Endotracheal Tube Cuff Pressure Measurement Techniques: Safety and Reliability: A Randomized Comparative Study
Abstract
Objective: The purpose of this study was to examine cuff inflation techniques and corresponding pressure estimations, as well as associated complications, in patients undergoing general anaesthesia with intubation for cesarean delivery at the Tamale Teaching Hospital's obstetric unit.
Methods: Finger palpation of the pilot balloon, predetermined volume of air, and a pressure gauge were used to measure endotracheal tube (ETT) cuff pressure after intubation. Associated side effects were determined after 24 hours of endotracheal tube extubation.
Results: Data for 384 patients were included in the analysis. Cuff pressure measured among patients varied from < 20-30 cmH2O for the standard manometer group, 20 to 50 cmH2O for the predetermined volume of air group and < 20 to > 50 cmH2O for the finger palpation group. Side effects were recorded in 2.4% of patients from the standard manometer group, 53.2% from the predetermined volume of air group and 83.6% from the finger palpation group.
Conclusion: The finger palpation of a pilot balloon technique for cuff pressure estimation was unreliable and prone to cuff over inflation and associated with post-extubation airway complaints. Cuff pressure estimation using the standard manometer was associated with satisfactory patient outcomes.
Keywords
Endotracheal tube, Cuff pressure, Standard manometer, Predetermined volume, Manual palpation, Complication
Abbreviations
ASA-PS: American Society of Anaesthesiologists Physical Status; ECG: Electrocardiography; SpO2: Partial Pressure of Oxygen Saturation; ETT: Endotracheal Tube; ID: Internal Diameter
Introduction
Endotracheal intubation is a critical clinical skill and lifesaving procedure [1,2] used by anaesthesia and intensive care professionals to secure an airway for patients who require mechanical ventilation [3-6]. The cuff inflation creates a seal between the tracheal tube and the tracheal wall, allowing anaesthetic gases to be delivered directly into the trachea for ventilation and oxygenation while also assuring airway conservation and safety [7-9]. Endotracheal tube cuff inflation and pressure assessment are commonly regarded as essential components of anaesthetic management in surgical patients [10]. It has been found that large volume, low pressure endotracheal cuffs are less damaging to the tracheal mucosa than high pressure, low volume cuffs. Low pressure cuffs, on the other hand, can easily be overinflated to produce pressures that surpass capillary perfusion pressure [11].
The appropriate cuff pressure for preventing aspiration must be maintained within 20-40 cmH2O using the hand-held analogue manometer or spirometer technique [12-16]. The cuff should seal the airway without putting so much pressure on the trachea that circulation is impeded or the trachea is dilated [17,18]. The minimal occlusive volume approach and the palpation method can also be used to determine the intra-cuff pressure, however these methods are usually more arbitrary and prone to complications. The hand-held analogue manometer or spirometer is regarded safe but not widely available in many countries, particularly in resource-poor settings where its use is limited by the cost of purchase and maintenance [19]. As a result, the majority of anaesthesia providers in these areas rely on manual palpation to determine techniques cuff pressure. Such approaches are prone to cuff hyperinflation [20,21] and may impose a mechanical strain as well as tissue-related complications [22-24]. If the intra-cuff pressure is also too low, the patient is at risk of aspiration.
While there have been various research on endotracheal intubation protocols [25-27], the most of these have been limited to the developed world, with little data from underdeveloped countries. Furthermore, healthcare reforms in low-income countries have been extremely gradual, and nurse anaesthetists are those who frequently provide anesthesia services. Although technically competent, nurse anaesthetists may have a poor awareness of the relationship between intra-cuff and lateral tracheal wall pressure and its implications for tracheal perfusion [28]. These knowledge gaps, which the current study intends to fill, are key drivers of unfavorable patient outcomes following extubation such as sore throat, upper airway oedema, tracheal stenosis, and infections, etc.
Because cuff pressure assessed by palpation may not be the best method for detecting high cuff pressure [29,30], the purpose of this study was to compare intra-cuff pressure inflation procedures and related issues in patients undergoing general anaesthesia with intubation for cesarean delivery. The outcome of this study will contribute to the literature on endotracheal tube cuff pressure procedures at Tamale Teaching Hospital, as well as affecting anaesthesia clinical policy at the obstetric unit for required monitoring of endotracheal tube cuff pressure and its estimations.
