Liposomal Bupivacaine is not Clinically Superior to a Standard Bupivacaine Mixture for Interscalene Nerve Block for Postoperative Pain Control in Shoulder Arthroplasty/Arthroscopy, but may Still be Beneficial
Abstract
Background: Interscalene brachial plexus blocks are commonly used to provide adjunctive, non-opioid pain relief as part of a multimodal pain control regimen for shoulder arthroscopy and arthroplasty. The purpose of this study was to assess the clinical efficacy of liposomal bupivacaine compared with a standard bupivacaine plus dexamethasone mixture in a single shot interscalene nerve block for postoperative pain control.
Methods: This single-blinded, randomized study was performed after institutional review board approval. Patients were > 18-years-old who underwent shoulder arthroplasty or arthroscopy, and were randomized into 2 groups, those who received an interscalene nerve block with liposomal bupivacaine (LB group) and those who received standard bupivacaine with dexamethasone (SB group). Primary outcomes were numerically graded pain scores (1-10), time to use of any postoperative pain medication, time to use of first postoperative opioid, and milligram morphine equivalents (MME) used up to 72 hours after the nerve block.
Results: Forty subjects were included in each group. There was no difference in time to first pain medication of any kind between groups. However, the LB group went a significantly longer time to first opioid than the SB group. Numeric pain scores were statistically lower in the LB group on average and at individual time points but did not reach clinical significance (as defined in previous studies). Cumulative MME up to 24, up to 48 and up to 72 hours were significantly reduced in the LB group. Lastly, a lower dose of bupivacaine (in mg) was needed to achieve a longer duration of block in the LB group. No significant adverse events were reported.
Conclusion: Although reductions in pain scores were statistically significant, they did not meet predefined goals for clinical significance. However, interscalene nerve block with LB provided a statistically significant reduction in postoperative opioid use compared with SB + dexamethasone. With improved patient satisfaction, reduced total dose of local anesthetic and reduced reliance on postoperative opioids, our evidence supports value added by use of LB.
Keywords
Shoulder surgery, Interscalene nerve block, Postoperative pain, Liposomal bupivacaine, Multimodal postoperative pain management
Introduction
Optimal postoperative pain management is critical to optimize outcomes for shoulder arthroscopy and arthroplasty. Interscalene brachial plexus blocks are commonly used to provide adjunctive, non-opioid pain relief as part of a multimodal pain control regimen. Effective analgesia with lower opioid intake and shorter hospital stay has been demonstrated with interscalene blocks [1,2]. The single injection interscalene block is, however, limited by the shorter duration of traditional immediate-acting local anesthetics, although additives such as dexamethasone can prolong the block for 6-8 hours [3]. In April 2018, liposomal bupivacaine (LB) was approved by the Federal Drug Administration for use in interscalene nerve blocks in the setting of shoulder surgery. Several studies have compared LB interscalene nerve block with intra-articular LB injection [4-11], or LB interscalene nerve block with continuous interscalene catheter with mixed results [12-15]. As a whole, studies show LB use in an interscalene nerve block is equivocal to SB use for shoulder surgery [16-19].
The goal of this study was to compare the clinical efficacy of LB compared with SB plus dexamethasone in a single shot interscalene nerve block for postoperative pain control. Specifically, we evaluated outpatient pain scores, use of postoperative pain medicine, patient-reported functional outcomes, frequency of adverse events and patient satisfaction through the third postoperative day after shoulder arthroplasty or arthroscopy.
Materials and Methods
Study design
We conducted a prospective, randomized, controlled, single-blinded clinical trial comparing patients undergoing shoulder arthroplasty or arthroscopy (both anatomic and reverse) treated with LB versus SB with a single bolus interscalene nerve block at a single institution between 12/3/2019 and 2/25/2021 (ClinicalTrials.gov NCT04180943 registered date 11/29/2019). All patients undergoing primary shoulder arthroplasty or arthroscopy were enrolled in the study if they met inclusion criteria (patients aged 18 years or older who met the criteria for standard of care of ambulatory surgery patients per anesthesia guidelines issued by the American Society of Anesthesiologists file:///C:/Users/m12927/Downloads/guidelines-for-ambulatory-anesthesia-and-surgery.pdf). Surgeries were performed by one of three experienced orthopedic surgeons. Exclusion criteria included contraindications to regional anesthesia, allergy to any component of multimodal analgesia, history of opioid use of > 50 morphine milligram equivalents (MME) daily, significant peripheral neuropathy or neurologic disorder affecting the upper extremity, cognitive or psychiatric condition that might affect the patient's assessment or inability to provide informed consent, and pregnancy. Nonelective procedures including infection, tumor or trauma, and revision surgeries were also excluded. Study approval was obtained from the relevant institutional review board.
