Effect of Vitamin D Supplementation on Clinical and Radiographic Evaluation of Oral Rehabilitation with Osseointegrated Implants
Abstract
Vitamin D (VD) is important for the development and maintenance of bone tissue. This study used clinical and radiographic evaluations to analyze whether insufficient VD levels affect the peri-implant health of patients with implant-supported prostheses. Data were collected for 33 patients with implant-supported prostheses: Probing depth (PD); width of keratinized mucosa (wKM); bleeding (mBI); peri-implant plaque index (mPI); distance from implant to bone crest and VD level. Patients with levels under 30 ng/ml at baseline received 50000 IU of VD per week for 8 weeks (post-treatment, PT), when clinical and radiographic evaluations were repeated for the control (n = 19) and the VD (n = 14) groups. Clinical and radiographic results were compared at baseline and at PT. There were differences in PD (p = 0.0247) and distance from implant to bone crest (p < 0.0001), but there were not statistically different after supplementation. wKM, mBI and mPI were not statistically different between groups. VD levels were 24.95 ± 0.96 ng/mL in the VD group (42.42% of patients), whereas 57.57% of all participants had a mean VD value of 40.99 ± 1.23 ng/mL, a statistically significant difference (p = 0.0034). According to clinical and radiographic findings, VD serum levels do not seem to affect peri-implant health.
Keywords
Bone density, Clinical study, Dental implantation, Vitamin D
Introduction
Vitamin D (VD) is known for its role in bone development and maintenance, as well as in calcium and phosphorus homeostasis [1]. A decrease in the VD levels leads to a reduction of its absorption in the intestines and hypocalcemia. In this condition, calcium homeostasis is a result of secondary hyperparathyroidism, as bone calcium mobilization increases and calcium renal clearance decreases. At the same time, the intestinal absorption of phosphate is reduced, which results in hypophosphatemia [2].
Mineralization is the physiological process of calcium and phosphorus deposition on the organic matrix after osteoblasts have synthesized and formed this matrix. Adequate amounts of calcium and phosphorus have to be available for normal mineralization. In cases of hypocalcemia or hypophosphatemia, if osteoblasts continue producing bone matrix that is not adequately mineralized, bone repair may not occur, and rickets in children, as well as osteomalacia in adults, may develop. VD insufficiency is inversely correlated with parathyroid hormone and carboxyl-terminal telopeptide (CTX), a marker of bone resorption [3]. Estimates suggest that about one billion people in the world have vitamin D deficiency or insufficiency [1].
The Endocrine Society guidelines define that the levels of 25(OH) VD are deficient when below 20 ng/mL, insufficient when between 21 and 29 ng/mL and sufficient when above 30 ng/mL. Supplementation should be 50,000 IU a week for eight weeks in cases of deficiency in adults [4].
Osseointegration, that is, bone repair around implants, has been defined as direct bone anchorage to titanium implants, capable of resisting masticatory loads [5,6]. Treatment success is defined by the evaluation of implant at bone level, peri-implant tissues, prosthetics and patient satisfaction [7,8]. Physiological success, assessed by measuring the position of the bone crest in relation to the cervical border of the implant, is defined as bone loss below 1.5 mm in the first year and up to 0.2 mm in subsequent years. Peri-implant success has been evaluated using probing depth, suppuration, bleeding, edema, plaque index, width of keratinized peri-implant mucosa, mobility and infection [8].
Few clinical studies have focused on osseointegrated implants and the important role of VD. This study investigated whether VD deficiency affects peri-implant clinical and radiographic findings at treatment follow-up, and whether full doses of VD supplementation may improve prognosis.
Methods
Participant selection
This cross-sectional study was approved by the Ethics and Research Committee of the institution where it was conducted and registered in the Brazilian Ethics in Research System (SISNEP) under no. 202/2012.
Patients that received treatment with osseointegrated tooth implants in 2011- 2013 were recruited in the Dental Clinics of State University of West Parana-Unioeste, in the city of Cascavel, Brazil.
Inclusion criteria were: Age 35 to 60 years; bothmen and women; adequate oral hygiene; single or multiple implant-supported prosthesis in use for mastication for at least six months; no periodontal disease.