Materials and Methods
Ethical statement
This prospective randomized comparative study was carried out at the obstetric unit of the Tamale Teaching Hospital from June 2021 to December 2021. The ethical committee of the University of Health and Allied Sciences approved the study protocol (ID No: UHAS REC A.9 [114]20-21). The clinical trial registration was obtained from ISRCTN Registry, BMC (No. ISRCTN66168037). All methods were performed under the relevant guidelines and regulations. The study protocol adhered to the CONSORT guidelines. Written informed consent was obtained from individual patients after providing them with adequate explanations regarding the aims of the study.
Subjects
This study recruited three hundred and eighty-nine (389) pregnant women who were to undergo elective cesarean section in which spinal anaesthesia was contraindicated or failed. The inclusion criteria were as follows: general anaesthesia and endotracheal intubation, age ranges of 18 to 40 years, American Society of Anaesthesiologists Physical Status (ASA-PS) score 1-4. The exclusion criteria were as follows; patients with a history of difficult intubation or multiple attempts (more than 3 attempts) during intubation, intubation performed by non-anaesthesia staff, parturient with known anatomical laryngotracheal abnormalities, and those expected to remain intubated beyond the operation room period.
Sample size determination
Due to the unknow population size, the sample size for this study was determined by the equation [31].
Necessary Sample Size = (Z-score 2*StdDev*(1-StdDev)/(margin of error)2
95% confidence interval (Z-score = 1.96),
Standard Diviation (StdDev = 0.5) and margine of error = ± 6%.
Therefore, our sample size estimated was 384 patients.
Randomization
Each recruited parturient was randomly assigned to one of three groups using a computer-generated random number table. The group allocation was concealed in a sealed opaque envelope which was opened just before the intubation.
The standard manometer group (n= 128) represented those whose endotracheal tube cuff pressures were determined by the use of a pressure gauge.
The predetermined volume of air group (n = 128) represented those whose endotracheal tube cuff (ETT cuff) pressures were estimated by a predetermined volume of air (10 ml).
The finger palpation group (n = 128) represented those whose endotracheal tube cuff pressures were determined by finger palpation of the pilot balloon.
Anaesthesia induction and cuff pressure measurement techniques
All parturients were prospectively assessed and classified according to the American Society of Anaesthesiologists physical status classification. Basic intraoperative monitoring (ECG, SpO2, Temperature, and non-invasive blood pressure) were applied, and the baseline vital signs were checked and recorded. All recruited patients had no history of difficult intubation during anaesthesia and surgery. Patient was advised not to eat any solid food for at least 6-8 hours before surgery. Independent anaesthesiologist was assigned to perform intubation and monitor patient till discharge from hospital.
In the supine position, the patient was anaesthetized with propofol 1.5-2 mg/kg, succinylcholine 1.0 mg/kg, and then intubated with the appropriate endotracheal tube size (ID = 6.5 or 7 mm; cuff type - high-volume low-pressure; Lot No. - 20170905). Successful insertion of the endotracheal tube was confirmed by either direct visualization of the endotracheal tube between the vocal cords or using capnography or the presence of equal bilateral breath sound. The vital signs (pulse rate, blood pressure, oxygen saturation, and respiratory rate) were monitored and recorded every 5 minutes for the first 30 minutes and then for every 15 minutes. Nitrous oxide was not used to maintain anaesthesia due to its possible effects on cuff pressure. Independent anaesthesiologist who was blinded to the study was asked to inflate the endotracheal tube cuff immediately after intubation using either of the following techniques: Standard manometer (VBM, Sulz, Germany), Predetermined volume of air, or Finger palpation of pilot balloon. Prior to extubation, the standard manometer was used to measure the intra-cuff pressure generated during spontaneous ventilation at the end expiratory time. The technique used and the cuff pressure measured in each group were recorded; Cuff pressure associated complaints were determined after 24 hours of extubation by an interview, and the overall perioperative satisfaction was evaluated on the day of discharge by an interview as; 4 = excellent, 3 = good, 2 = satisfactory, 1 = poor.
