Large Mediastinal Ectopic Parathyroid Adenoma Causing Malignant Hypercalcemia in a Young Female: A Case Report and Review of Literature
Abstract
Ectopic parathyroid tissue can pose difficulties in diagnosis and management of patients with hyperparathyroidism. Due to the embryological origins of the inferior parathyroid glands from the 3rd pharyngeal arch where they develop with the thymus; they can have variable anatomical locations, including the anterior mediastinum. While the incidence of ectopic parathyroid glands varies in the literature mediastinal parathyroid tissue is extremely rare. This anatomical variation has important diagnostic and surgical ramifications for patients and is an important topic for trainees in medical endocrinology, endocrine surgery and cardiothoracic surgery to be aware of. We present the case of a 22-year-old woman who presented as an emergency with severe hypercalcaemia. Who was subsequently found to have an ectopic mediastinal parathyroid adenoma. She underwent surgery within days of her initial presentation providing her with an immediate cure and restoring her calcium homeostasis. Despite diagnostic and operative challenges, combined care from our endocrine and cardio-thoracic surgical teams ensured an uneventful post-operative recovery for this patient.
Keywords
Parathyroid adenoma, Ectopic, Mediastinal parathyroidectomy
Introduction
Parathyroid glands are endocrine organs that release parathyroid hormone into the blood stream to regulate calcium homeostasis within the body. Its actions in the body, in response to low serum calcium, are three-folds: It acts on the osteochondrocytes to create an efflux of calcium from bone; it acts on the renal tubule to increase calcium reabsorption in urine and decrease phosphorous reabsorption and increases the activation of vitamin D; it acts on the gastrointestinal system to increase calcium and phosphorous absorption. Primary hyperparathyroidism occurs when any/all of these glands become overactive and they lose the negative feedback response to normal serum calcium, producing inappropriately high levels of parathyroid hormone. This results in extremely high serum calcium levels. The patient may experience symptoms of hypercalcaemia which include, abdominal pain, bone pain, confusion, depression, kidney stones and cardiac arrhythmias. In addition, they may also have decreased bone density due to the action of parathyroid hormone on the bone.
Primary hyperparathyroidism is the most common cause of hypercalcaemia in the community and is a very important differential to include in the work-up of patients presenting with any of these symptoms. Solitary parathyroid adenoma is the most common cause of elevated parathyroid hormone, accounting for 80% of cases of primary hyperparathyroidism [1]. With most other cases being caused by multiple adenomas or by four-gland hyperplasia, these causes are more common in patients who may have rare inherited conditions such as familial hypocalciuric hypercalcaemia and multiple endocrine neoplasia type I. Very rarely (less than 1%), primary hyperparathyroidism may be due to a malignancy within a parathyroid gland.
Case Presentation
Our patient is a 22-year-old woman who presented to a peripheral hospital with five months history of oligomenorrhoea and three months history of mood disturbances. She was admitted for diagnostic work up which included full clinical examination and serology. There were no findings on initial examination which included neck examination with assessment of cervical lymph chains. Her serological results were largely within normal parameters with the only abnormality being a high Calcium of 3.52 mmol/L (normal range 2-2.5 mmol/L). Subsequently a serum PTH was performed, it returned at 401.2 pg/ml (normal range 10-55 pg/ml). Primary hyperparathyroidism and malignancy account for 80-90% of all causes of hypercalcaemia; with the former being most common in the community and the latter most common in hospitalised patients. Given these extremely abnormal results this patient was referred to our tertiary endocrine surgery department for further assessment and management.
