Surgeon-Performed Ultrasound in Preoperative Parathyroid Localization: A Real-World Experience in a Community Hospital
Abstract
Introduction: Primary hyperparathyroidism (PHPT) is an endocrine disorder which is only curable with the surgical removal of the hyperfunctioning parathyroid gland(s). Surgeon-performed Ultrasound (SUS) has been shown to be an accurate and instrumental tool in preoperative parathyroid localization and can improve patient outcomes. This study aims to report on real-world experience from a community-based hospital on preoperative SUS in comparison to Radiology-performed US (RUS).
Methods: Out of 53 patients who underwent parathyroidectomy between December 2020 and July 2023, 37 patients who had combined SUS and RUS were analyzed.
Results: RUS had an accuracy of 13.5% compared to SUS accuracy of 76%. Sestamibi scan increased accuracy to 96%. The further exploration of this topic is essential to create a more standard and accurate process in which to localize and surgically treat parathyroid adenomas in a community-hospital setting.
Conclusion: Preoperative localization of parathyroid adenoma in PHPT is accurate in the hands of experienced surgeon. The need for a more standardized approach and education of ultra-sonographers is of utmost importance in a community-hospital setting.
Introduction
Primary hyperparathyroidism (PHPT) is a common disorder with an estimated prevalence of 1 to 7 cases per 1,000 persons [1-3]. The incidence of PHPT is highest in the seventh decade of life, and it is more common in postmenopausal women, in whom the prevalence is as high as 3.2% [4].
PHPT can be cured by surgical removal of parathyroid gland(s). Conventional four-gland neck exploration and identification of all parathyroid glands and removal of abnormal ones is the accepted standard of care. Recently, however, there has evolved a paradigm of limited surgical exploration, wherein only the enlarged and hyperfunctioning gland(s) is approached, exposed, and removed. Although both four-gland neck exploration and limited surgical exploration have a valid role in appropriately selected patients, the targeted approach has a comparable cure rate in addition to limiting exploration to one side, hence less perioperative complications [5,6]. The success of a focused approach is determined by preoperative identification of abnormally enlarged or hyperfunctioning parathyroid adenoma. Multiple modalities for preoperative localization have been utilized such as 99m Tc-MIBI, computed tomography (CT) scan, magnetic resonance imaging (MRI), single photon emission computed tomography (SPECT), and ultrasound (US).
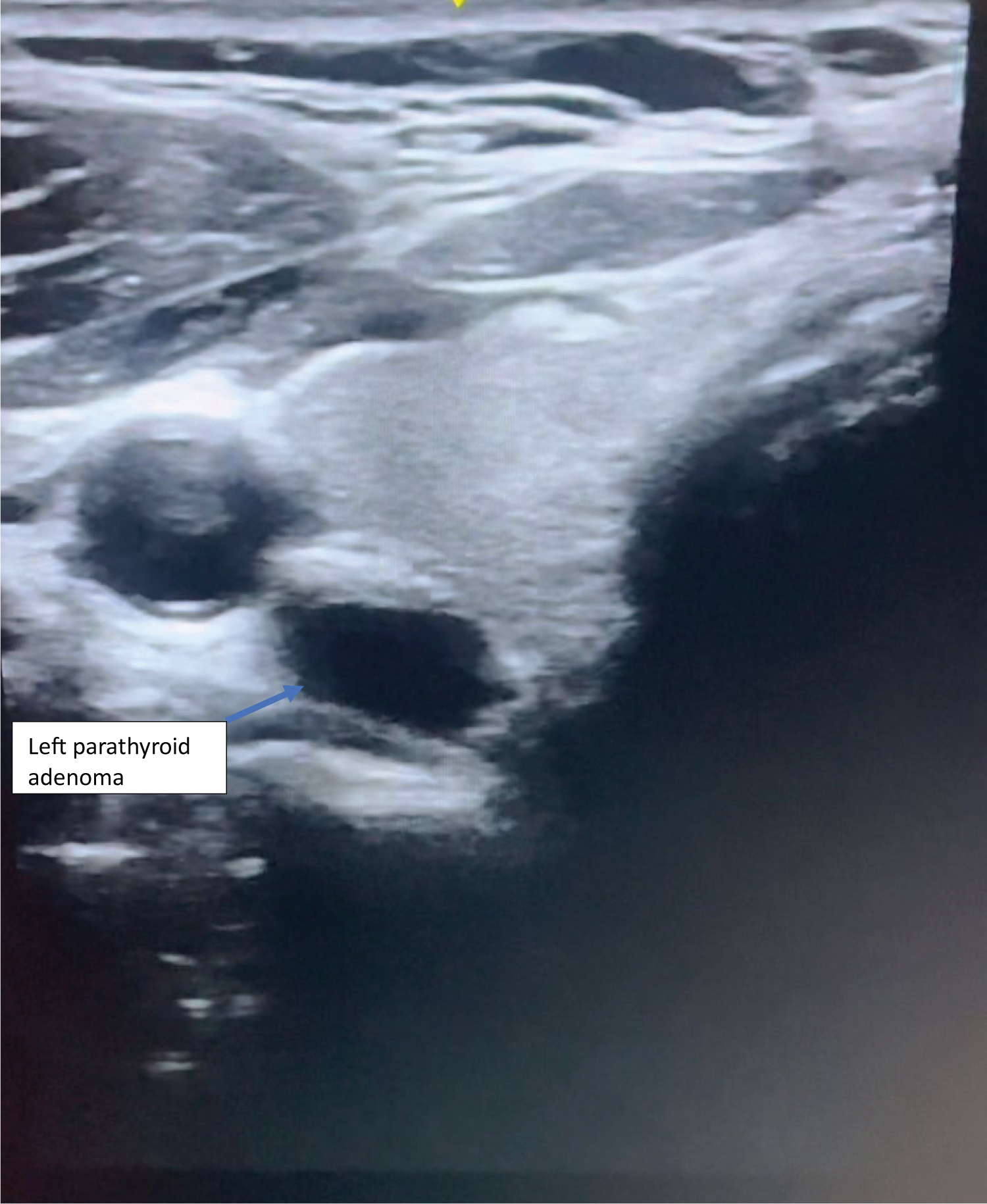