Primary and secondary outcomes measured
The endotracheal tube cuff was inflated and the pressure determined at the end expiratory time using a standard manometer, predetermined volume of air, or manual palpation of endotracheal tube pilot balloon immediately after intubation or prior to extubation. The technique used and the cuff pressure estimated in each group was recorded; Cuff pressure associated complications (cough, sore throat, hoarseness, and blood-streaked expectoration) were determined during an interview after 24 hours of extubation, and overall perioperative satisfaction was also evaluated on the day of discharge during an interview as; 4 = excellent, 3 = good, 2 = satisfactory, 1 = poor.
Statistical analysis
The Statistical Package for Social Sciences Software (SPSS) version 20.01 (IBM Corporation, Armonk, NY, USA) was used for data entry and analysis. Mean and SD were computed for quantitative variables such as age, weight, gestational age, BMI, cuff pressure, and the duration of intubation. Independent-samples t-test was applied for quantitative variables; age, weight, cuff pressure, BMI, duration of intubation, complaints and patient satisfaction of the anaesthesia service. Chi-square was applied for statistical comparisons between three or more groups. The data were presented in frequencies, percentages, means or SD wherever appropriate. P < 0.05 was considered significant.
Results
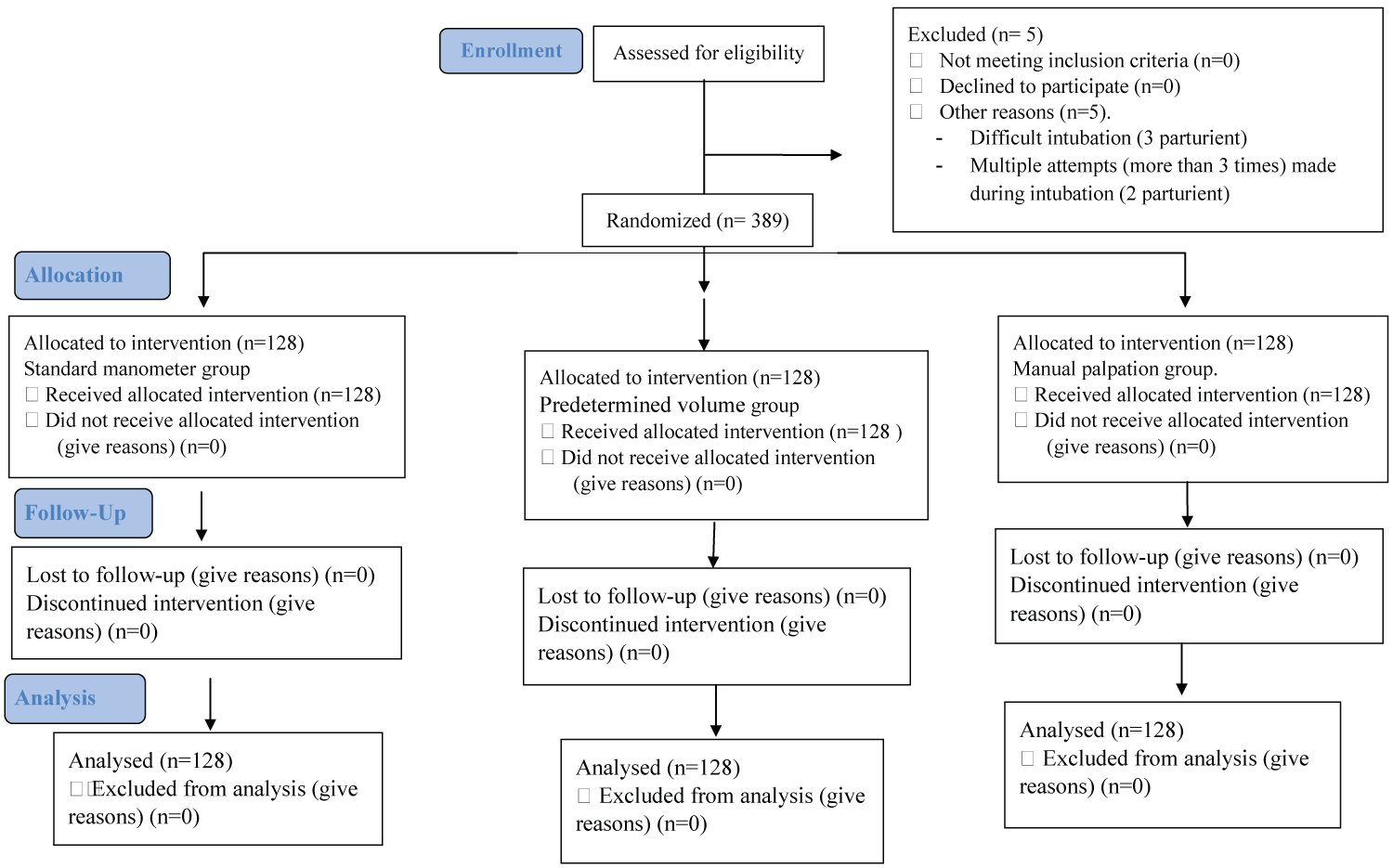
A total of 389 patients were recruited for the study, of which 384 met the inclusion criteria. The 384 were randomized into three groups of equal numbers of 128 each (Figure 1). The results showed no significant difference among patients from the standard manometer, predetermined volume of air, and the finger palpation of pilot balloon groups regarding age, weight, BMI, gestational age and duration of intubation (P < 0.96; P < 0.98; P < 0.67; P < 0.48; P < 0.96 respectively) (Table 1).
