Xeroderma Pigmentosum: A Defying Problem
Abstract
Three patients with xeroderma pigmentosum are presented, stressing the need for prevention (trying to avoid exposure to irradiation and namely to sun light), showing the benefits of rotation dermabrasion and showing the benefits of radical surgery through the presentation of two patients with radical surgical treatment, one of them having had a monoblock total facial skin excision (performed for the first time in the world).
Keywords
Xeroderma pigmentosum dermabrasion, Radical surgery, Facial skin replacement
Introduction and Objectives
Xeroderma pigmentosum is fortunately a rare autosomal recessive disease, resulting from a congenital anomaly of the ectoderm that reacts with hypersensitivity to any form of radiation energy. Due to that, the sun rays or any form of radiation can lead to the progressive development of skin cancer, frequently of early development, thus affecting mostly children (that, eventually, may even not attain adult life).
This pathology is considered to be one of the rare hereditary disorders, studies having shown marked multiple involved genes, genetic heterogeneity conditioning various clinical aspects and intensity of signs. There are 7 complementation groups, plus a variant form. So far hormonal and radiological studies have been within normal limits. Nevertheless EEG studies always reveal alterations, although with no fixed pattern. Psychiatric evaluation has always shown a low intellectual level that seemed to be particularly significant at older ages.
The main aim of this paper is to call attention to the possible preventive measures to be taken as much as possible, by protecting the skin surface from sun light exposure (not forgetting about clothes and large hats), to the advantage of early rotation dermabrasion and the need for immediate surgical control of all initially small lesions that will appear. Obviously, everything is based on regular and frequent clinical examinations.
Material and Methods
We present 3 of the 5 treated children:
1. A 3-years-old girl with a spindle cell carcinoma of the nose and a small basal cell carcinoma of the right malar region, treated by direct surgical excision, complemented by a 2 stage rotation dermabrasion of the face and neck and further small plastic surgery procedures.
2. A 11-years young boy with a spindle cell carcinoma of the left auricular region and invasion of the temporal bone and thus requiring its partial (although radical) removal, care being taken to preserve the facial nerve. The extensive wound remaining after radical excision of the tumor was covered by a large rotation temporal flap. That patient was later subject to a rhinoplasty, using a tubular graft obtained from the inner surface of the arm. Unfortunately, he died some years later, because of an inoperable chest wall sarcoma.
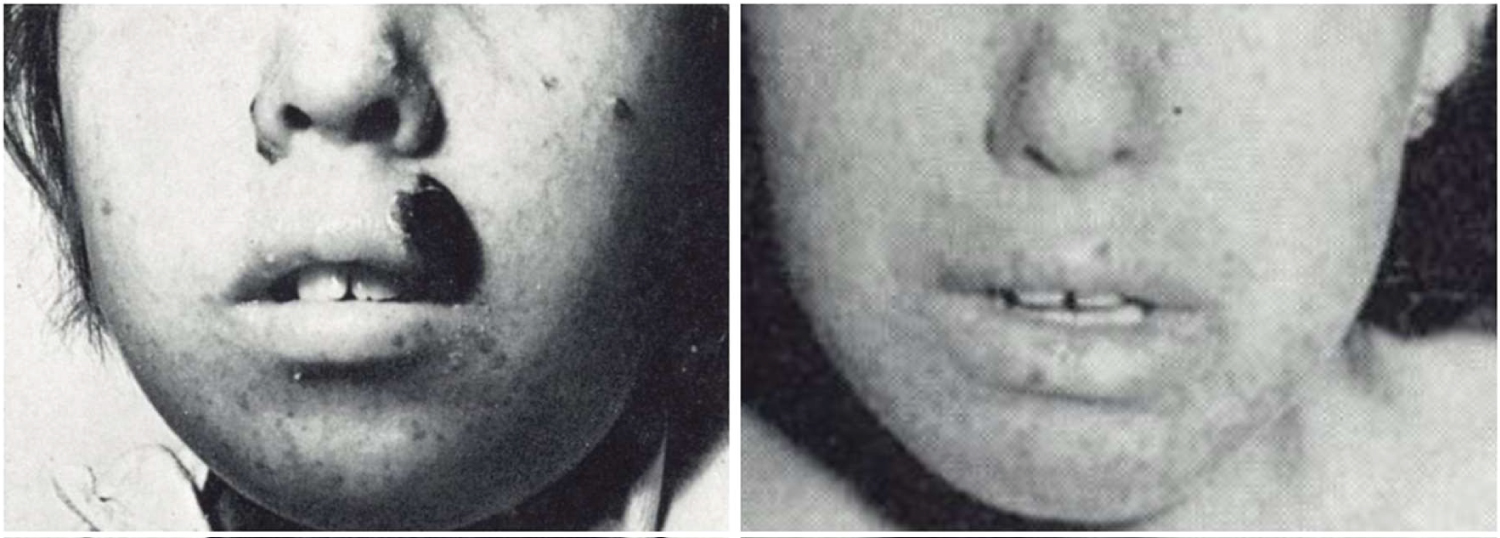
3. A 9-years young boy, son of a fisherman, and living near a beach, showed the typical distribution of the lesions in the face, hands and feet (those later ones not yet malignant). His lesions had started to increase when aged 3, after having had irradiation with ultraviolet light, because of rickets. After several small surgical interventions and the use of radiotherapy, he had infected malignant lesions disseminated all over his face as well as palpebral ectropion. It was then that it was decided to perform a surgical intervention never done before, even at world level: The one stage monoblock excision of the total facial skin [1].
