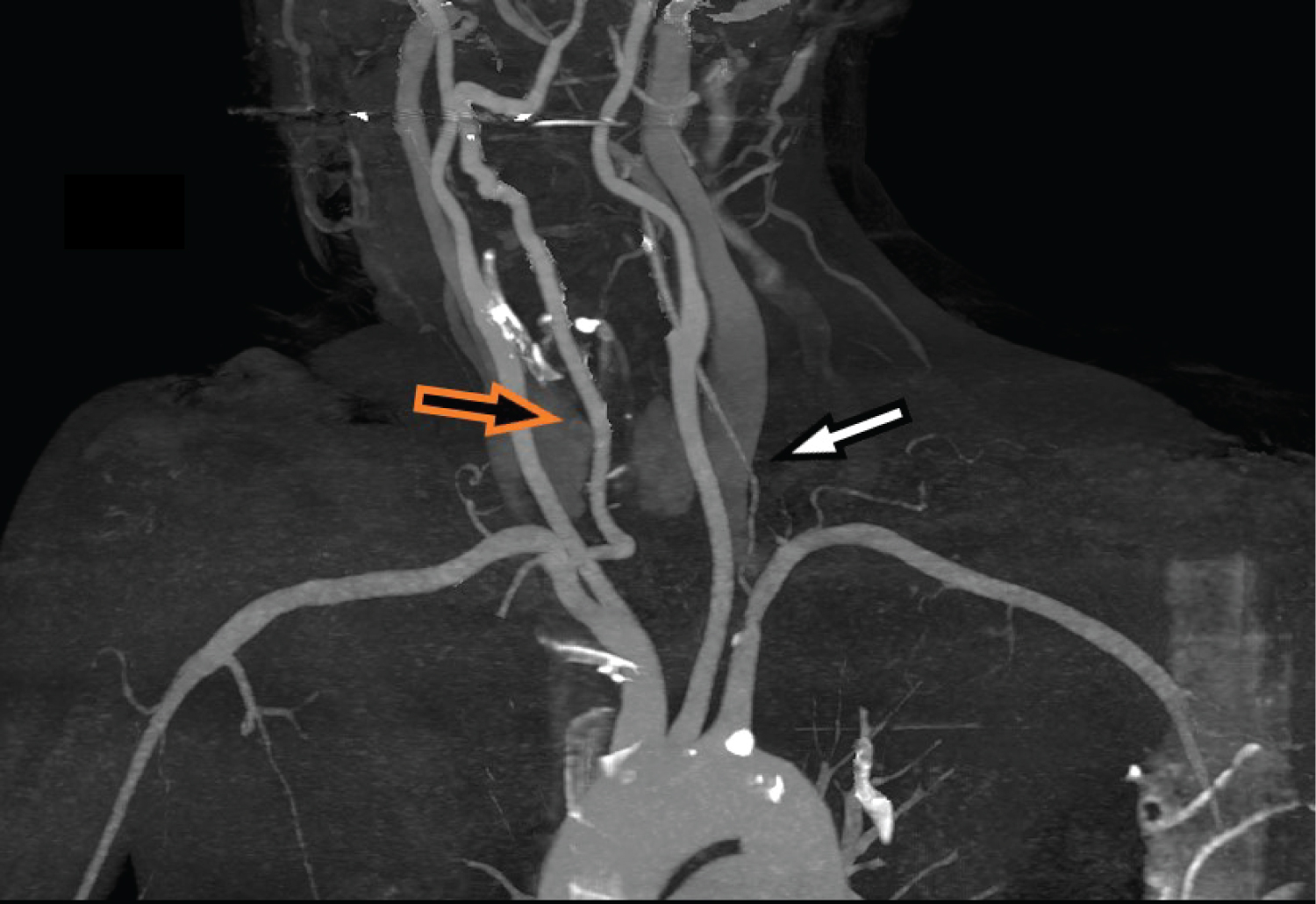
In an attempt to obtain artefact free bilateral subclavian CTA in patients who do not have a Central Venous line in situ the lower limb has been used as an injection site with good effect.