For the standard manometer group, the cuff pressure measured varied from < 20 to 30 cmH2O with 99.2% (n = 127) of the patients recording cuff pressure of 20-30 cmH2O. For the Predetermined volume group, the cuff pressure measured varied from 20 to 50 cmH2O with 53.9% (n = 69) of the patients recording cuff pressure of 20-30 cmH2O, 43.8% (n = 56) recording cuff pressure of 31-40 cmH2O and 2.3% (n = 3) recording cuff pressure of 41-50 cmH2O. For the finger palpation of pilot balloon group, the cuff pressure measured varied from < 20 to > 50 cmH2O with 5.5% (n = 7) of the patients recording cuff pressure of < 20 cmH2O, 26.6% (n = 34) recording 20-30 cmH2O, 39.8% (n = 51) recording 31-40 cmH2O, 15.6% (n = 20) recording 41-50 cmH2O and 12.5% (n = 16) recording cuff pressure of > 50 cmH2O. The data showed significant difference between the groups regarding the cuff pressures measured (P < 0.01; P < 0.01; P < 0.01; P < 0.01; P < 0.01 respectively) (Table 2).
Side effects were recorded in 2.4% of patients from the standard manometer group, among these, 1.6% (n = 2) complained of cough, and 0.8% (n = 1) complained of sore throat. For the predetermined volume of air group, side effects were recorded in 53.2% of the patients, among these, 39.1% (n = 50) complained of cough, 13.3% (n = 17) complained of sore throat, and 0.8% (n = 1) complained of hoarseness. For the manual palpation group, side effects were recorded in 83.6% of the patients, among these, 53.1% (n = 68) complained of cough, 17.2% (n = 22) complained of sore throat, 11.7% (n = 15) complained of hoarseness and 1.6% (n = 2) complained of blood-streaked expectoration. The results showed significant difference between the groups regarding the incidence of cough, sore throat, hoarseness, and blood-streaked expectoration, (P < 0.01; P < 0.01; P < 0.01; P < 0.01; P < 0.01 respectively) (Table 3).