The minimum age of 35 years was defined to make sure that bone mass peak had already been reached. Maximum age of 60 was defined to reduce chances of recruiting individuals with senile osteoporosis. Exclusion criteria were: Osteoporosis under treatment; diseases, such as primary hypogonadism, primary hyperparathyroidism, current hyperthyroidism, Cushing syndrome, hyperprolactinemia, anorexia nervosa, osteomalacia, rheumatoid arthritis, chronic obstructive pulmonary disease, cancer, Marfan's syndrome, Ehler-Danlos syndrome, homocystinuria, diabetes; continuous use ofcorticosteroids, thyroxin, anticonvulsants, lithium, alendronate,methotrexate; pregnancy.
Patients were selected according to their medical records in the Dental Clinic Institute of Unioeste. Patients were invited to participate, received information about the study, its risks and benefits and signed an informed consent term.
Clinical procedures
Titanium frictional dental implants (Kopp System, Curitiba, Parana, Brazil), measuring 3.75 mm in diameter and 8, 9 or 11 mm long, were placed under local anesthesia by one surgeon in a single intervention. The implants were placed after raising a full-thickness mucoperiosteal flap. The implant site preparation was performed according to the protocol of the system and primary stability was always achieved. The implants were placed 1 to 2 mm below the bone crest. After one week, the sutures were removed and postoperative control was performed.
Temporary restorations were maintained for a period of 2 months, in order to monitor the peri-implant tissues and masticatory load and were replaced with final restorations made of metal porcelain.
Data Collection
Clinical analysis
Two examiners were calibrated for clinical analysis. Data collected were statistically analyzed to detect method error and intra- and interexaminer agreement. Probing depth (PD): Intraexaminer error p (bilateral) = 0.1133; interexaminer error p (bilateral) = 0.0976; modified sulcus bleeding index (mBI): Intraexaminer error (Wilcoxon) p (bilateral) = 0.7532; interexaminer error p (bilateral) = 0.3739; Width of keratinized mucosa (wKM): Intraexaminer error p (bilateral) = 1.000; interexaminer error p (bilateral) = 1.000; modified plaque index (mPI): Intraexaminer error (Wilcoxon) p (bilateral) = 0.3137; interexaminer error p (bilateral) = 0.3137.
A one-millimeter implant probe (PCV12KIT6 Colorvue) was used to assess peri-implant tissue health and disease and determine peri-implant indices, such as: 1) PD: Depth of peri-implant sulcus measured from the free gingival margin to the deepest point of the sulcus; 2) wKM: Width of gingiva inserted in the buccal surfaces of implants, measured in millimeters from the free gingival margin to the border of the free gingiva. Measures were made for the mesial, distal, lingual and buccal surfaces of all implants; 3) mBI: 0 = no bleeding; 1 = isolated bleeding spots; 2 = bleeding formed a confluent red line on the gingival margin; 3 = heavy or profuse bleeding. Bleeding was measured at the buccal, medial and distal surfaces of all implants and 4) mPI: 0 = no plaque; 1 = plaque on implant margin; and 2 = plaque visible to the naked eye. Plaque was scored on the buccal, lingual, mesial and distal surfaces of all implants [9]. Peri-implant tissues were examined at baseline and after treatment (PT).
Participants were instructed to keep oral hygiene practices using the modified Bass technique from baseline to clinical reexamination [10].
Radiographic analysis
All participants underwent radiographic evaluations, and the images were digitalized by technicians in the Oral Diagnose radiology clinic (CNPJ: 03.645.515/0007-22). A Gnatus X-ray unit and a digital imaging system (Digora-Optime, Soredex, Joinville, Brazil) were used with a positioner to ensure standardization. The areas of image distortion, structure overlapping and other artifacts were removed, and the best images were selected for the measurement of distances from the bone crest to the implant and for the counting of cancellous pixels at baseline. The same measurements were made at PT.
The Image J 1.48 (Wayne Rasband, National Institute of Health, USA) was used to measure the distance between implant cervical area, where the post was placed, and the mesial and distal bone crest.
Chemical analysis
Blood samples were collected to measure 25(OH) VD using chemiluminescence in a clinical analysis laboratory (Álvaro, corporate taxpayer number in Brazil [CNPJ]: 61.486.650/0284-36). Patients with less than 30 ng/mL were included in the VD insufficiency group and received free vitamin supplementation with eight 50,000-IU VD capsules dispensed by a manipulation drugstore (Chamomilla, CNPJ 01.983.404/0001-05) and administered once a week as prescribed [11]. After that, post-treatment clinical and radiographic evaluations were conducted.
