Aneurysm of Extracranial Internal Carotid Artery: A Case Report
Abstract
Introduction: Aneurysms of the extracranial internal artery (ICA) are rare and accountable for about 1% of all cerebral anerysms , it's an uncommon patology, reported in literature as individual case or small series. Aneurysm of extracranial carotid artery etiology is diverse and ranges from athrosclerosis, infection, fibromuscolar dysplasia, connettive tissue desease to traumatic or spontaneous dissection, patch pseudoaneurysm from prior repair. Rupture and thrombo-embolism are two major risk of aneurysm of ICA, wich may lead to acute ischaemic attacks and strokes.
Case presentation: A 57-year-old woman without medical history, presented passing diplopia and distesthesia at right half face. Duplex ultrasound that revealed a saccular aneurysm of right. CT angiography confirmed the diagnosis. The first approach was endovascular, without results because a difficult signing of ICA downstream aneurysm. So was performed an oper surgical resection of the aneurysm, the ICA ends were bevelet to the appropriate lenght and anastomosed in an end to end fashion.
Discussion: The available information on extracranial carotid artery aneurysm treatment in the litterature suffers greatly because of its rarity, from small cases series, missing data, publication bias. Both endovascular ans open surgery as well as medical treatment have been raccomended depending on desease location and comorbities.
Conlcusion: Surgical repair can be safe and effective solution to treat extracranial ICA aneurysm, however the choice of treatment should be evaluated time by time, according to symptoms of patients and comorbities but, mostly, to the aneurysm conformation.
Keywords
Extracranial carotid artery, Aneurysm, Surgical treatment, Endovascular repair
Intoduction
Aneurysms of the extracranial internal artery (ICA) are rare and accountable for about 1% of all cerebral anerysms [1,2], it's an uncommon patology, reported in literature as individual case or small series. In 67%, the aneurysm involved ICA, 32% the common carotid artery (CCA) bifurcation and 1% the external carotid artery (ECA) [3]. The definition of extracranial carotid artery aneurysm ic unclear, it has been suggested to define it as the permanent dilatation on the bulbus greater than 200% of the diameter of normal ICA or greater 150% of the diameter of the normal CCA [4,5]. Aneurysm of extracranial carotid artery etiology is diverse and ranges from athrosclerosis, infection, fibromuscolar dysplasia, connettive tissue desease to traumatic or spontaneous dissection, patch pseudoaneurysm from prior repair [2,3]. May present at any location along carotid arterery, but true aneurysms more frequently occur at the carotid bifurcation and proximal ICA, whereas psudoanerysm tend to present near suture lines or area of trauma [2].
Like other peripheral aneurysm, rupture and thrombo-embolism are two major risk of aneurysm of ICA, wich may lead to acute ischaemic attacks and strokes. Other symptoms and signs can be cervical masses and pain, but in the era of modern imaging, many asymptomatic aneurysm are discovered incidentally [3,6].
Since the first reported successful treatment of a carotid artery aneurysm by Sir Astley Cooper in 1808, in which he ligated the proximal carotid artery, there have been multiple treatments options that include medical therapy, open surgical therapy, and endovascular therapy. In 1956, Dimtza performed the first resection of the carotid artery for aneurysm disease [7]. Aneurysm resection with arterial reconstruction is generally considered the standard operation because it is a definitive and durable repair, even if intra operative cranial nerve injury is not rare [1-3,6].
Medical therapy of carotid aneurysms has mostly been derived from the Mayo Clinic experience. Fankhauser and colleagues examined 141 carotid aneurysms diagnosed in 132 patients over 15-year period in Mayo Clinic. 11 Seventy-five aneurysms were treated nonoperatively. Treatment included antiplatelet therapy, anticoagulation, or serial imaging per the treating clinician. Most of the patients were asymptomatic and were in patients that had prior imaging showing stability to the aneurysm. During the study period, none of the patients treated medically died or suffered major morbidity related to the aneurysm. One did have significant growth but nonsurgical intervention was elected due to the patients' age [7].
