Retained Supraclavicular Peripheral Nerve Catheter
Introduction
The use of continuous peripheral nerve block catheters (CPNB) is widespread for the control of intraoperative and postoperative pain with the benefits espoused in the literature; CPNB catheters provide effective pain control in the perioperative period which may facilitate earlier discharge, improve postoperative rehabilitation, improve patient satisfaction, and decrease the use of opioids postoperatively [1-3]. In addition to improved analgesia, use of CPNB is associated with less sedation, nausea, and pruritis [2]. Various techniques for removal include open surgery, minimally invasive techniques under fluoroscopic guidance, manipulation of patient position, and prolonged traction [1,4-6]. In our case report, a supraclavicular continuous nerve block catheter was retained and subsequently removed with minimally invasively under fluoroscopy by Interventional Radiology. CPNB catheters will continue to be placed due to the many benefits, and minimally invasive options for removal of retained catheters will continue to serve as a beneficial option compared to open surgical removal.
Case Report
The patient and next of kin approved reporting this case and signed appropriate consent forms. A 31-year-old female, American Society Anesthesiologists physical status I, underwent a right wrist diagnostic arthroscopy with triangular fibrocartilage complex (TFCC) debridement and right wrist ulnar shortening osteotomy. The patient had a history of right ulnar sided wrist pain who failed non-operative management. Pre-operative MRI demonstrated a central TFCC tear as well as a 2 mm of ulnar positive variance on her plain radiographs. The attending surgeon requested a supraclavicular nerve block and CPNB catheter placement for intraoperative and postoperative pain control. After review of risks and benefits, the patient consented to regional anesthesia and sedation with Propofol. The surgery and immediate postoperative course were unremarkable.
Insertion was uneventful with the use of a previously described ultrasound-guided technique. A 19-gauge single-orifice nonstimulating catheter (Arrow FlexTip Plus, Teleflex Medical, Wayne, PA) was advanced without resistance approximately 4 cm beyond the tip of the 17-gauge Tuohy-tip placement needle after hydrodissection. The patient was discharged the same day with adequate analgesic control. The duration and effect of the CPNB infusion of 0.2% Ropivacaine at 10 cc/hr lasted approximately 48 hours.
On postoperative day 2, the patient attempted to remove the catheter at home but experienced significant discomfort with mild traction in the right posterior scapular region. She subsequently presented to the ambulatory center complaining of inability to remove the catheter. The catheter was examined at the patient's bedside in a sterile fashion.
The catheter tip was difficult to visualize with ultrasound. However, when traction was applied the catheter and brachial plexus would move as a unit. Multiple maneuvers to free the catheter at the patient's bedside were trialed, including concomitant injection of normal saline via the catheter, with slow, steady traction, applied to the free end of the catheter but due to mild paresthesias further attempts were halted. No other maneuvers were conducted to remove the catheter at that time due to concerns for potential nerve injury, and Interventional Radiology at our institution was consulted for catheter removal.