Statistical analysis
After normal distribution was tested, ANOVA and the Tukey test were used to determine differences between the VD and the control groups, and the Kruskal-Wallis test was used to analyze data in the control and the VD groups and determine differences in the same period of time. Prism 5.0 (GraphPad) was the software used for all calculations. The level of statistical significance was set at p < 0.05.
Results
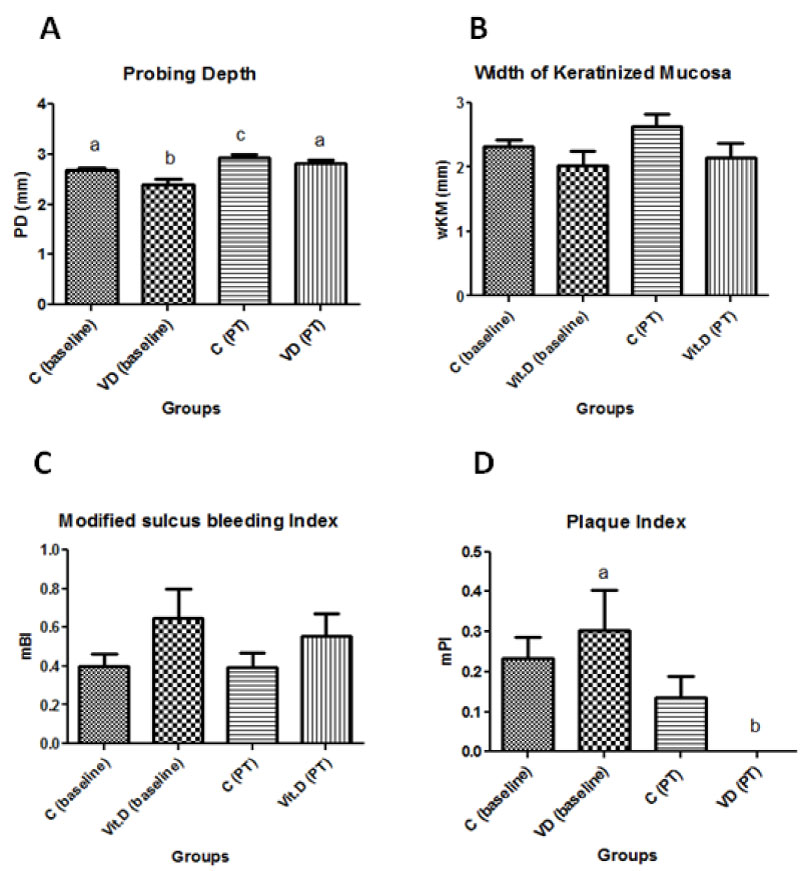
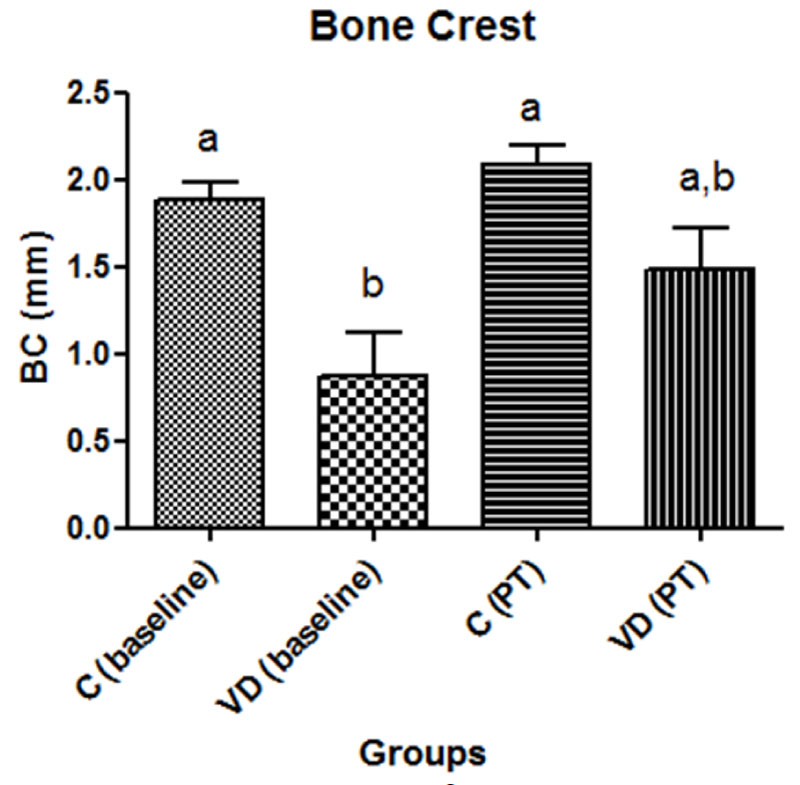
The characteristics of patients with sufficient and insufficient levels of vitamin D are shown in Table 1. Peri-implant parameters are described in Figure 1 and Figure 2. No statistically significant differences were found in mean width of keratinized mucosa (wKM), modified sulcus bleeding index and modified plaque index in the control and VD deficiency groups at baseline and after treatment (ANOVA and Tukey test; p > 0.05).The results of mean probing depth (PD) and mean distance from bone crest to implant cervical area in the control and vitamin D deficiency groups at baseline and after treatment (PT) are shown in Figure 1A and Figure 2.