Investigations
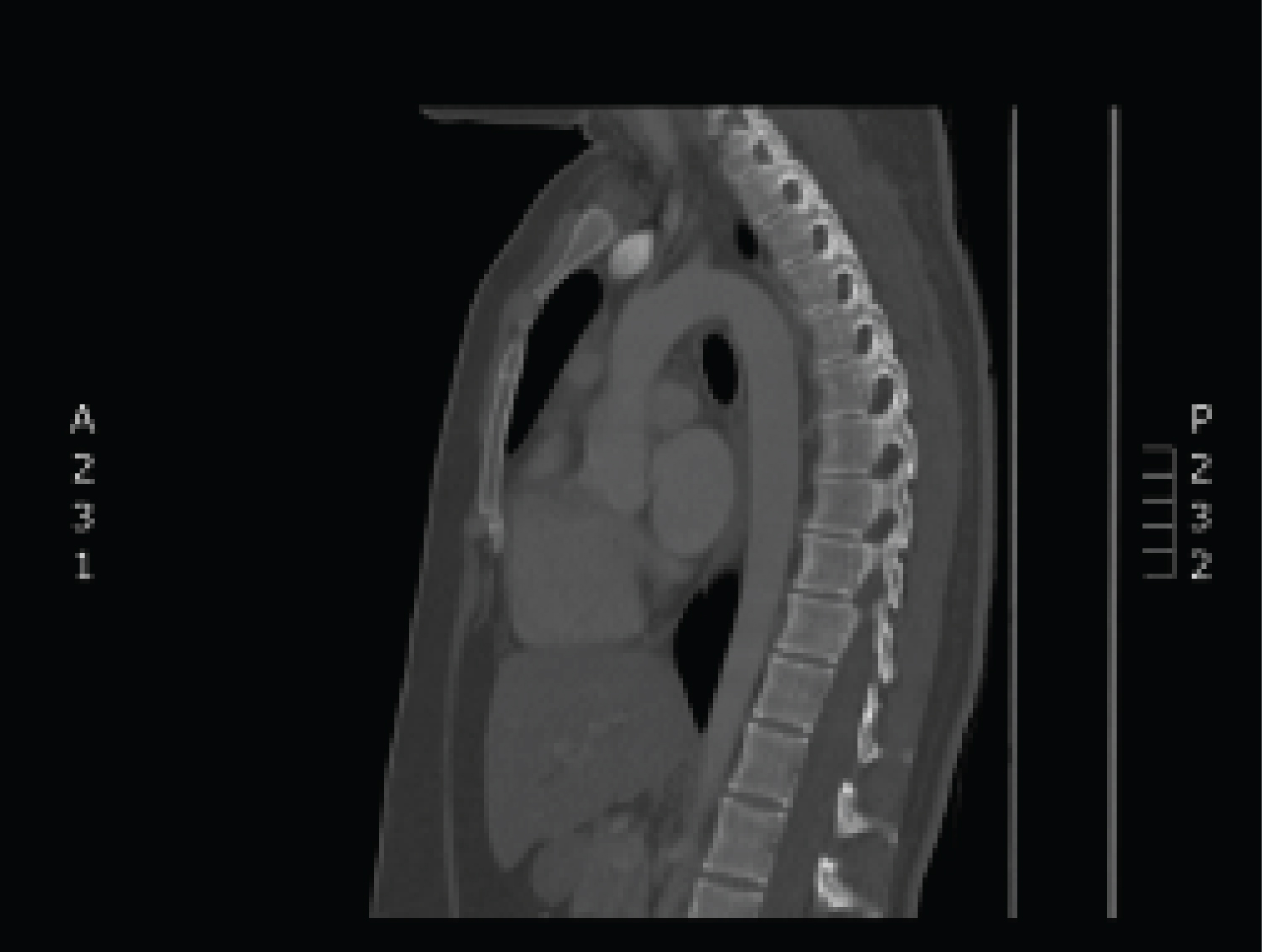
A 99mTc-sestimibi (MIBI) scan was performed which did not indicate abnormal uptake within the neck. It did show an area of increased uptake within the patient’s mediastinum (Figure 1). This required further evaluation with a CT scan of her neck and thorax. This was able to clearly delineate a lesion within the anterior mediastinum at the origin of the aortic arch (Figure 2 and Figure 3).
Procedure
There are several surgical approaches to excising the mediastinal parathyroid tissue. Open techniques such as sternal lifting [2], which involves elevating the sternum by the sternoclavicular joints to allow further dissection inferiorly, may be used for lesions within the superior mediastinum. Mini or total midline sternotomy [3] may be utilised in cases such as ours when the lesion lies deep within the thorax. There are laparoscopic approaches which can be utilised including subxiphoid, video-assisted thoracoscopy [4] and video-assisted mediastinoscopy [5] depending on the exact location of the adenoma.