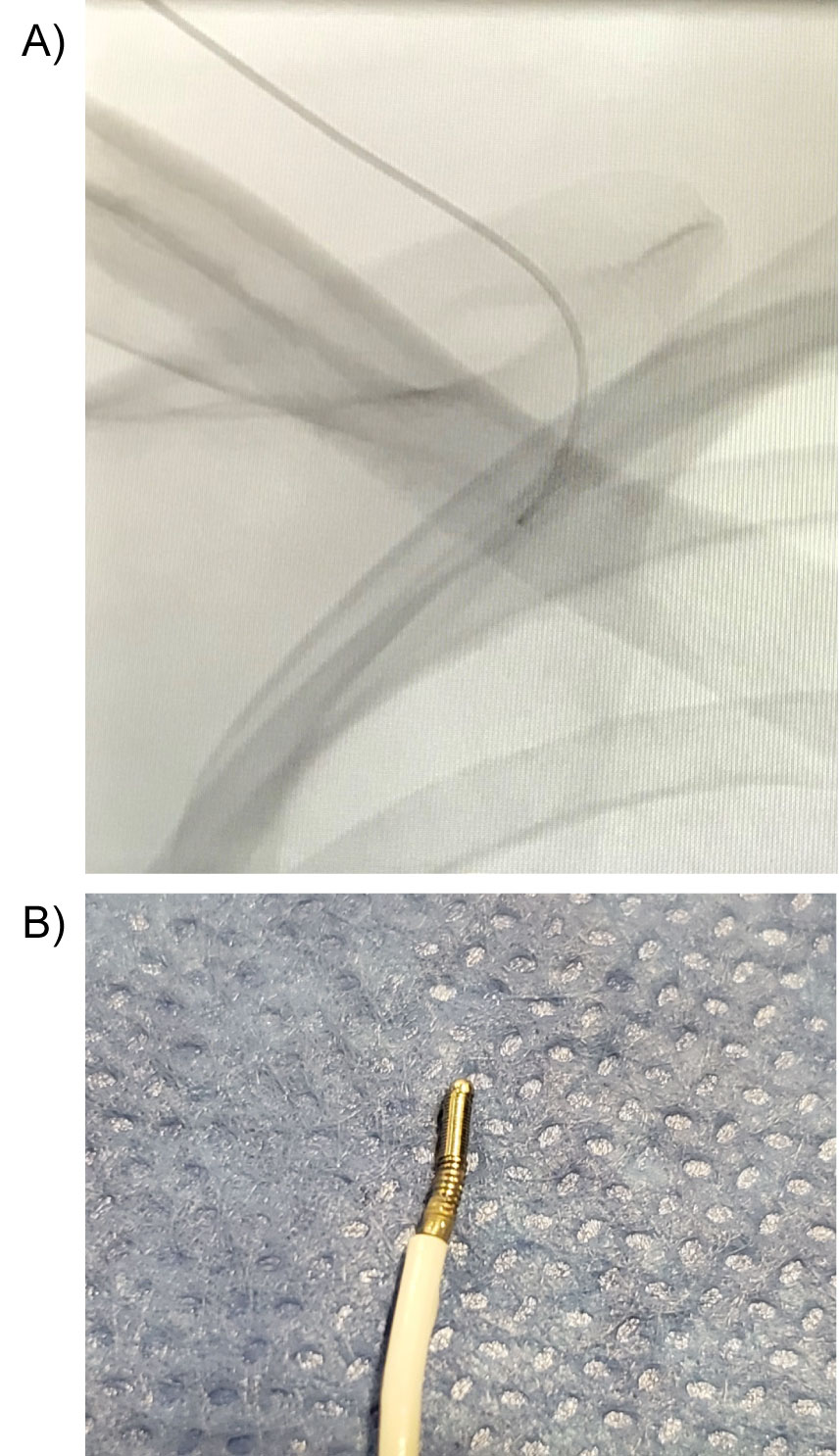
The patient was brought to the Interventional Radiology fluoroscopy suite and the catheter and surrounding tissue were prepared and draped in standard sterile fashion. The patient was placed under moderate sedation with Fentanyl and Versed. After disconnecting the hub, an 0.018" Nitrex wire (ev3, Plymouth, MN) was inserted through the catheter with attempts to elongate and provide stability. Under fluoroscopy, the tip of catheter visibly straightened and changed position, however light tension on the catheter elicited severe pain. This was re-attempted with the back end with similar results. Next, the outer portion of a 6 French Introducer System (Mac-NV, Merit Medical, Jordan, UT) was advanced over the catheter and Nitrex wire while pinning the catheter-wire complex. Unfortunately, attempt to remove the catheter was unsuccessful due to severe pain with light traction and the 6 Fr catheter was unable to be fully advanced to sheath the catheter. Finally, A Tuohy-Borst adapter was placed on the hub of the 6-French dilator. Approximately 15 cc of sterile saline was injected through the side port of the Tuohy-Borst adapter for hydrodissection. Steady, light tension was again applied to the catheter with forward pressure of the 6 French dilator allowing removal of the catheter without pain. On visual inspection, the catheter was intact, however the coiled tip of the catheter had tissue intertwined (Figure 1A and Figure 1B).