Anatomy and pathology
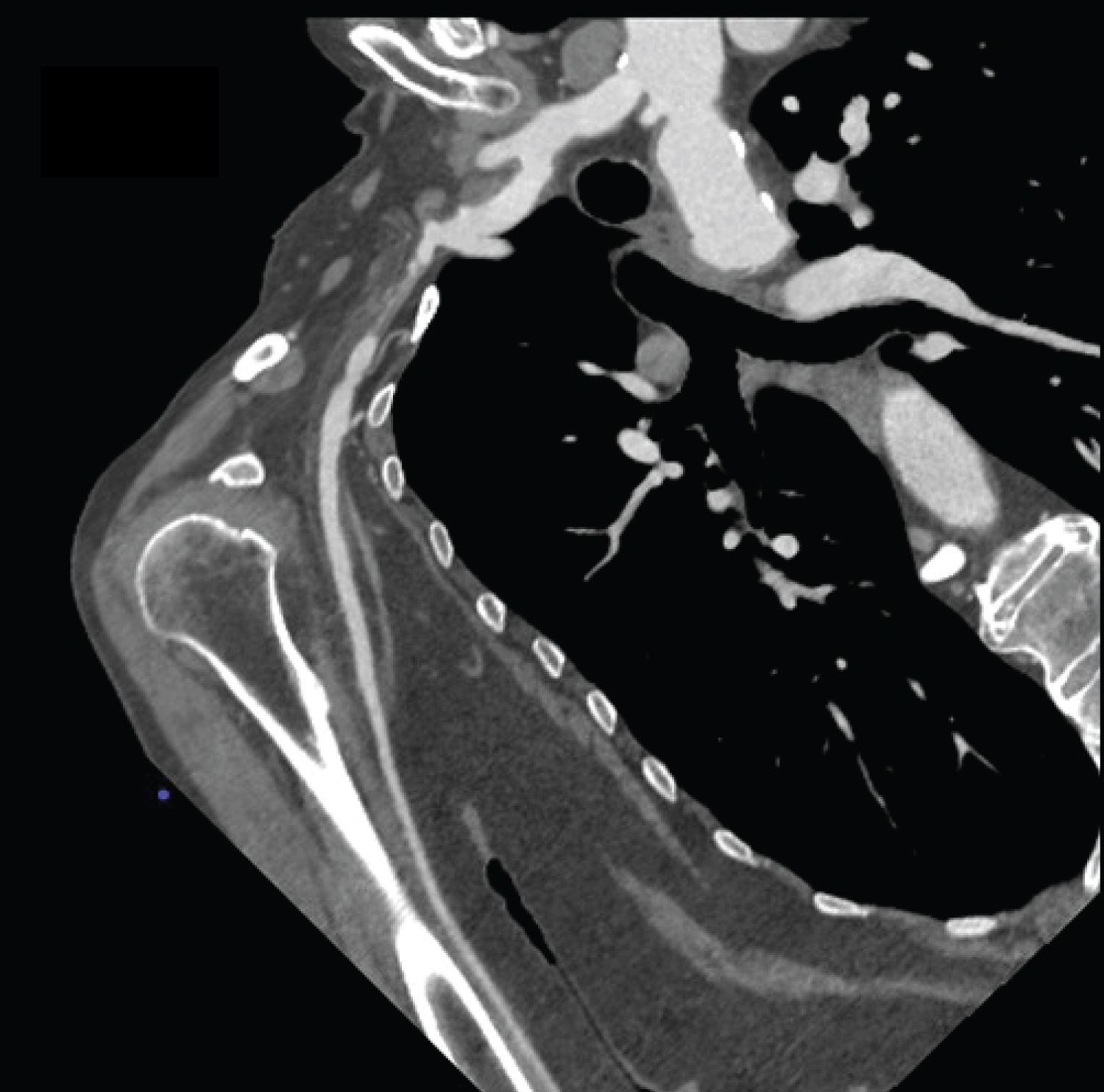
The anatomy of the subject region is relatively uncomplicated. On the right the brachiocephalic artery arises from the aortic arch and divides into the right subclavian and right carotid arteries. On the left the carotid and subclavian arteries arise separately, the subclavian artery arising posteriorly. The vertebral arteries arise from the subclavian arteries with the right vertebral artery dividing from the subclavian artery slightly distal to the bifurcation of the carotid artery from the brachiocephalic artery.
In an acute setting unilateral CTA of the entire upper limb is usually more appropriate [1] and requires an entirely different technique which is not discussed here. In the non-acute setting subclavian artery CTA is commonly requested for asymmetry of blood pressure, unilateral limb weakness, claudication, and syncope when lifting and using an upper limb.
A blood pressure differential of greater than 10mm/Hg can suggest cardiovascular disease [2]. A differential of 15mm/Hg or greater [3] suggests subclavian artery stenosis on the side where the pressure is low. Similarly in the absence of a clear neurological cause, claudication and limb weakness can suggest a reduced arterial supply. Syncope can occur if there is severe stenosis or obstruction between the origin of the subclavian artery and the vertebral artery. This phenomenon is known as a "subclavian steal" and is caused by reversal of the direction of flow in the vertebral artery on the symptomatic side. Due to the difference in anatomy between the two sides this occurs on the left in 66.7% of cases [3].