Patient randomization and study blinding
The study statistician prepared stratified randomization schedules, one each for arthroplasty and arthroscopy. Subjects were randomized using random permutations of the numbers 1 and 2 to ensure balanced numbers of subjects assigned to the treatment and control groups. After providing informed consent patients received a single, equal dosed interscalene brachial plexus block with either LB or SB. Specifically, 133 mg (10 mL) LB and 0.5% bupivacaine were mixed in same syringe; the volume of bupivacaine was provider-specific based on patient weight but could not exceed 13 mL. For the control patients, the mixture was not standardized but was a provider-specific combination of bupivacaine 0.5% and lidocaine 2% (volume at provider discretion based on patient's weight) + 10 mg dexamethasone in order to simulate the variation in practice common in many institutions. Patients and the care team including surgeon, pre- and postoperative nurses, and study team members collecting and recording data were all blinded to the randomization assignment. The lead research nurse who conducted the randomization and the anesthesiologist who performed the block were not blinded.
All interscalene nerve blocks were performed with ultrasound guidance by an attending anesthesiologist experienced in performing these blocks. Patients underwent either monitored anesthesia care with a propofol infusion, or general anesthesia with endotracheal tube or laryngeal mask airway, depending on anesthesiologist clinical judgement. A standardized pain management protocol was prescribed to all patients, that included scheduled doses of 1000 mg acetaminophen every 8 hours, and 5 mg oxycodone every 4 to 6 hours as needed for pain.
Assessment
Study staff contacted the patient by phone on postoperative days 1, 2, and 3 to assess pain levels, pain medication consumption, sleep, satisfaction, functional outcome and adverse events. The primary outcome investigated was time to first postoperative pain medication, obtained from either from the medical record if administered in the post anesthesia care unit, or via telephone assessment if consumed outside the hospital. In addition, all doses and times of narcotics measured in Milligrams of Morphine equivalents (MME) administered during the inpatient stay were compared (See Appendix for data collection sheet). The secondary outcome measures included: 1) Time to first opioid; 2) Numeric pain scores (0, no pain through 10, worst pain possible) at 24, 48, and 72 hours; 3) MME at 24, 48, and 72 hours postoperatively; 4) Cumulative MME at 24, 48, and 72 hours postoperatively; 5) Duration of block; 6) Incidence of adverse events during first 72 hours; and 7) Patient satisfaction.
Study team members asked at every time point about adverse events, specifically nausea, somnolence, local anesthetic toxicity (tinnitus, perioral numbness, dysgeusia), and adverse events specifically related to the nerve block including watery eye, droopy eye, hoarseness, difficulty breathing/shortness of breath, dizziness and fainting.
Statistical analysis
Initial significance tests were run for differences between treatment groups (LB vs. SB) with regard to patient characteristics. Categorical variables were compared using chi-square and continuous variables were compared using Student's t-tests. Kaplan-Meier analysis was used to compare time to first post-op pain medication between the LB and SB groups. Time to first opioid was also analyzed using Kaplan-Meier analysis. Milligrams of Morphine equivalents (MME) at 24 hours, 48 hours, and 72 hours post-block as well as cumulative MME was compared between LB and SB groups using the Wilcoxon Rank sum test. Numeric pain scores between the LB and SB groups were compared in the same manner. The minimal clinically important difference between groups for pain scores was considered clinically significant if > 2.0 as has been established in the orthopedic literature, so our outcome [20-23].