Discussion
Vitamin D levels in the blood of a population vary according to age, eating habits, use of sunscreen, seasonality, geography and cultural and genetic factors [3]. The inclusion criteria in this study, however, defined unique population characteristics, as participant age was narrowly limited, and participants were all from the same geographic region and had similar social and cultural backgrounds, which precluded statistical correlations with findings in other studies.
Peri-implant success was evaluated using probing depth, suppuration, bleeding, edema, plaque index, width of keratinized peri-implant mucosa, mobility and infection [8]. In a study with peri-implant tissues in which probing depth was 3.8 mm + 1.1 mm and osseointegrated implants were followed up for 7 to 8 years, Lekholm, et al. [12] defined a probing depth threshold of 5 mm for healthy tissues. Mombelli & Lang [13] and Brägger, et al. [14] also classified peri-implant sites with probing depths of up to 5 mm as healthy.
Figure 1A shows that the greatest probing depth, which was not greater than 3 mm, was found in the control group at PT, and this finding indicated that peri-implant tissues were healthy. The absence of any pathology at clinical and radiographic evaluations explains why there were no significant statistical differences in bleeding index between the two groups at baseline and PT.
In Figure 1D, the modified plaque index at baseline was greater in both groups at baseline and statistically different in the VD group between baseline and PT. Our study protocol defined that VD should be administered for eight weeks before reevaluation. This contact with the patient, as well as the weekly administration, may have consciously promoted better oral hygiene.
One of the several important actions of VD is the promotion of immune and inflammatory responses, and VD deficiency is associated with a greater prevalence of infection [15]. VD acts as an anti-inflammatory agent, as it inhibits the expression of inflammatory cytokines and stimulates monocytes and macrophages to secrete molecules that have powerful antibiotic effects [16]. According to Hiremath, et al. [17], vitamin D has an effective anti-inflammatory action when the daily dose is 500 IU to 2000 IU, a treatment indicated only for patients with levels below 30 ng/mL. In patients with gingivitis, the desired anti-inflammatory effects may be achieved by keeping supplementation for two to three months. Fretwurst, et al. [18] demonstrated that implant placement was successful after vitamin D supplementation in patients with vitamin D deficiency and early failed implants. Despite that, the results of VD supplementation on clinical peri-implant health parameters were not statistically significant in our study.
Figure 2 shows that there were statistically significant differences in the distance from bone crest to implant cervical area between groups only at baseline, but these measures were up to2.2 mm. According to Papaspyridakos, et al. [8], the criteria that define success in osseointegration accept a bone loss of 2 mm in the first year and up to 0.2 mm each year thereafter. The difference in the distance from bone crest to implant cervical area between baseline and PT in the VD group was not statistically significant. As the patients in both groups had already completed their implant rehabilitation treatments more than a year earlier, and as the 2-month interval of VD administration was too short for further measurement of distances from bone crest to implant cervical area, distances were classified as within the limits prescribed by success criteria. A more detailed evaluation of bone remodeling, local clinical conditions and oral hygiene habits should require clinical and radiographic re-examinations at a longer follow-up time. Considering the evaluation of clinical parameters used in this study, our results are not in agreement with studies that have found positive effects of VD on osseointegration and bone repair [18,19].