While an obstruction can be easily identified with unilateral CTA, stenosis can be difficult to interpret without comparison between both arteries. The path of the subclavian arteries passes close to bony structures which can have an impact on their CT angiographic appearance. Comparison between sides is helpful in identifying stenoses. In our department these non acute cases are often first investigations so bilateral CTA is appropriate.
Equipment
Over time this examination has been performed using two different CT machine/injector configurations. The first was a Siemens Definition AS 64 (Erlangen, Germany) paired with a Salient single syringe manually triggered contrast injector (Hannover, Germany). This machine was in use from April 2010 to February 2020. In March 2020 a Siemens Go. Top (Erlangen, Germany) was installed and paired with a Salient dual syringe contrast injector (Hannover, Germany). In February of 2021 the injection tubing was switched to the Tran flux system (Radiology, New Zealand).
Omnipaque 350(GE Healthcare) and normal saline, via the dual syringe system only, were injected via a Surflash (Tokyo Japan) 20g x 32mm IV cannula.
Method
In accordance with department policy the patient's compatibility with the examination is checked. This includes radiation safety issues like their pregnancy status and previous imaging history. Anecdotally most of the patients examined in our department who require subclavian artery angiography are past a reproductive age. A contrast safety and consent form is used to consistently assess suitability for injection of contrast media and a General Chemistry blood test result from the last 3 months used to check renal function.
After the examination is explained clearly to the patient and consent obtained they sit on the side of the scan table. The table is raised so the foot and ankle are at a comfortable height for cannulation by a seated operator. A tourniquet is applied above the malleoli and the dorsum of the foot and anterior ankle are inspected for a suitable, engorged vein. Wearing gloves and having cleaned the skin surface with an appropriate swab the vein is cannulated and a high flow rate connector applied to the cannula hub. The cannula position and flow rate are checked by flushing with 10ml of normal saline and it is secured with a transparent film dressing.
Once suitable IV access has been secured the patient is positioned head first on the scan table with their arms close by their sides. The CT machines used have suitable arm supports provided as part of the accessory pack. The patient's legs are elevated using a combination of the supplied knee support accessory and pillows. The patient is warned to expect breathing instructions and the usual warmth and smell or taste sensations associated with iodinated contrast injection.
A scanogram is performed and a pre-monitoring scan obtained through the level of the aortic arch. A region of interest cursor is positioned in the ascending aorta and a trigger value of 100HU is set. Following the injection of a suitable volume of contrast delivered at a rate of 4ml/s or greater the patient is scanned from the base of the neck to the level of the elbow. The patient is then asked to wait under observation for 20 minutes in case of post injection reaction and sent home. The images are assessed for anatomical coverage, image noise and adequate opacification. A HU value of 200 or greater [1] is considered acceptable. The acquired data is processed according to practice protocol like other CTA examinations and reported by the duty radiologist.
Discussion
There are few differences between this novel approach and the conventional technique. Essentially the injection site, the volume of contrast used and the timing of the acquisition are the important considerations. It is not the author's intent to teach CTA technique, only to propose an alternative and a guide to how it may be implemented. Certainly the technique described here reduces both the contrast and radiation doses of examining the subclavian arteries unilaterally in succession.
As stated in the preceding section the dorsum of the foot or ankle is the usual site for venous access although in one case, with the help of a radiologist, the great saphenous vein was cannulated under ultrasound guidance. The seated position described above significantly increases the volume of the leg and foot veins by virtue of the impact gravity has on fluid dynamics. This aids in identifying and cannulating an appropriate vessel. As a rapid bolus is required for any CTA a 20g cannula is routinely used to obtain adequate opacification, particularly when the contrast is being delivered to a vein distant from the heart. If possible, an 18g cannula and increased injection rate are recommended.
While a tourniquet is typically applied to a single bone location, above the elbow, to increase venous compression when cannulating at the ante cubital fossa or distally, this may not be an effective technique in the lower limb. The path of the popliteal vein and thickness of the surrounding tissue protect it from compression by a tourniquet so application proximal to the malleoli has proved to be an effective option.
The use of an upper limb vein to deliver intravenous contrast is very well established and technologists trained in CTA techniques are very familiar with the volume and timing needed to achieve adequate opacification of the arteries to be examined. Effectively the volume needs to be that which will provide good opacification in the artery for the entirety of the scan time. The volume of the veins between the injection site and the heart is quite small and so the patient's size should be considered but does not have a great impact on opacification.