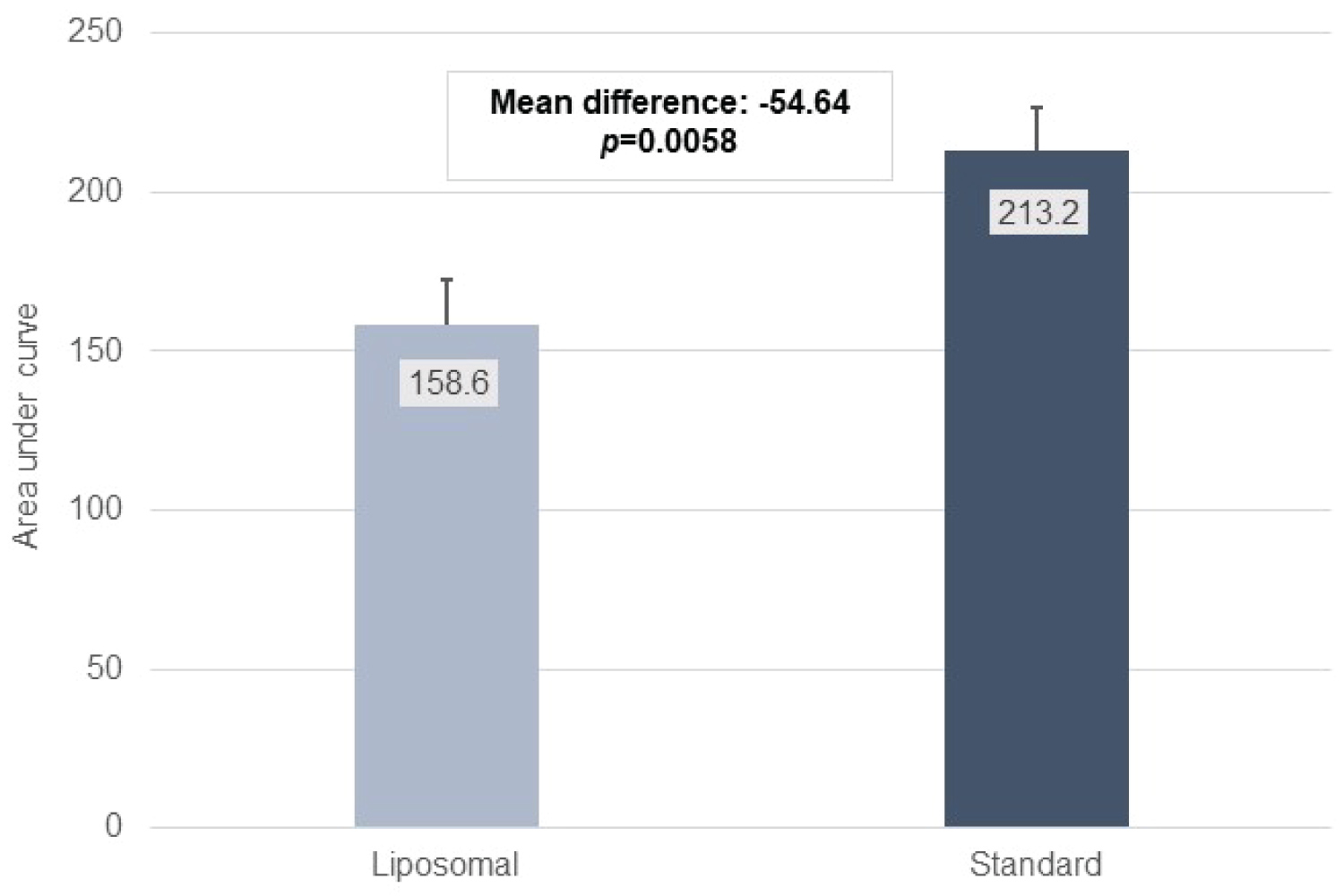
An area under the curve (AUC) analysis was conducted for pain scores from 24 to 72 hours post-block. Each subject's pain score area was calculated using trapezoidal approximation; mean area under the curve was compared between LB and SB groups using the student's t-test. All statistical analyses were conducted using SAS 9.4 (Cary, NC).
Results
A total of 80 subjects were included, 40 in the LB Group and 40 in the SB group. The study population consisted of 21 men and 19 women, with an average age of 57.1 years. Subjects in the SB group were an average of 6 years older than the LB group (p = 0.0256). All other patient characteristics did not differ between treatment groups (Table 1). There were no significant adverse events as defined in the study protocol.
Time to first medication
There was no difference in time to first pain medication between treatment groups (log rank test p-value = 0.3918). All subjects reported use of some pain medication in the 72 hours post-operatively. Median time to first pain medication was 672 minutes in the LB group and 677 minutes in the SB group (p-value = 0.7192 by the Wilcoxon Rank Sum test).