Open surgical approaches vary depending on anatomy and underlying pathology. Attigah, et al. proposed a morphological classification of extracranial artery aneurysm and different surgical therapeutic modalities in accordance with each lesion type: type I: Isolated and short aneurysms of the ICA above the carotid bulb can almost resected and an end-to-end anastomosis; type II: long aneurysms of the ICA, ranging from the carotid bulb up to the line of Blaisdell (line between mastoid process and angle of the mandible): Can be reconstructed by vein or Dacron-graft interposition; Type III: Aneurysms of the proximal ICA and the carotid bifurcation can be locally resected and then reconstructed by aneurysmorrhaphy, patch angioplasty or a Dacron graft; type IV: Aneurysms involving the CCA and ICA as type III, but extending far more distally and proximally, can be treated by vein grafts. Type V: isolated aneurysms of the CCA, can be reconstructed with Dacron grafts [8]. Moreau and associates reported only 2.6% perioperative mortality, yet 26% of all surgically treated patients had cranial nerve palsy. Hertzer indicated that although rate of stroke is only 4% in his experience, the incidence of cranial nerve dysfunction approaching 44% [9]. The combinated risk of mortality and major stroke risk for open surgery is approximately 9%, a minor stroke incidence of 1.5%, incidence of cranial nerve injury, as noted by clinical examination, was 6% according to the Texas Heart Institute experience [10]. Cranial nerve injuries include facial, vagus, spinal accessory, hypoglossal, and glossopharyngeal nerves. To reduce risk of embolization, meticulous dissection as one would do during carotid endarterectomy is suggested along with minimal manipulation of the aneurysm [7].
Multiple endovascular modalities are described in literature, spanning from covered stenting, flow-diverting stenting, bare metal stenting, stent assisted coil embolization. Reported benefits of endovascular repmanagement: Av to avoid hostile surgical field caused by pior sugery or radiation therapy, to provide easier access to more proximal or distal lesions, avoidance cranial nerve injury, the procedure can be performed under local anesthesia, shorter hospitalization. Faries, et al. reported no perioperative and postoperative complications [2].
Although information regarding the best treatment is scarce [11], but the goal of therapy is to prevent local mass effect, rupture, and neurologic deficits from either embolization or thrombosis.
Presentation of the Case
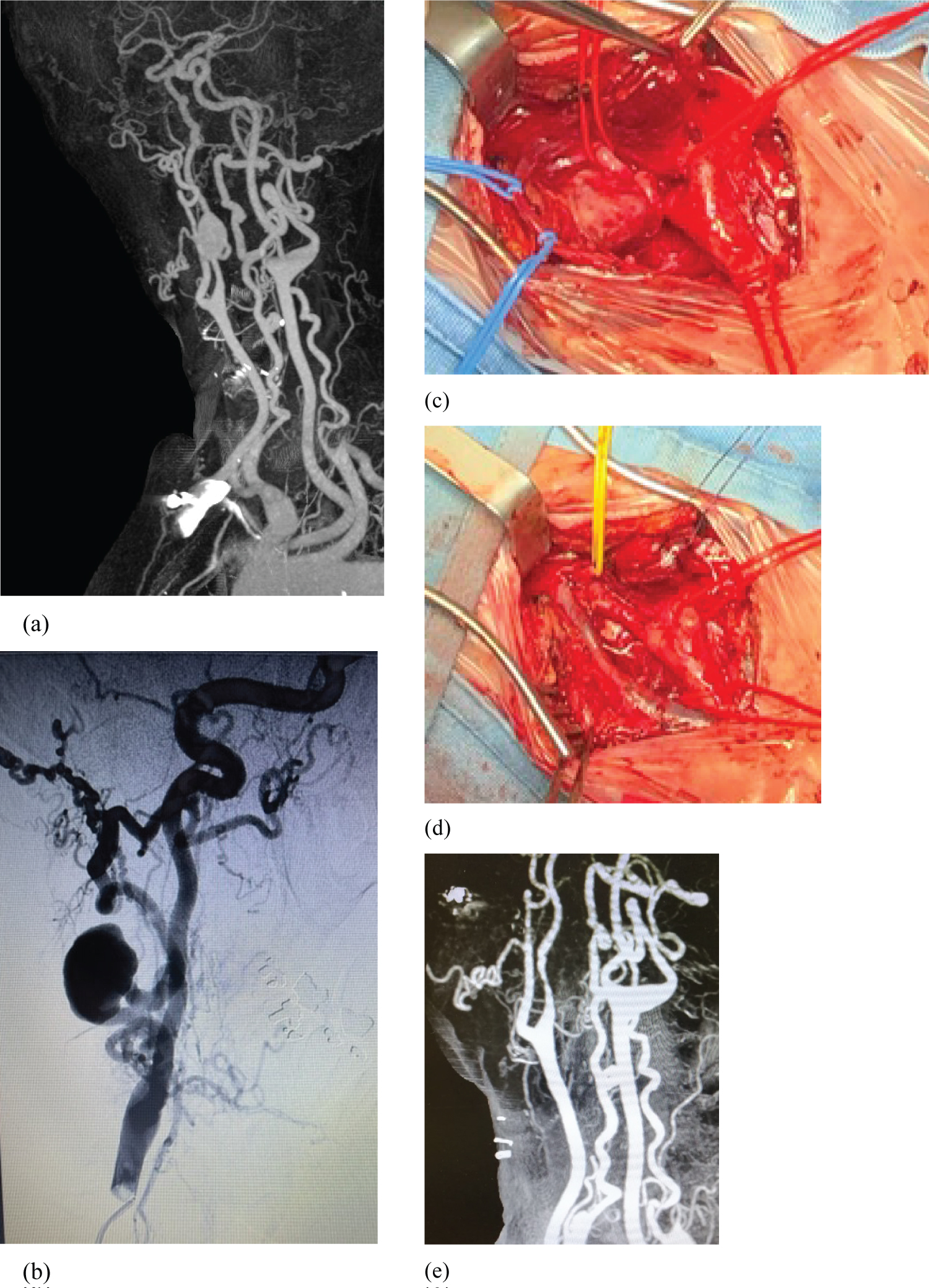