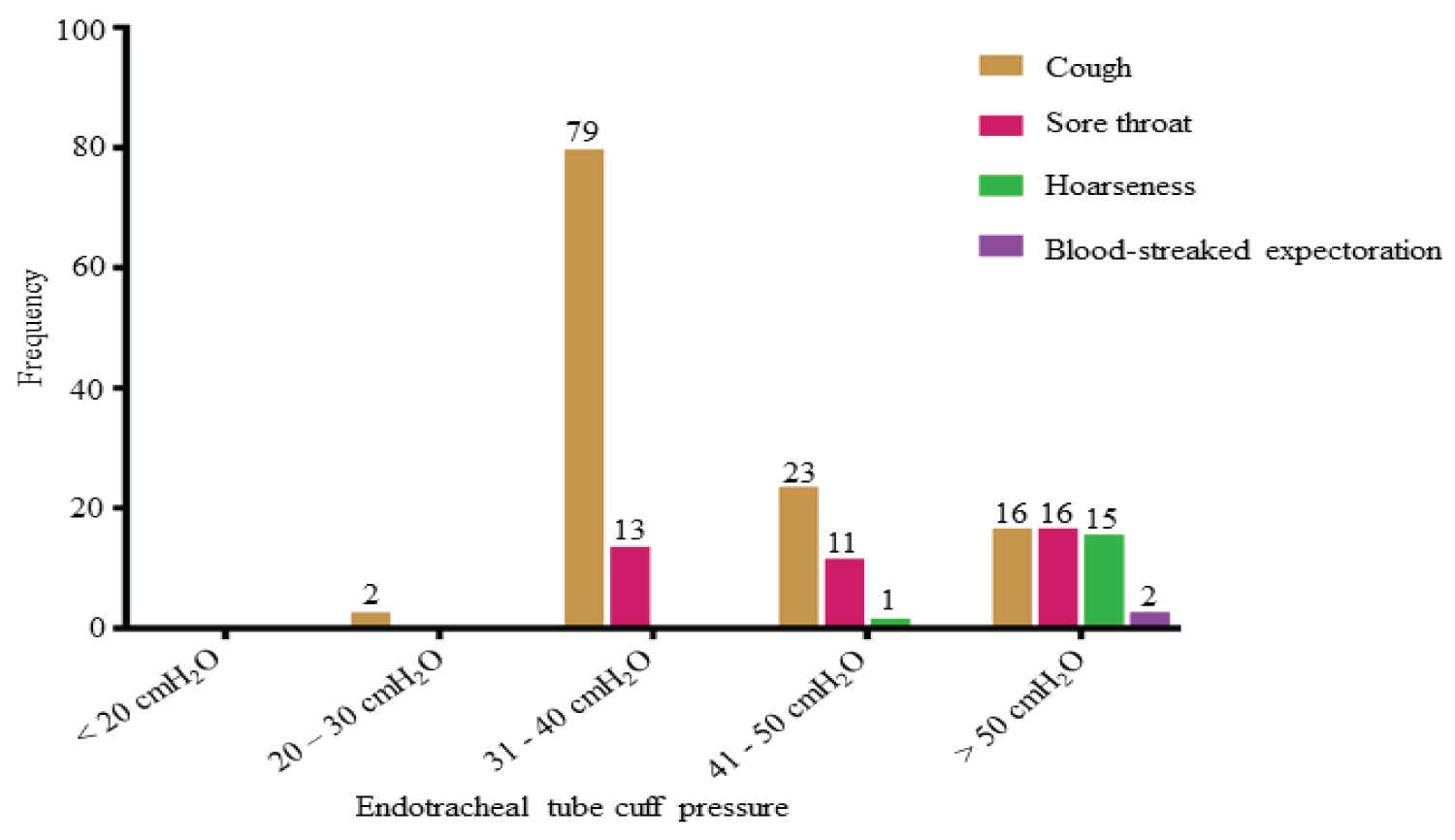
We again assessed the endotracheal tube cuff pressure measured and the occurrence of associated side effects. For cuff pressure within 20-30 cmH2O, we observed 2 of the patients who complained of cough. For those who recorded cuff pressure within 31-40 cmH2O, we observed 79 and 13 of the patients who complained of cough and sore throat respectively. For the patients who recorded cuff pressure within 41-50 cmH2O, we observed 23 of them who complained of cough, 11 who complained of sore throat, and 1 who complained of hoarseness. Whereas for those who recorded cuff pressure above 50 cmH2O, we observed 16, 16, 15 and 2 of the patients who complained of cough, sore throat, hoarseness and blood-streaked expectoration respectively (Figure 2).
We next assessed the patient's satisfaction with the anaesthesia services rendered. For the standard manometer group, 73.4% (n = 94) scored excellent, 25.8% (n = 33) scored good and 0.8% (n = 1) scored satisfactory. For the predetermined volume of air group, 52.3% (n = 67) scored excellent, 43.8% (n = 56) scored good and 3.9% (n = 5) scored satisfactory. Whereas the manual palpation of the pilot balloon group, 2.3% (n = 3) scored excellent, 18.0% (n = 23) scored good, 47.7% (n = 61) scored satisfactory and 32.0% (n = 41) scored poor for the anaesthesia service (Table 4). The data showed a significant difference between the groups regarding those who scored excellent, good, satisfactory, or poor for the anaesthesia service (P < 0.01; P < 0.01; P < 0.01; P < 0.01 respectively) (Table 4).