Time to first opioid
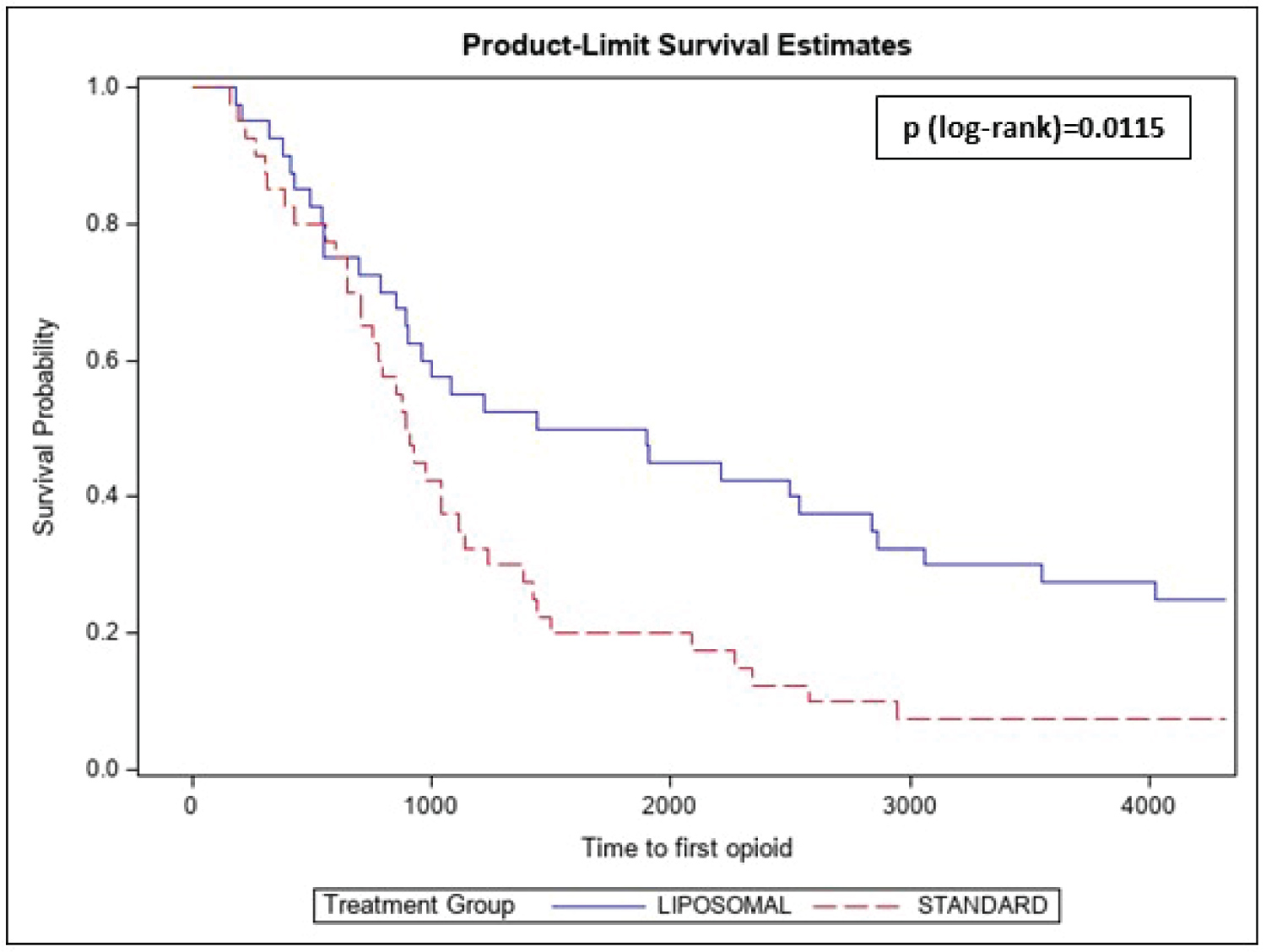
The median time by which 50% of subjects had used an opioid was greater for the LB group (1444 min) as compared to the SB group (894 min); Kaplan-Meier analysis (log-rank test) for time to first opioid was statistically significant at p = 0.0115 (Figure 1).