A 57-year-old woman, non smoker, previusly healty, without medical history, no family history of aneurysm war reported, denied any antecedent trauma or infection. She presented passing diplopia and distesthesia at right half face. So the patient underwent a duplex ultrasound that revealed a saccular aneurysm of right ICA (32 mm in diameter, without mural thrombi), situated about at 2 cm from common carotid artery bufurcation. CT angiography confirmed the diagnosis showed an anatomical tortuous path, the patency of distal ICA that presents an extracranial kinking (Figure 1). The study CT of intracranial arteries was negative, negative also cerebral CT. Laboratory data of peripheral blood revealed no sign of inflammation.
The first approach was endovascular, without results because a difficult signing of ICA downstream aneurysm. So, surgery was performed with general endotracheal anesthesia, through a right lateral cervical incision. A careful surgical exposure of carotid aneurysm was performed; internal giugular vein, common carotid artery, external carotid artery, internal carotid artery, hipoglossal nerve were selectively underlying by vessel loop. 5000 UI of sodic heparin was adminstred before clamping. The resection of the aneurysm was done, the ICA ends were bevelet to the appropriate lenght and anastomosed in an end to end fashion with a running 6/0 Prolene suture, without tension. It was not possible use the shunt, because the distal trait of ICA had a diametre about 5-6 mm and it presented a suboccludent stenosis immediatly next the exit of the aneurys. The clamping time was of 21 minutes. The procedure was performed under general anesthesia conducted in target controlled infusion with propofol and remifentanil, monitored by bilateral bispectral index (BIS). Cerebral protection against clamping was obtained constantly mantaining mean arterial pressure a 10% higher than baseline with low doses of norepinephrine.
Supplemental intravenous anesthesia with thiopental, up to burst suppression guided by BIS monitor, lowered brain metabolism and O2 demand.
The postoperative course was uneventful. A postoperative CT angiography showed a regular patency of ICA. The patient was discharged on postoperative day 4 with ASA 100 mg/die. Any neurological symptoms has been observed at 4 weeks after surgery, duplex scan demostrated patency of ICA, with anstomotic stenosis of 30% without flow alterations.
Histological examination of aneurysm wall revealed a degeneration of media lamina, a typical appearance of non complicated atherosclerosis.
Discussion
The available information on extracranial carotid artery aneurysm treatment in the literature suffers greatly because of its rarity, from small cases series, missing data, publication bias [12]. Also exact treatment remains uncertain and no guidelines are available [5].
However, despire is rarity, carotid aneurysms can cause cerebral complication potentially serious due to thormboembolism or local compressione of vagus nerve, recurrent laryngeal nerve or facial nerve, but the natural course is still hardly understood [12].