US offers the advantages of the avoidance of ionizing radiation and the ability to perform a study portably and repeatedly at a low-cost. US is an operator-dependent imaging modality and several studies have demonstrated higher accuracy in the hands of surgeons [7-10]. The anatomical expertise of the Surgeon may correlate to the greater accuracy of parathyroid localization [10]. Surgeon-performed Ultrasound (SUS) can also allow for simultaneous surgical planning. This practice approach has highlighted discrepancies of localization and number of parathyroid adenomas reported between pre-consultation Radiology department performed US (RUS) and SUS (Figure 1) [4,11,12].
Our study was conducted to assess the accuracy of surgeon-performed office US from a community-based hospital, reflecting on real-world experience.
Methods
This was an observational study of a prospectively collected data over the period from December 2020 to July 2023. All consecutive adult patients who underwent either a minimally invasive parathyroidectomy or a four-gland exploration for PHPT, at a community-based hospital were included. Surgery was performed by a single parathyroid surgeon. Exclusion criteria included patients with secondary or tertiary hyperparathyroidism and patients undergoing revision surgery or patients who did not have independent combined SUS and RUS.
Data regarding SUS were recorded at the initial encounter in the clinic, preoperative imaging and histology collected from office notes, and pathology reports. Data obtained included patient demographic information, serum parathyroid hormone (PTH), serum adjusted calcium levels, and pre-operative imaging results.
SUS was performed using the high-resolution US system (General Electric Logiq p9) equipped with high frequency linear-array transducer (14 MHz). The surgeon was blinded to the results of any prior pre-operative RUS and SS. SUS was carried out with the patient in supine position, the neck hyperextended with the aid of shoulder roll. The neck was screened systematically between the carotid arteries laterally, the sternal notch inferiorly and the carotid bifurcation superiorly.
We reviewed the reports of RUS and correlated them to the intraoperative findings and the outcome. Patients underwent either focused or four-gland explorations depending on the intraoperative findings and PTH drop (adhering with the Miami criteria > 50% intraoperative PTH drop at 10 minutes post-adenoma excision from baseline).
Operative findings and pathology reports were compared with pre-operative imaging and SUS scan to compare accuracy in localizing a parathyroid adenoma.
Statistical analysis
Analysis was completed using the IBM SPSS Analytics 18 software (Chicago, Ill., USA), and included analysis for independent association of each imaging modality with surgical findings. Basic demographics were reported as mean with standard deviation or median with interquartile ranges.