Pain scores and total opioid consumption
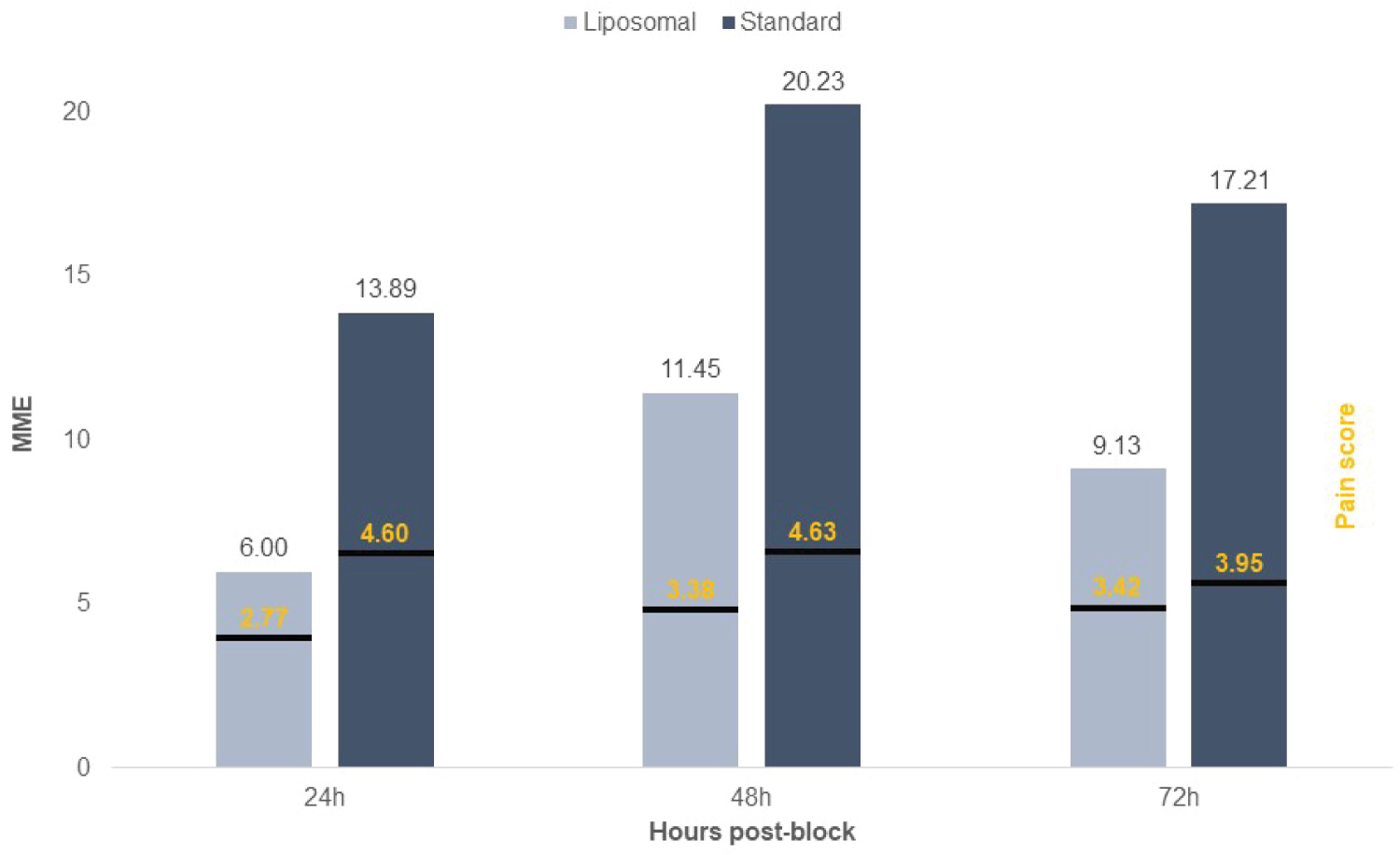
There were significant differences between groups with respect to pain scores during the first 72 hours (Table 2). One subject in the LB group did not have pain score. For the LB group, the worst pain over 72 hours was 6.3 v 8.3 in the SB group (p = 0.0014). The least pain over 72 hours was 1.0 for the LB group and 1.5 for the SB group (p = 0.0013). The average pain score over the first 72 hours was 3.2 for LB group v 4.4 for the SB group (p = 0.0018). AUC analyses (Figure 2). Figure 3 compares LB and SB groups at each individual time point with respect to pain score and MME. Pain scores at the 24-hour phone call and at the 48-hour phone call were significantly lower in the LB group as compared to the SB group (p = 0.0003 and p = 0.0042, respectively). The difference was not significant at the 72-hour phone call (Figure 3). Despite statistical significance, the minimally clinically significant difference of 2.0 was not seen at any time point.
MME for each 24-hour interval taken independently was significantly lower among the LB group for the 24-hour post-block period (p = 0.0017) and for the 24-48-hour period p = 0.0061; (Table 3 and Figure 3). The difference between groups was not significant for the 48-72-hour period (Table 3). Cumulative MME up to 24, up to 48 and up to 72 hours were significantly reduced in the LB group as compared to SB group (p = 0.0072, p = 0.0033 and p = 0.0056, respectively).
For average pain over the time course, the interaction term for pain measurement*time was significant. This indicates that the pattern of change for reported pain differed between the LB and SB groups. As seen in Figure 2, the pain score in the LB group started significantly lower and then increased slightly and tapered off by 72 hours. In the SB group, the 24-hour and 48-hour measures were relatively stable and then decreased at 72-hour. For MME over the time course, the interaction term for MME*time was not significant (0.9566), meaning that the pattern of MME for each 24-hour interval did not differ between treatment groups (same general pattern of higher MME at 48-hour followed by lower at 72-hour). However, the overall effect for treatment group was significant (lower average MME among the LB group for all time points), p = 0.0032, as was the main effect of time (MME increased over time in both groups), p = 0.0012. The amount of fentanyl and ketorolac given intra- and post-operatively (eg. in post anesthesia care unit) was not related to the treatment group and therefore, cannot be confounders in any of the outcome analyses.