Discussion
It is indicated that increasing lateral wall cuff pressure above 30 cmH2O compromises blood flow, and cuff pressure more than 40 cmH2O completely impede the tracheal wall blood flow [18,32-34]. In a study of 93 patients, it was observed that 27% of cuff pressure measured exceeded 40 cmH2O using the manual palpation of pilot balloon irrespective of the experience of the anaesthesia provider [35]. Similarly, our present study recorded high cuff pressure (≥ 40 cmH2O) among the finger palpation and the predetermined volume of air groups. This suggests that finger palpation or predetermined volume techniques may correspond poorly with cuff pressure measured [36,37]. Conversely, the standard manometer technique recorded cuff pressure within the standard therapeutic range (20-30 cmH2O). This was consistent with other studies which reported a significantly lower incidence of high cuff pressure using a standard manometer [37,38].
Post-extubation airway complaint is an unpleasant experience often underestimated side effect of over-inflation of ETT cuff. Its incidence is estimated to vary from 15% to 94% [26]. Existing literature has shown a relationship between high intra-cuff pressures and tracheal lesions [25,28]. Our present study noted a high incidence of airway complaints (cough, sore throat, hoarseness, and blood-streaked expectoration) among those whose cuff pressure was ≥ 40 cmH2O compared with 20-30 cmH2O. It is therefore recommended that cuff pressure should be maintained within a narrow ideal range of 20 to 30 cmH2O to prevent post-extubation airway complaints. This can be achieved by the use of a standard manometer. Recent literature showed that the duration of intubation was associated with airway complaints such as cough, sore throat, hoarseness, and blood-streaked expectoration and would occur even following a short duration of tracheal intubation (1-3 hours) [28,39]. In the contrary, our study's results showed no significant difference between the groups regarding the duration of tracheal intubation.
Patients' safety and satisfaction with anaesthesia services have been a major concern for many anaesthetists. In our study, we assessed the patients' satisfaction with the anaesthesia service. We observed that 73.4% of the patients from the pressure gauge group scored excellent for the anaesthesia service compared with 2.3% from the finger palpation groups.
Study Limitation
The study did not highlight the issue of experience among the anaesthesia providers regarding the cuff inflation and pressure measurement technique.
Conclusion
Inadequate or excessive ETT cuff inflation is a preventable risk factor for tracheal ischemia and its complications. Excessive pressure on the tracheal mucosa, greater than the mucosa's mean capillary perfusion pressure, should be avoided during cuffed intubation. The finger palpation of a pilot balloon technique for cuff pressure estimation was unreliable and prone to cuff over inflation and associated with post-extubation airway complaints. Cuff pressure estimation using the standard manometer was associated with satisfactory patient outcomes. Because finger palpation of a pilot balloon is not a reliable guide to cuff pressure, we recommend that the pressure on the lateral tracheal wall measured at end expiration be kept between 20 and 30 cmH2O whenever possible using a pressure gauge.
Declarations
Ethics approval and consent to participate
The ethical committee of the University of Health and Allied Sciences approved the study protocol (ID No: UHAS REC A.9[114]20-21). The clinical trial registration was obtained from ISRCTN Registry, BMC (No. ISRCTN66168037). Written informed consent was obtained from each recruited parturient after providing them with adequate explanations regarding the aims of this study.
Consent to publish
Not applicable.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to patient confidentiality but are available from the corresponding author on reasonable request.
Competing interests
Authors declare that they have no competing interests.
Funding
No funding was obtained for this study.
Authors' contributions
SK, TWA, and FB conceived and designed the study. SK and TWA were responsible for the supervision and coordination of this study. SK, TWA, FB, MEH, ADBB and OS conducted the data collection.SK led the data analysis with inputs from TWA, FB, MEH, ADBB, EDK and JBZ. The first draft of the manuscript was written by SK and TWA, FB, MEH, ADBB, SO, EDK and JBZcontributed to revising and reviewing the manuscript. All authors read and approved the final manuscript before submission.