Results
Out of fifty-one patients who underwent parathyroidectomy for PHPT, thirty-seven patients underwent combined preoperative SUS and RUS. The median age at presentation was 64-years-old [range: 35-88], with female gender preponderance (65%). Two patients (5%) had family history of PHPT with no other features suggestive of syndromic hyperparathyroidism. On presentation, the median serum adjusted Calcium was 10.8 mg/dl [interquartile range: 10.6-11.25], median PTH of 119.8 pg/ml [interquartile range: 97.6-1174.2] and median 1,25 OH-Vitamin D of 26.4 mg/dl [interquartile range: 23.0-32.3] (Table 1).
Preoperative RUS identified a suspicious parathyroid adenoma in 7 patients, of which 5 were concordant with the intraoperative surgical findings, which translates into a sensitivity of 18.9% and accuracy of 13.5%. SUS identified suspicious parathyroid adenoma in 34 patients, of which 28 were concordant with the intraoperative surgical findings. This translates into sensitivity of 92% and accuracy of 75.6%. Sestamibi scan (SS) was performed in 36 patients, of which it suggested retained 99m Technetium in 20 patients, of which 18 correlated with the intraoperative surgical findings, which translates into an accuracy of 50% (Table 2).
Out of the 9 patients who did not localize on SUS, 5 patients had a suspicious lesion on SS which was concordant with surgical findings. Combined SUS and SS accurately predicted the correct parathyroid adenoma in 33 patients. This translates to an accuracy of 92% (Table 3).
Thirty-six patients (97%) were cured with normal serum calcium and normal PTH at median follow up of 22 months. Only one patient had persistent disease after four-gland cervical exploration.
In one patient, SUS was confounded for an esophageal diverticulum, Who eventually, underwent a remote staged exploration of the contralateral side at which time the adenoma was identified and removed.
In 3 patients (8%) who had double adenoma, only one abnormal gland was identified on preoperative SUS and none on RUS.
Discussion
The success of focused parathyroidectomy is greatly influenced by accurate preoperative imaging. Multiple studies have demonstrated the usefulness and accuracy of SUS, and it has been introduced into the arsenal of tools of endocrine surgeons to help localize abnormal parathyroid adenomas. Training courses for neck ultrasound have been offered during surgical society meetings such as the American Association of Endocrine Surgeons yearly conference.
In addition to many advantages, SUS offers evaluation from the surgeon’s perspective: Anatomic configuration, relationship to the adjacent structures, and size of the abnormal gland; all potentially relevant to the subsequent surgical exploration. It is also ideal for the definition of concomitant thyroid pathology which, in one series, was present in more than half of patients with PHPT being evaluated for surgery and changed the operative plan in almost 20% of cases [13].
In our cohort, we find SUS is highly accurate and comparable to the literature. Soon, et al., demonstrated an accuracy of 83% for SUS [14], and, when compared to RUS, Thomas, et al., reported a higher SUS accuracy (90.1% vs. 80.1%) [15]. When utilizing combined SS and SUS, we report a higher detection rate accuracy of 92%, as compared to 75% with SUS alone or 50% with SS alone. This is in line with literature; De Feo, et al., reported a higher sensitivity of combined SS and US (96%) compared to the use of SS (71%) or US (67%) alone [16].
RUS sensitivity and accuracy were lower than the reported literature and significantly different than the SUS. RUS were all performed by technicians, and upon reviewing the false negative images by an independent radiologist, we found concordance with the original reports, which highlights a poor technique in image acquisition. There are several medical societies that have produced practice guidelines for parathyroid evaluation with Ultrasound. The American Institute of Ultrasound in Medicine and the American College of Radiology follow similar practice guideline for the performance parathyroid ultrasound examination. These guidelines recommend the patient’s neck be hyperextended during evaluation with longitudinal images taken between the right and left carotid arteries and transverse images from the carotid bifurcation to the thoracic inlet. It is also recommended to examine below the clavicle or in the mediastinum for enlarge inferior parathyroid glands. With these inferior glands it is advised to use angling of the probe and a tightly curved array transducer which can aid in diagnosis of these glands. It also states that 1 to 3% of parathyroid adenomas are infrahyoid and that these ectopic glands can sometimes be visualized better with having the patient swallow or turning their head away from the site of examination. It is suggested that swallowing, gentle compression of ultrasound transducer, and addition of color doppler imaging are methods that may improve visualization of parathyroid glands [17-19].
We suggest further training of ultra-sonographers in this disease, normal anatomic sites of enlarged parathyroid adenoma and the potential ectopic sites. We suggest a stepwise approach for US reporting where the anatomic locations of potential abnormal parathyroid glands would be screened and illustrated objectively abiding by different medical societies listed above.