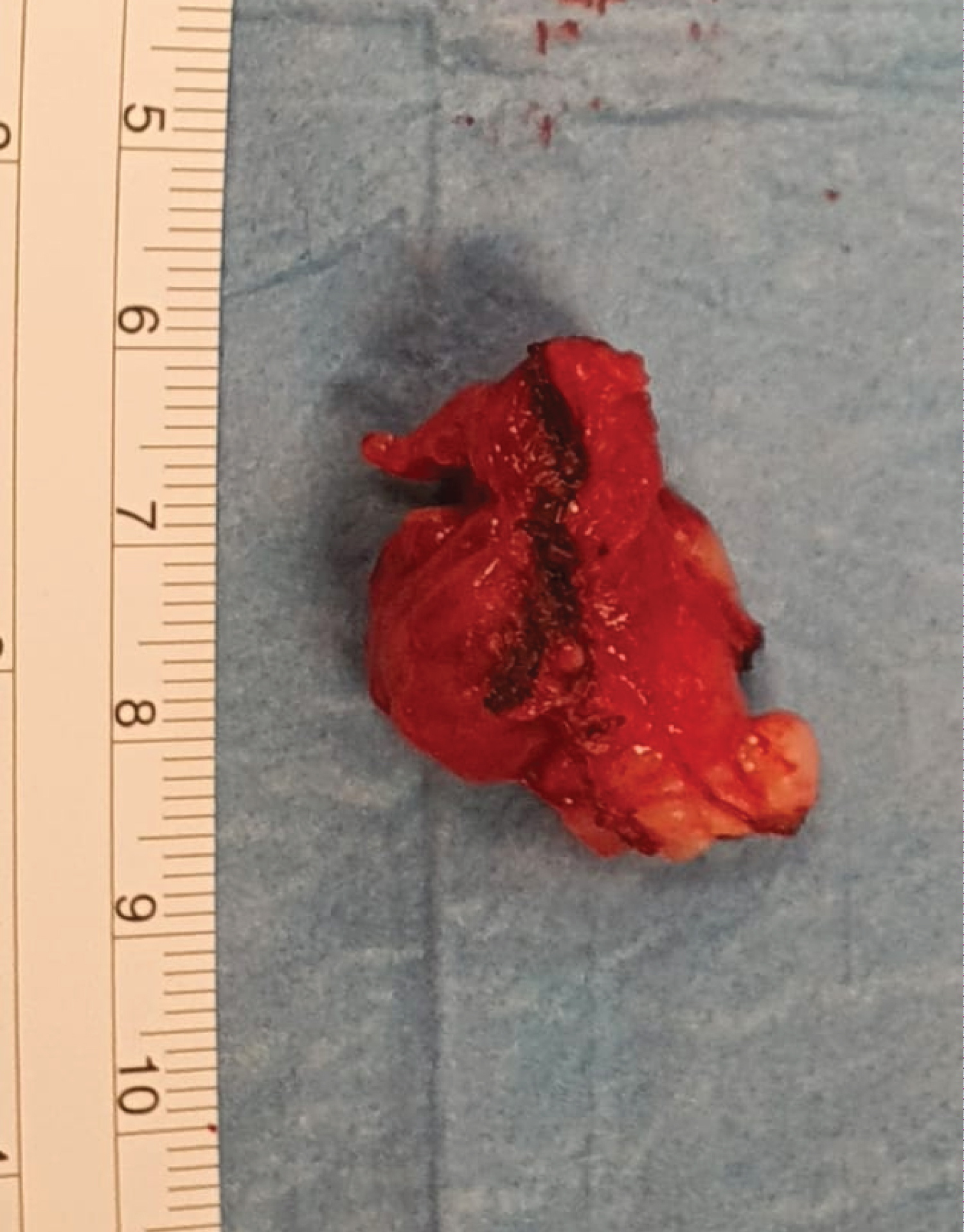
As the location of this lesion was within the anterior mediastinum and in close proximity to the heart and great vessels, we requested the assistance of the cardiothoracic surgery team in our institution. The decision was made to access the gland via a mini-midline sternotomy. This involved a midline split from sternal notch to the 3rd intercostal space. At which point the incision was extended laterally to the left and this portion of the bony thorax could be elevated to expose the lesion. The parathyroid adenoma was identified close to the thymus and was excised (Figure 4).