Injection into a lower limb requires more consideration. The volume of the veins in the leg and vena cava is far greater and dilution of the contrast bolus is a factor which must be taken into account [4]. Experience within our department has suggested a portal venous abdomen contrast volume of 1ml/kg is effective and increasing that by 20% (1.2ml/kg) is a well judged minimum for lower limb injection CTA. A normal saline bolus of 60ml at 4ml/s to "push" the contrast minimises the dose of iodinated material required to maintain opacification for the entirety of the scan. Elevation of the lower limbs should help rapid flow of the contrast to the heart and minimise dilution of the contrast by the greater blood volume. There is an argument for the application of a tourniquet at the level of the femoral condyles to reduce peripheral vein filling and increase contrast flow directly into the popliteal vein however this addition to the technique has not been used in our department.
The tyranny of distance inherent in this technique has an effect on scan timing. Monitoring the HU value of the aorta provides a trigger point for commencing the scan but each monitoring scan increases the patient's radiation dose minutely. It is important therefore to estimate with some accuracy the point at which aortic arch opacification is likely to occur and commence monitoring shortly beforehand. This minimises the number of monitoring scans performed and thus, reduces unnecessary exposures.
The Trans-flux tubing system used in our department requires the patient line to be saline filled. At 4ml/s this adds approximately 2 seconds to the scan trigger time. An upper limb contrast injection monitoring delay of 12 seconds reliably minimises the number of monitoring scans performed without missing the start of the opacification window. Lower limb injection adds to this delay by between 5 and 10 seconds depending on cardiac output, age, height and a number of other factors. In order to reduce the risk of error and optimise contrast density a monitoring delay of 20 seconds is used with a region of interest cursor positioned in the ascending aorta. Similarly a test bolus technique could be used however there is concern that the volume of contrast required to avoid dilution would be excessive.
The primary advantage of this approach is to avoid beam hardening artefact from hyper dense venous contrast in the subclavian vein and superior vena cava [4]. It also provides an alternative injection site for patients who are at increased risk of upper limb lymphodema. Consideration should be given to the disadvantages and contraindications of this technique so as to do no harm. As previously mentioned above, timing and dilution of the contrast are hurdles but the method outlined manages these challenges effectively. Aside from the well established contraindications of contrast allergy and renal impairment the condition of the lower limb is a factor.
Venous pathology in the lower limb can decrease the patient's suitability for this procedure. Deep vein thrombosis (DVT) is dramatically more common in the lower limb than in the upper limb [5] and may prevent cannulation and/or flow of contrast via the deep veins to the vena cava. Collateral drainage of the peripheral veins around a DVT will not supply contrast to the heart with the efficiency needed to obtain adequate opacification of the subclavian arteries. Cellulites occur more commonly in the lower limb [6] and increases systemic infection risk from the injection site. Both cellulites and oedema may make cannulation of the lower limb impractical.
Conclusion
With a few minor changes to the accepted practice outlined in the literature this technique allows incoming contrast artefact to be avoided in bilateral subclavian CTA without the use of a central venous line. Compared to scanning the subclavian arteries twice, once per side, the risks associated with x-radiation and contrast dose are inherently lower. The approach described facilitates anatomical comparison providing increased confidence for the reporting radiologist. All of the examinations performed this way in our department have proved to be of diagnostic quality and there have been no extravasations or injuries to veins.
References
- Bozlar Ugur, Torel Ogur, Patrick T Norton, et al. (2022) CT Angiography of the upper extremity arterial system: Part 1-Anatomy, technique, and use in trauma patients. Am J of Roentgenol 201:745-752.
- Shadman R, Criqui M, Bundens W, et al. (2022) Subclavian artery stenosis: Prevalence, risk factors, and association with cardiovascular diseases. J Am Coll Cardiol 44: 618-623.
- Foucheres G, Maigret P, Elias-Billon I, et al. (2015) CO-31: Prevalence of asymmetrical blood pressure in uncontrolled hypertensive patients is high and highly related with cardiovascular diseases prevalence. Annales de Cardiologie et d'Angéiologie 64: S15.
- Ghouri M, Gupta N, Bhat A, et al. (2019) CT and MR imaging of the upper extremity vasculature: Pearls, pitfalls, and challenges. Cardiovasc Diagn Ther 9(S1) S152-S173.
- Ageno W, Haas S, Weitz J, et al. (2019) Upper extremity DVT versus lower extremity DVT: Perspectives from the GARFIELD-VTE Registry. Thromb Haemost 119: 1365-1372.
- Brown B, Watson K, (2022) Cellulitis.
Corresponding Author
Kim Smith, Radiology SA, Central Districts Hospital, Elizabeth Vale South Australia 5116, Australia
Copyright
© 2022 Smith K. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.