Duration of block
Subjects were asked whether the block had waned during the phone calls. At the 24-hour call, a greater proportion of subjects in the SB group reported that their block had worn off; 7 (17.5%) said that the block had not yet subsided in the SB group as compared with 24 (60%) in the LB group (p < 0.0001). At 72 hours, a similar proportion in each group reported that the block had worn off (90.6% in the LB group and 94.9% in the SB group; p = 0.6518). Interestingly, the total amount of local anesthetics (mg) including bupivacaine and lidocaine was significantly lower in the LB group (199.33 mg) compared to the SB group (224.00 mg) which is significant at p < 0.0001 using Wilcoxon rank sum test.
Adverse events
Reported incidence of adverse events post-block did not differ between LB and SB groups at the 24-, 48-, or 72-hour phone calls (Table 4). At 24 hours, 12 subjects (30.0%) reported one or more adverse events in the LB group versus 8 subjects (20.0%) in the SB group (p = 0.3014). The most frequently reported adverse event in both groups was shortness of breath (n = 7 at 24h; 4 in LB group and 3 in SB group), followed by nausea (n = 6 at 24h; 4 in LB group and 2 in SB group) and dizziness (n = 4 at 24h; 3 in LB group and 1 in SB group).
Patient satisfaction
Reported satisfaction with pain control ("on a scale of 1-10, how satisfied are you with your pain control so far after surgery") was significantly higher in the LB group compared to the SB group (mean 9.0 ± 1.4 and 7.6 ± 2.8 in LB and SB groups, respectively; p = 0.0214).
Discussion
Our primary outcome, time to first pain medicine of any kind, did not differ between LB and SB study groups. However, the median time by which 50% of subjects had used an opioid was greater for the LB group; the MME were significantly lower for the LB group cumulatively and at each time point in all but the 48-72-hour phone calls. At 24 hours post-block, 60% of patients in the LB group reported that the block was still in effect. These results suggest that an interscalene nerve block with LB may not be clinically superior to an interscalene nerve block with a varied amount of bupivacaine, lidocaine, and dexamethasone in terms of our primary outcomes. However, the LB interscalene nerve block did reduce the amount of opioid consumption, which is clinically important due to the importance of reducing postoperative opioid consumption and thus the potential for opioid dependence. With improved patient satisfaction, longer duration of block, reduced total dose of local anesthetic and reduced reliance on postoperative opioids, our evidence supports value added by use of LB.
The LB group had lower numeric pain scores at the 24- and 48-hour phone calls and for all categories during the 72 hours postoperatively: The pain scores for the worst pain over 72 hours (6.3 v 8.3), the least pain over 72 hours (1.0 v 1.5), and the average pain scores (3.2 v 4.4). Although statistically significant, our results do not meet the minimally clinically significant difference in pain scores of 2.0; the worst pain over 72 hours was the only outcome measure that reached clinical significance. However, the amount of local anesthetic used (mg) in the LB group was significantly lower than the amount used in the SB group while still the LB group demonstrated a notably increased duration of the block and patient satisfaction. In order to prevent bias, we used both AUC and individual timepoint analyses and these results corroborated each other. There were no confounders identified in the intraoperative analgesic regimens.
Many studies have compared LB interscalene nerve blocks to a placebo [24], others compared to an indwelling, continually infusing catheter [13-15,25] and others compared to surgeon infiltration [7,9]. In these studies, LB was deemed superior. Recently Hussain, et al. performed a largescale systematic review and meta-analysis of 9 clinical trials using LB for nerve blocks in a variety of surgeries and block types, and concluded that despite reaching statistical significance, postoperative pain scores were not clinically improved with LB [26]. Hattrup, et al. conducted a randomized, double-blinded study to compare interscalene block with SB vs. LB after shoulder replacement surgery and found no significant difference in time to first opioid rescue, total MME use, or patient satisfaction with pain management [17]. Most recently, Kim, et al. demonstrated a lack of superiority for interscalene block with LB compared to SB + dexamethasone in terms of numerical pain scales duration of analgesia, and opioid use in ambulatory shoulder surgery [18]. Flaherty, et al. also recently demonstrated no decrease in opioid use with LB added to interscalene nerve block for rotator cuff repair compared with SB [16]. We provide corroborating evidence of this lack of superiority of liposomal bupivacaine, but also some additional benefits that go beyond traditional outcomes. Our study is unique because our control group SB also included the additive dexamethasone, which is known to extend block duration [3], it included patients undergoing arthroplasty, which is less common and often more extensive, as well as arthroscopy. Moreover, we let the individual clinicians determine the dose of local anesthetic used in the SB interscalene nerve block in order to allow for variable clinical scenarios and how the total dose of local anesthetic may affect results. Our study also addressed total opioid consumption during the 72-hour period after the block, which is an important benchmark for reducing population opioid dependence.