As with all parathyroidectomy procedures there are many techniques utilised to ensure that the target gland/tissue has been removed. All three techniques routinely performed in our institution (Intra-operative PTH assay, Gamma probe and frozen section) indicated removal of the problematic gland and no further dissection was required. These techniques are detailed below. Careful haemostasis was achieved and our cardiothoracic colleagues closed her sternotomy wound and placed a redivac drain. This was then covered with a negative pressure dressing.
Outcome and Follow Up
She had an uneventful post-operative recovery with close observation in the High Dependency Unit (HDU) for one night, she did not require post op ventilation or ICU stay. Calcium checks morning and evening for 24 hours were done and monitoring of drain output was ensured. There was 78 mls in the drain the following day. On review of a normal chest X-ray to rule out any post-operative pneumothoraces this drain was removed. Her calcium steadily reduced over the course of her recovery from 2.35 mmol/L the evening of surgery to 2.12 mmol/L on the 3rd post-operative day. She did experience some peri-oral tingling, for which she was given calcium replacement twice a day for several weeks. She was discharged on post-operative day 7 with endocrine medicine follow up to review her serological tests and ongoing need for calcium supplementation. The final histopathology was consistent with a benign enlarged parathyroid adenoma, with no evidence of malignancy.
Discussion
The parathyroid glands develop during the 4th-5th week of development from the pharyngeal arches [6]. The pouches formed between these arches give rise to a variety of endodermic tissue. The 3rd and 4th pouches are responsible for the formation of the parathyroid glands, the thymus and part of the thyroid gland. The dorsal wing of the 3rd pouch gives rise to the inferior glands, while the dorsal wing of the 4th pouch produces the superior glands. In the 7th week of gestation these glands separate from the pharyngeal wall and attach to the posterior aspect of the thyroid gland. For the inferior glands this requires them to follow the path of the descending thymus gland and can cause them to have variable anatomical locations, including within the anterior mediastinum.
Incidence of ectopic parathyroid gland varies in the literature and has been noted to be between 6-16% in disease states however there have been anatomical studies that have found rates as high as 43%. The majority being inferior glands located intrathymic, anterosuperior mediastinum intrathyroidal, within the thyrothymic ligament, submandibular [7].
Ectopic superior glands have been identified in a number of aberrant positions including the tracheoesophageal groove, retroesophageal, paraesophageal, posterosuperior mediastinum, intrathyroidal, and within the carotid sheath [7]. This has important diagnostic and surgical ramifications for patients and is an important variant for trainees in medical endocrinology, endocrine surgery, and cardiothoracic surgery to be aware of.
Comparison of localisation techniques and findings during surgery was made by Van der Harst, et al. [8] in 1994 in a cohort of 115 patients undergoing neck dissection. They reviewed ultrasound scanning, thallium-technetium subtraction scintigraphy, computed tomography (CT) and 99 3mTc-sestimibi scanning. In patients with single gland disease, they were found to have 56%, 65%, 67% and 83% sensitivity respectively. With all modalities sensitivity was reduced in multiple gland disease. It was noted that the mean weight of tumours that were not identified was lower than the weight of tumours seen on pre-operative imaging. A 2005 meta-analysis of 20,225 patients with primary hyperparathyroidism showed that sestamibi-scintigraphy was noted to have an overall sensitivity of 88% for detection of a single adenoma [9]. This decreased to 45% and 30% for patients with four-gland hyperplasia and double adenomas respectively.
In a 2006 study by Phitayakorn, et al. [7], Sestamibi scanning was shown to identify 81% of retrosternal parathyroid glands. Burke, et al. [10] reviewed two-stage Sestamibi scanning in more detail in 2013, assessing the use of early phase imaging to increase accuracy in adenoma detection and localisation. Normal parathyroid tissue should not appear on Sestamibi scanning, thyroid tissue washes out the 99mTc isotope faster than parathyroid tissue. In theory abnormal parathyroid tissue should be visible in the later stage imaging, however this may result in false negatives if washout has occurred. They were able to show that 141 of 209 non-localising scans were positive in the early phases. Localisation of abnormal parathyroid glands pre-operatively will allow for minimally invasive radio-guided parathyroidectomy reducing the risks associated with extensive and bilateral neck dissection.