Acknowledgement
We thank the staff of the department of anaesthesia and intensive care of the Tamale Teaching hospital for providing all the necessary material we needed for this study. We also thank the management and staff of the department of obstetrics and Gynecology of the Tamale Teaching hospital for approving this study protocol and making available all the necessary materials needed for the study.
References
- Lecky F, Bryden D, Little R, et al. (2008) Emergency intubation for acutely ill and injured patients. Cochrane Database Syst Rev 2008: CD001429.
- Pepe PE, Roppolo LP, Fowler RL (2015) Prehospital endotracheal intubation: Elemental or detrimental. Crit Care 19: 1-7.
- Barak M, Bahouth H, Leiser Y, et al. (2015) Airway management of the patient with maxillofacial trauma: Review of the literature and suggested clinical approach. Biomed Res Int 2015: 724032.
- Crewdson K, Lockey DJ, Røislien J, et al. (2017) The success of pre-hospital tracheal intubation by different pre-hospital providers: A systematic literature review and meta-analysis. Crit Care 21: 31.
- Fiadjoe JE, Nishisaki A, Jagannathan N, et al. (2016) Airway management complications in children with difficult tracheal intubation from the Pediatric Difficult Intubation (PeDI) registry: A prospective cohort analysis. Lancet Respir Med 4: 37-48.
- Yentis S, Hirsch NP, James IP (2013) Anaesthesia and intensive care az-print & e-book: An encyclopedia of principles and practice. Elsevier Health Sciences.
- Chrimes N, Fritz P (2013) The Vortex Approach: management of the unanticipated difficult airway. Monash Simulation. Br J Anaesth 117: i20-i27.
- Higgs A, McGrath BA, Goddard C, et al. (2018) Guidelines for the management of tracheal intubation in critically ill adults. Br J Anaesth 120: 323-352.
- Tanaka Y, Taniguchi J, Wato Y, et al. (2012) The continuous quality improvement project for telephone-assisted instruction of cardiopulmonary resuscitation increased the incidence of bystander CPR and improved the outcomes of out-of-hospital cardiac arrests. Resuscitation 83: 1235-1241.
- Kumar M, Seet E, Van Zundert TCRV (2021) Measuring endotracheal tube intracuff pressure: no room for complacency. J Clin Monit Comput 35: 3-10.
- Young PJ, Pakeerathan S, Blunt MC, et al. (2006) A low-volume, low-pressure tracheal tube cuff reduces pulmonary aspiration Crit. Care Med 34: 632-639.
- Carhart E, Stuck LH, Salzman JG (2016) Achieving a safe endotracheal tube cuff pressure in the prehospital setting: Is it time to revise the standard cuff inflation practice. Prehospital Emerg Care 20: 273-277.
- Deutsch CJ, Tan A, Smailes S, et al. (2018) The diagnosis and management of inhalation injury: An evidence based approach. Burns 44: 1040-1051.
- Jordan P, Van Rooyen D, Venter D (2012) Endotracheal tube cuff pressure management in adult critical care units. South. African J. Crit. Care 28: 13-16.
- Lizy C, Swinnen W, Labeau S, et al. (2014) Cuff pressure of endotracheal tubes changes in body position in critically ill patients treated with mechanical ventilation. Am J Crit Care 23: 1-8.
- Bernon JK, McGuire C, Carrara H, et al. (2013) Endotracheal tube cuff pressures - The worrying reality: A comparative audit of intra-operative versus emergency intubations. S Afr Med J 103: 641-643.
- Nordin U, Lindholm CE, Wolgast M (1977) Blood flow in the rabbit tracheal mucosa under normal conditions and under the influence of tracheal intubation. Acta Anaesthesiol Scand 21: 81-94.
- Liu J, Zhang X, Gong W, et al. (2010) Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: A multicenter study. Anesth Analg 111: 1133-1137.
- Bulamba F, Kintu A, Ayupo N, et al. (2017) Achieving the recommended endotracheal tube cuff pressure: a randomized control study comparing loss of resistance syringe to pilot balloon palpation. Anesthesiol Res Pract 2017: 16-20.