When our outcome measures are compared overall, they demonstrate that the use of LB in an interscalene nerve block may be a superior option, resulting in less risk of local anesthetic toxicity and reduction in postoperative opioid dependence. In addition, the surgeons participating in the study had a strong preference for the use of LB because of the positive subjective comments received from patients postoperatively.
Study limitations
This study had several limitations, most notably was the sample size. The difference in pain scores did not reach clinical significance, but our study was not powered to do so. A larger sample size may or may not have allowed the comparisons to reach clinical significance; a larger sample size may also have allowed us to compare results between arthroplasty and arthroscopy. In addition, the dose in mg of local anesthetic differed between the LB group vs. the SB group, and the amount within each group varied. The total dose of SB mixed with LB in the LB group was left to the discretion of the performing Anesthesiologist based on patient weight, and the total dose of SB and any amount of lidocaine used in the SB group was also based on Anesthesiologist judgement, resulting in a control group that was not uniform. However, we felt that despite this limitation, it more accurately represented the real-world variations in use of local anesthetics in interscalene nerve blocks in different clinical settings. The number of surgeons participating in the trial was limited to 3, which may have reduced the variability in pain experienced in each surgical procedure as the surgical technique was relatively homogeneous. We did not evaluate more long-term outcomes such as pain-related disability, persistent pain, and opioid dependence. Lastly, we excluded patients who used more than a predefined daily amount of opioid, which did not allow us to make conclusions about the benefit of interscalene nerve blocks in populations with long-term opioid dependence.
Conclusion
Our study provides multiple lines of evidence that LB used in interscalene nerve blocks for shoulder arthroscopy/arthroplasty provides a superior advantage for patients' postoperative pain control. Specifically, we demonstrated decreased use of postoperative opioids, increased duration of block, decreased local anesthetic dose and patient satisfaction. While our primary outcomes in terms of pain scores did not reach clinical significance, LB may still be considered beneficial.
Acknowledgments
Drs. James Anania, Christopher McCarthy, Dean Robinson, Erica Zulueta, Itisha Bansal, Scott Raffo and Chinedu Abara.
References
- Lehmann LJ, Loosen G, Weiss C, et al. (2015) Interscalene plexus block versus general anaesthesia for shoulder surgery: A randomized controlled study. Eur J Orthop Surg Traumatol 25: 255-261.
- Warrender WJ, Syed UAM, Hammoud S, et al. (2017) Pain management after outpatient shoulder arthroscopy: A systematic review of randomized controlled trials. Am J Sports Med 45: 1676-1686.
- Kirkham KR, Jacot-Guillarmod A, Albrecht E, et al. (2018) Optimal dose of perineural dexamethasone to prolong analgesia after brachial plexus blockade: A systematic review and meta-analysis. Anesth Analg 126: 270-279.
- Ali I, Gupta HO, Khazzam M, et al. (2021) Do local liposomal bupivacaine and interscalene nerve block provide similar pain control after shoulder arthroplasty? A dual-center randomized dontrolled trial. J Shoulder Elbow Surg 30: S145-S152.
- He J, Li Y (2020) Randomized trial protocol of interscalene nerve block vs liposomal bupivacaine injection after total shoulder arthroplasty. Medicine (Baltimore) 99: e20968.
- Ilfeld BM, Eisenach JC, Gabriel RA (2021) Clinical effectiveness of liposomal bupivacaine administered by infiltration or peripheral nerve block to treat postoperative pain. Anesthesiology 134: 283-344.
- Namdari S, Nicholson T, Abboud J, et al. (2017) Randomized controlled trial of interscalene block compared with injectable liposomal bupivacaine in shoulder arthroplasty. J Bone Joint Surg Am 99: 550-556.
- Namdari S, Nicholson T, Abboud J, et al. (2018) Interscalene block with and without intraoperative local infiltration with liposomal bupivacaine in shoulder arthroplasty: A randomized controlled trial. J Bone Joint Surg Am 100: 1373-1378.
- Okoroha KR, Lynch JR, Keller RA, et al. (2016) Liposomal bupivacaine versus interscalene nerve block for pain control after shoulder arthroplasty: A prospective randomized trial. J Shoulder Elbow Surg 25: 1742-1748.