The treatment of ICA aneurysms can have many choices: Medical therapy endovascular, open surgery. Treatment options depend primarily on the local aneurysm anatomy and morfology and simptoms. Nonoperative treatment, which comprises antiplatelet therapy or and regular follow up, is safe in selected asymptomatic patients and can occur after dissection in the carotid artery or in patients with generalized atherosclerotic disease. In these situation, medial therapy has long been used and scientifically substained [12]. Endovascular treatement has become more popular, using nitinol bare metal stent, covered stent, flow-diverting braided stents (only if the adjacent ICA had diameter > 5 mm) or covered stent. Small case series have reported favorable procedural results, mainly because avoids nerve injuries [2,12]. Furthermore, there are situation in which endovascular repair may be not an option forfor extracranial ICA aneurysm: Patients with sign of infected aneurysm, patients with significantly challenging arch anatomy owing to take off of major branches or calcification and is well documented incidence of spontaneous thrombosis of covered stents in cerebral circulation despite anticoagulation. The data about endovascular option for extracranial ICA aneurysm are relately scarce without much long term follow up [2,3]. Open surgery with resection of the aneurysm and arterial reconstruction is generally considered the standard operation [5,7], even if intra-operative cranial nerve injury is not rare. In according to litterarure occurs transiently in 11-22% of the cases, permanetly in 3-13% of patients. Only a few studies provide information in late neurological complication after reconstruction: About 80% of the operated patients remain neurologically free symptom in follow up [8].
Conclusion
We reported a rare case of saccular ICA aneurysm, open surgical treated eith complete resection and end-to-end anastomosis without complication peri and postoperative. Surgical repair can be safe and effective solution to treat extracranial ICA aneurysm, however the choice of treatment should be evaluated time by time, according to symptoms of patients and comorbities but, mostly, to the aneurysm conformation.
Larger experience and randomized trials are needed in order to definitively assess the best approach and technical details to treat extracranial ICA aneurysm.
References
- Omran S, Raude BH, Muller V, et al. (2021) Giant saccular aneurysm of the internal carotid artery with adesion to the vagus nerve: A case report. International Journal of Surgery Case Reports 81: 105845.
- Cornwall JW, Maximilian PNG CY, Han DK, et al. (2021) Endovascular techniques in the treatment of extracranial carotid artery aneurysm. J Vasc Surg 73: 2031-2035.
- Trubert LC, Ozdemir BA, Lounes Y, et al. (2021) Asyntomatic internal carotid aneurysm: An uncommon disease of the carotid arteries. Ann Vasc Surg 70: 570.e1-570.e5.
- de Jong KP, Zondervan PE, van Urk H (1989) A new method of quantifying extracranial carotid artery aneurysms. J Vasc Surg 10: 103-104.
- Johnston KW, Rutherford RB, Tilson MD, et al. (2015) Suggested standards for reporting on arterial aneurysm. J Vasc Surg 61: 389-393.
- Xue S, Tang X, Zaho G, et al. (2000) Contemporary outcomes of open and endovascular intervention for extracranial carotid artery aneurysms: A single centre experience. Eur J Vasc Endovasc Surg 60: 347-354.
- Kraemer CJK, Zhou W (2019) Carotid Aneurysm Review. Int J Angiol 28: 17-19.
- Attigah N, Kulkens S, Zausig N, et al. (2009) Surgical therapy of extracranial carotid artery Aneurysms: Long-Term Results over a 24-year period. Eur J Vasc Endovasc Surg 37: 127-133.
- Zhou W, Lin PH, Bush RL, et al. (2006) Carotidartery aneurysm: Evolution of management over two decades. J Vasc Surg 43: 493-496.
- El Sabrout R, Cooley DA (2000) Extracranial carotid artery aneurysms: Texas Heart Institute experience. J Vasc Surg 31: 702-712.
- Robaldo A, Persi F, Trucco A, et al. (2021) Athrosclerotic saccular aneurysm of the extracranial internal carotid artery: Surgical repair. Annals of Medicine and Surgery 65: 102321.
- Welleweerd JC, den Ruijter HM, Nelissen BGL, et al. (2015) Borst Management of extracranial carotid artery aneurysm. Eur J Vasc Endovasc Surg 50: 141-147.
Corresponding Author
Laura Nicolai, MD, PhD, Cardiovascular Department, AULSS Marca Trevigiana, via Sant'Ambrogio di Fiera, 37-31100 Treviso, Italy.
Copyright
© 2022 Nicolai L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.