The patient has been followed for 5 months. Initial symptoms following catheter removal included moderate, intermittent paresthesias in the axilla and T1 dermatomal distribution. The patient declined EMG testing but has continued physical therapy with Physical Medicine and Rehabilitation to almost complete resolution of symptoms.
Discussion
The incidence of CPNB catheter complications is relatively low, but may consist of infection, nerve injury, local anesthetic systemic toxicity, pump malfunction, catheter displacement, obstruction, and catheter migration [2,3,7]. Catheter retention specifically is estimated to occur in only 1-2 per 1000 patients [1,5,6]. 1,5,6 Causes of CBNP catheter retention may include knotting, tissue adhesion, or even tissue invagination, with knotting the most commonly reported cause in the literature [1,5,8]. Risk factors for retained catheters may include excessive insertion length and the use of stimulating catheters [1,4,6]. A study involving rat models to evaluate the effect of catheter design on tissue adhesion suggested that the exposed metal coils at the tip of stimulating catheters could separate during placement and pinch tissue between the coils, leading to retention; the same study demonstrated significant adhesion development with use of a stimulating catheter [9]. Catheter retention thus may be influenced by catheter type and insertion technique.
When troubleshooting retained catheters, if noninvasive techniques for catheter removal fail, minimally invasive intervention may be a viable option. Anesthesiologists with experience in fluoroscopic guidance may intervene when access to Interventional Radiologists is not readily available, and the procedure can be performed with minimal or moderate sedation. However, for issues involving complex knots or catheters nearby sensitive neurovascular structures, care should be deferred to an experienced Interventional Radiologist [5].
Long-term neurologic sequelae following removal of retained CBNP catheters appear to be minimal, but additional data needs to be gathered when complications are reported. While catheter complications are rare, it is important to continue to optimize safe and efficacious practice. Evidence-based practice to avoid retained or knotted catheters involves limiting the amount of catheter over-threading past the needle hub to less than 5 cmat the time of insertion [1,5,8,9]. While safer practices of catheter insertion and maintenance continue to be developed, safe and minimally invasive options for resolving catheter malfunction and retention should continue to be optimized.
References
- Gharabawy R, Abd-Elsayed A, Elsharkawy H, et al. (2014) The Cleveland Clinic experience with supraclavicular and popliteal ambulatory nerve catheters. Scientific World Journal 2014.
- JM Richman, SS Liu, G Courpas, et al. (2006) Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesthesia & Analgesia 102: 248-257.
- PF White, T Issioui, GD Skrivanek, et al. (2003) The use of a continuous popliteal sciatic nerve block after surgery involving the foot and ankle: does it improve the quality of recovery. Anesth Analg 97: 1303-1309.
- Borg LK, Kumar G, Funck N, et al. (2018) Six Month Follow-Up of a Patient With a Retained Fascia Iliaca Catheter: A Case Report. A APract 10: 107-109.
- Burgher AH, Hebl JR (2007) Minimally invasive retrieval of knotted nonstimulating peripheral nerve catheters. Reg Anesth Pain Med 32: 162-166.
- Abrahams MS, Noles LM, Cross R, et al. (2011) Retained stimulating perineural catheters: A report of four cases. Reg Anesth Pain Med 36: 476-480.
- BM Ilfeld, TE Morey, RD Wang, et al. (2002) Continuous popliteal sciatic nerve block for postoperative pain control at home: a randomized, double-blinded, placebcontrolled study. Anesthesiology 97: 959-965.
- M David (2003) Knotted peripheral nerve catheter. Regional Anesthesia and Pain Medicine 28: 487-488.
- Offerdahl MR, Lennon RL, Horlocker TT (2004) Successful removal of a knotted fascia iliaca catheter: Principles of patient positioning for peripheral nerve catheter extraction. Anesth Analg 99: 1550-1552.
Corresponding Author
Ricardo Serrano, MD, Assistant Professor, Anesthesiology, University of North Carolina at Chapel Hill, North Carolina, USA.
Copyright
© 2019 Suggs J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.