- Wang K, Zhang HX (2017) Liposomal bupivacaine versus interscalene nerve block for pain control after total shoulder arthroplasty: A systematic review and meta-analysis. Int J Surg 46: 61-70.
- Yan Z, Chen Z, Ma C (2017) Liposomal bupivacaine versus interscalene nerve block for pain control after shoulder arthroplasty: A meta-analysis. Medicine (Baltimore) 96: e7226.
- Abildgaard JT, Lonergan KT, Tolan SJ, et al. (2017) Liposomal bupivacaine versus indwelling interscalene nerve block for postoperative pain control in shoulder arthroplasty: A prospective randomized controlled trial. J Shoulder Elbow Surg 26: 1175-1181.
- Orebaugh SL, Dewasurendra A (2020) Has the future arrived? Liposomal bupivacaine versus perineural catheters and additives for interscalene brachial plexus block. Curr Opin Anaesthesiol 33: 704-709.
- Sabesan VJ, Shahriar R, Petersen-Fitts GR, et al. (2017) A prospective randomized controlled trial to identify the optimal postoperative pain management in shoulder arthroplasty: Liposomal bupivacaine versus continuous interscalene catheter. J Shoulder Elbow Surg 26: 1810-1817.
- Weir TB, Simpson N, Aneizi A, et al. (2020) Single-shot liposomal bupivacaine interscalene block versus continuous interscalene catheter in total shoulder arthroplasty: Opioid administration, pain scores, and complications. J Orthop 22: 261-267.
- Flaherty JM, Berg AA, Harrison A, et al. (2022) Comparing liposomal bupivacaine plus bupivacaine to bupivacaine alone in interscalene blocks for rotator cuff repair surgery: A randomized clinical trial. Reg Anesth Pain Med 47: 309-312.
- Hattrup SJ, Chung AS, Rosenfeld DM, et al. (2021) Liposomal bupivacaine interscalene nerve block in shoulder arthroplasty is not superior to plain bupivacaine: A double-blinded prospective randomized control trial. J Shoulder Elbow Surg 30: 587-598.
- Kim DH, Liu J, Beathe JC, et al. (2022) Interscalene brachial plexus block with liposomal bupivacaine versus standard bupivacaine with perineural dexamethasone: A noninferiority trial. Anesthesiology 136: 434-447.
- Vandepitte C, Kuroda M, Witvrouw R, et al. (2017) Addition of liposome bupivacaine to bupivacaine HCl versus bupivacaine HCl alone for interscalene brachial plexus block in patients having major shoulder surgery. Reg Anesth Pain Med 42: 334-341.
- Berglund DD, Law TY, Rosas S, et al. (2019) The procedure value index: A new method for quantifying value in shoulder arthroplasty. J Shoulder Elbow Surg 28: 335-340.
- Mease PJ, Spaeth M, Clauw DJ, et al. (2011) Estimation of minimum clinically important difference for pain in fibromyalgia. Arthritis Care Res (Hoboken) 63: 821-826.
- Tashjian RZ, Hung M, Keener JD, et al. (2017) Determining the minimal clinically important difference for the American Shoulder and Elbow Surgeons score, Simple Shoulder Test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. J Shoulder Elbow Surg 26: 144-148.
- Tashjian RZ, Shin J, Broschinsky K, et al. (2020) Minimal clinically important differences in the American Shoulder and Elbow Surgeons, Simple Shoulder Test, and visual analog scale pain scores after arthroscopic rotator cuff repair. J Shoulder Elbow Surg 29: 1406-1411.
- Patel MA, Gadsden JC, Nedeljkovic SS, et al. (2020) Brachial plexus block with liposomal bupivacaine for shoulder surgery improves analgesia and reduces opioid consumption: Results from a multicenter, randomized, double-blind, controlled trial. Pain Med 21: 387-400.
- Weller WJ, Azzam MG, Smith RA, et al. (2017) Liposomal bupivacaine mixture has similar pain relief and significantly fewer complications at less cost compared to indwelling interscalene catheter in total shoulder arthroplasty. J Arthroplasty 32: 3557-3562.
- Hussain N, Brull R, Sheehy B, et al. (2021) Perineural liposomal bupivacaine is not superior to nonliposomal bupivacaine for peripheral nerve block analgesia. Anesthesiology 134: 147-164.
Corresponding Author
Linda Demma, MD, PhD, Department of Anesthesiology, Bassett Healthcare, 1 Atwell Rd, Cooperstown, NY 13326, USA, Tel +1-678-488-0055
Copyright
© 2022 Demma L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.