Intra-operative assessment of the gland is an essential part of any parathyroidectomy procedure regardless of the location. First, we use the 20% rule, this requires the patient to undergo pre-operative radio-isotope injection (the same isotope that is used in pre-operative sestamibi scanning). Using a sterile probe, we measure the output from the background tissue and from the likely adenoma. The second technique involves intra-operative PTH-serum-assay. Given the 2.5-minute half-life of parathyroid hormone, venous blood is taken 5 minutes after the gland is removed and is measured. Finally, the gland is brought immediately to the pathology department for frozen section and a consultant pathologist relays their initial impression of the tissue to the team waiting in theatre.
The following results would be consistent with removal of the over-active gland: A 20% increase in output from the adenoma; A 50% drop in the parathyroid hormone compared to the pre-operative level, and hypercellular parathyroid tissue on frozen section.
Summary
Hypercalcaemia is a common condition that can affect patients of all age groups and demographic backgrounds. Primary hyperparathyroidism should be investigated in patients with elevated calcium levels and no history or signs of malignancy. Parathyroid adenoma is the most common cause of this condition and can be treated definitively by surgical removal of the gland. This is of huge benefit to the patient as it can restore calcium homeostasis, prevent complications associated with high calcium, and avoid the need for long-term medications. As it has been shown in this case it is important to remember the embryological origins of these glands when investigating a patient with a possible adenoma. The significant diagnostic and management implications of these anatomical variants should not be overlooked.
Author Contributions
Conceptualization: Mr Z Razzaq and Dr A Bell; Investigation: Mr H Mustafa; Methodology: Professor HP Redmond; Project Administration: Dr A Bell; Writing - Original draft preparation: Dr A Bell; Writing – Review & Editing: Dr A Bell and Mr Z Razzaq.
Authors Declaration
All authors listed have approved the paper in its current form. This work has not been previously published. There are no conflicts of interest to disclose. There was no funding received for this work.
References
- Bilezikian JP, Brandi ML, Eastell R, et al. (2014) Guidelines for the management of asymptomatic primary hyperparathyroidism: Summary statement from the Fourth International Workshop. J Clin Endocrinol Metab 99: 3561-3569.
- Ikeda Y, Sasaki Y, Miyabe R, et al. (2009) Cervical approach by lifting the superior sternum for mediastinal parathyroid adenoma. Surg Laparosc Endosc Percutan Tech 19: 78-81.
- Shpitzer T, Saute M, Gilat H, et al. (2007) Adaptation of median partial sternotomy in head and neck surgery. Am Surg 73: 1275-1278.
- Wei JP, Gadacz TR, Weisner LF, et al. (1995) The subxiphoid laparoscopic approach for resection of mediastinal parathyroid adenoma after successful localization with TC-99m-sestamibi radionuclide scan. Surg Laparosc Endosc 5: 402-406.
- Cupisti K, Dotzenrath C, Simon D, et al. (2002) Therapy of suspected intrathoracic parathyroid adenomas. Experiences using open transthoracic approach and video-assisted thoracoscopic surgery. Langenbecks Arch Surg 386: 488-493.
- Rosen RD, Bordoni B (2021) Embryology, Parathyroid.In: Stat Pearls [Internet], Treasure Island (FL): Stat Pearls Publishing.
- Phitayakorn R, McHenry CR (2006) Incidence and location of ectopic abnormal parathyroid glands. Am J Surg 191: 418-423.
- Van der Harst E, Bonjer HJ, Pols HA, et al. (1994) Preoperatieve non-invasieve lokalisatieonderzoeken van vergrote bijschildklieren bij 115 patiënten met hyperparathyreoïdie. Ned Tijdschr Geneeskd 138: 1660-1664.
- Ruda JM, Hollenbeak CS, Stack BC (2005) A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg 132: 359-372.
- Burke JF, Naraharisetty K, Schneider DF, et al. (2013) Early-phase technetium-99m sestamibi scintigraphy can improve preoperative localization in primary hyperparathyroidism. Am J Surg 205: 269-273.
Corresponding Author
Dr. Aisling Bell, MB BCh BAO MRCSI MCh, Beaumont Hospital, Beaumont Road, Dublin 9, Ireland, Tel: 00353857562374.
Copyright
© 2022 Bell A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.