The limitations of this study are a small sample size; however, considering the significant difference in outcome between RUS and SUS, these findings suggest a trend that is worth investigating and reporting.
Conclusion
Preoperative localization of parathyroid adenoma in PHPT is highly accurate in the hands of experienced surgeons. The need for a more standardized approach and education of ultra-sonographers is of utmost importance in a community-hospital setting.
References
- Yeh MW, Ituarte PH, Zhou HC, et al. (2013) Incidence and prevalence of primary hyperparathyroidism in a racially mixed population. J Clin Endocrinol Metab 98: 1122-1129.
- Adami S, Marcocci C, Gatti D (2002) Epidemiology of primary hyperparathyroidism in Europe. J Bone Miner Res 17: N18-N23.
- Wermers RA, Khosla S, Atkinson EJ, et al. (1997) The rise and fall of primary hyperparathyroidism: A population-based study in Rochester, Minnesota, 1965-1992. Ann Intern Med 126: 433-440.
- Lundgren E, Hagström EG, Lundin J, et al. (2002) Primary hyperparathyroidism revisited in menopausal women with serum calcium in the upper normal range at population-based screening 8 years ago. World J Surg 26: 931-936.
- Steward DL, Danielson GP, Afman CE, et al. (2009) Parathyroid adenoma localization: Surgeon-performed ultrasound versus sestamibi. Laryngoscope 116: 1380-1384.
- Choi JH, Jayaram A, Bresnahan E, et al. (2022) The role of surgeon-performed office and preincision ultrasounds in localization of parathyroid adenomas in primary hyperparathyroidism. Endocr Pract 28: 660-666.
- Jabiev AA, Lew JI, Solorzano CC (2009) Surgeon-performed ultrasound: A single institution experience in parathyroid localization. Surgery 146: 569-575.
- Kairys JC, Daskalakis C, Weigel RJ (2006) Surgeon-performed ultrasound for preoperative localization of abnormal parathyroid glands in patients with primary hyperparathyroidism. World J Surg 30: 1658-1663.
- Van Husen R, Kim LT (2004) Accuracy of surgeon-performed ultrasound in parathyroid localization. World J Surg 28: 1122-1126.
- Aspinall SR, Nicholson S, Bliss RD, et al. (2012) The impact of surgeon-based ultrasonography for parathyroid disease on a British endocrine surgical practice. Ann R Coll Surg Engl 94: 17-22.
- Starker LF, Fonseca AL, Carling T, et al. (2011) Minimally invasive parathyroidectomy. Int J Endocrinol 2011: 206502.
- Udelsman R, Lin Z, Donovan P (2011) The superiority of minimally invasive parathyroidectomy based on 1650 consecutive patients with primary hyperparathyroidism. Ann Surg 253: 585-591.
- Shalaby M, Hadedeya D, Lee GS, et al. (2020) Im0pact of surgeon-performed ultrasound on treatment of thyroid cancer patients. Am Surg 86: 1148-1152.
- Soon PS, Delbridge LW, Sywak MS, et al. (2008) Surgeon performed ultrasound facilitates minimally invasive parathyroidectomy by the focused lateral mini-incision approach. World J Surg 32: 766-771.
- Thomas PR, Beggs AD, Han TS (2019) Utility of surgeon-performed pre-operative ultrasound in the localisation of parathyroid adenomas. JRSM Cardiovascular Disease 8: 1-7.
- De Feo ML, Colagrande S, Biagini C, et al. (2000) Parathyroid glands: Combination of (99m)Tc MIBI scintigraphy and US for demonstration of parathyroid glands and nodules. Radiology 214: 393-402.
- (2023) AIUM practice parameter for the performance and interpretation of diagnostic ultrasound of the thyroid and extracranial head and Neck. J Ultrasound Med 42: E55-E62.
- (2018) Aium-ACR-SPR-sru practice parameter for the performance and interpretation of a diagnostic ultrasound examination of the extracranial head and Neck. J Ultrasound Med 37: E6-E12.
- Petranovic Ovcaricek P, Giovanella L, Carrió Gasset I, et al. (2021) The EANM practice guidelines for parathyroid imaging. Eur J Nucl Med Mol Imaging 48: 2801-2822.
Corresponding Author
Mustapha El Lakis, MD, FACS, General Surgery Department, University of Pittsburgh Medical Center, Pittsburgh, PA, USA.
Copyright
© 2024 El Lakis M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.