Conclusion
The clinical and radiographic results of this study suggest that VD supplementation for patients with insufficient serum levels does not affect peri-implant health.
References
- Schuch NJ, Garcia VC, Martini LA (2009) Vitamina D e doenças endocrinometabólicas. Arq Bras de Endocrinol e Metab 53: 625-633.
- Mechica JB (1999) Raquitismo e osteomalácia. Arq Bras de Endocrinol Metab 43: 457-466.
- Premaor MO, Furlanetto TW (2006) Hipovitaminose D em adultos: Entendendo melhor a apresentação de uma velha doença. Arq Bras de Endocrinol e Metab 50: 25-37.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. (2011) Evaluation, treatment, and prevention of vitamin D deficiency: An endocrine society clinical practice guideline. J Clin Endocrinol Metab 96: 1911-1930.
- Albrektsson T, Brånemark PI, Hansson HA, et al. (1981) Osseointegrated titanium implants: Requirements for ensuring a long-lasting, direct bone to implant anchorage in man. Acta Orthop Scand 52: 155-170.
- Carlsson L, Röstlund T, Albrektsson B, et al. (1986) Osseointegration of titanium implants. Acta Orthop Scand 57: 285-289.
- Gallucci GO, Doughtie CB, Hwang JW, et al. (2009) Five-year result of fixed implant-supported rehabilitation with distal cantilevers for the edentulous mandible. Clin Oral Implants Res 20: 601-607.
- Papaspyridakos P, Chen JC, Singh M, et al. (2012) Success criteria in implant dentistry: A systematic review. J Dent Res 91: 242-248.
- Karoussis IK, Salvi GE, Heitz-Mayfield LJ, et al. (2003) Long-term implant prognosis in patients with and without a history of chronic periodontitis: A 10-year prospective cohort study of the ITI® Dental Implant System. Res Clin Oral Impl 14: 329-339.
- Poyato-Ferrera M, Segura-Egea JJ, Bullón-Fernández P (2003) Comparison on modified bass technique with normal toothbrushing practices for efficacy in supragingival plaque removal. Int J Dent Hyg 1: 110-114.
- Ronchi FC, Sonagli M, Ronchi MGC (2012) Prevalência de hipovitaminose D em população de consultório médico. Rev Med Res 13: 173-180.
- Lekholm U, Adell R, Lindhe J, et al. (1986) Marginal tissue reactions at osseointegrated titanium fixtures. (II) A cross-sectional retrospective study. Int J Oral Maxillofac Surg 15: 53-61.
- Mombelli A, Lang NP (1994) Clinical parameters for the evaluation of dental implants. Periodontol 2000 4: 81-86.
- Brägger U, Aeschlimann S, Bürgin W, et al. (2001) Biological and technical complications and failures with fixed partial dentures (FPD) on implants and teeth after four to five years of function. Clin Oral Implants Res 12: 26-34.
- Zittermann A (2003) Vitamin D in preventive medicine: Are we ignoring the evidence? Br J Nutr 89: 552-572.
- Dietrich T, Joshipura KJ, Dawson-Hughes B, et al. (2004) Association between serum concentrations of 25-hydroxyvitamin D3 and periodontal disease in the US population. Am J Clin Nutr 80: 108-113.
- Hiremath VP, Rao CB, Naiak V, et al. (2013) Anti-inflammatory effect of vitamin d on gingivitis: A dose response randomized controlled trial. Indian J Public Health 57: 29-32.
- Fretwurst T, Grunert S, Woelber JP, et al. (2016) Vitamin D deficiency in early implant failure: Two case reports. Int J Implant Dent 2: 24.
- Mangano FG, Oskouei SG, Paz A, et al. (2018) Low serum vitamin D and early dental implant failure: Is there a connection? A retrospective clinical study on 1740 implants placed in 885 patients. J Dent Res Dent Clin Dent Prospect 12: 174-182.
Corresponding Author
Adriane Yaeko Togashi, PhD, Associate Professor, Stricto Sensu Graduate Program in Dentistry, Universidade Estadual do Oeste do Paraná, Cascavel, Brazil.
Copyright
© 2019 Piccolotto A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.