- Butler KH, Clyne B (2003) Management of the difficult airway: Alternative airway techniques and adjuncts. Emerg Med Clin North Am 21: 259-289.
- Irefin T, Kopyeva S (2016) Perioperative airway management. In Basic Clinical Anesthesia, Springer, New York, NY 124: 23-24.
- Al-Qadi MO, Artenstein AW, Braman SS (2013) The ‘forgotten zone’: Acquired disorders of the trachea in adults. Respir Med 107: 1301-1313.
- Balfour Lynn M, Wright M (2019) Acute Infections That Produce Upper Airway Obstruction 2019.
- Brodsky MB, Levy MJ, Jedlanek E, et al. (2018) Laryngeal Injury and Upper Airway Symptoms after Oral Endotracheal Intubation with Mechanical Ventilation During Critical Care: A Systematic Review. Crit Care Med 176: 139-148.
- Jung B, Muller L, Subbane M, et al. (2010) An intervention to decrease complications related to endotracheal intubation in the intensive care unit: A prospective, multiple-center study. Intensive Care Med 36: 248-255.
- Maharaj CH, Buckley E, Harte BH, et al. (2007) Endotracheal intubation in patients with Cervical Spine Immobilization: A comparison of macintosh and airtarq laryngoscopes. Anesthesiology 107: 53-59.
- Schramm C, Knop J, Jensen K, et al. (2012) Role of ultrasound compared to age-related formulas for uncuffed endotracheal intubation in a pediatric population. Paediatr Anaesth 22: 781-786.
- Ghafouri HB, Saeeidi H, Yasinzadeh M (2012) Excessive endotracheal tube cuff pressure: Is there any difference between emergency physicians and anesthesiologists. Signa Vitae 7: 17-20.
- Hoffman RJ, Parwani V, Hahn IH (2006) Experienced emergency medicine physicians cannot safely inflate or estimate endotracheal tube cuff pressure using standard techniques. Am J Emerg Med 24: 139-143.
- Totonchi Z, Jalili F, Hashemian SM, et al. (2015) Tracheal stenosis and cuff pressure: Comparison of minimal occlusive volume and palpation techniques. Tanaffos 14: 252-256.
- Seyidov J, Adomaitienė R (2017) Factors influencing local tourists’ decision-making on choosing a destination: A Case of Azerbaijan. Ekonomika 95: 112-127.
- Nseir S, Duguet A, Copin M-C, et al. (2007) Continuous control of endotracheal cuff pressure and tracheal wall damage: A randomized controlled animal study. Crit Care 11: 1-8.
- Seegobin RD, Van Hasselt GL (1984) Endotracheal cuff pressure and tracheal mucosal blood flow: Endoscopic study of effects of four large volume cuffs. Br Med J 288: 965-968.
- Bernhard WN, Yost L, Joynes D, et al. (1985) Intracuff pressures in endotracheal and tracheostomy tubes: Related cuff physical characteristics. Chest 87: 720-725.
- Sengupta P, Sessler DI, Maglinger P, et al. (2004) Endotracheal tube cuff pressure in three hospitals, and the volume required to produce an appropriate cuff pressure. BMC Anesthesiol 4: 4-9.
- Dixon MJ (2018) Analysis of current practices for measuring endotracheal cuff pressures.
- Ünsal Ö, Seyhun N, Türk B, et al. (2017) The evaluation of upper airway complications secondary to intubation: cuff pressure manometer versus conventional palpation method. Sisli Etfal Hastan Tip Bul/Med Bull Sisli Hosp 52: 289-295.
- Harm F, Zuercher M, Bassi M, et al. (2013) Prospective observational study on tracheal tube cuff pressures in emergency patients- is neglecting the problem the problem. Scand J Trauma Resusc Emerg Med 21: 1-6.
- Darkwa EO, Boni F, Lamptey E, et al. (2015) Estimation of endotracheal tube cuff pressure in a large teaching hospital in Ghana. Open Journal of Anesthesiology 5: 233-241.
Corresponding Author
Sylvanus Kampo, Department of Anaesthesia and Intensive Care, School of Medicine and Dentistry, C. K. Tedam University of Technology and Applied Sciences, Navrongo, Ghana
Copyright
© 2022 Kampo S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.