Surgical Technique: (Patient Number 3)
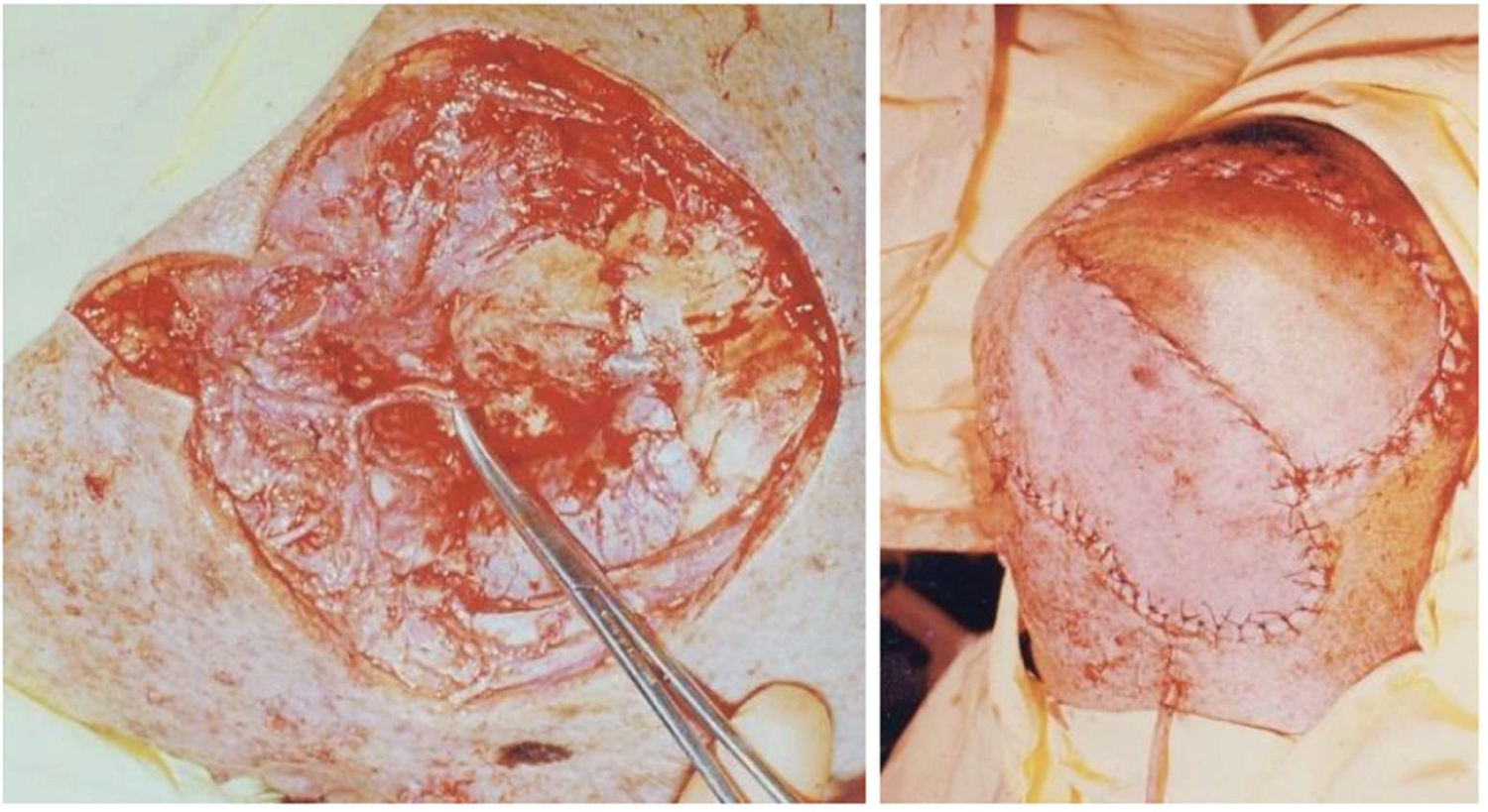
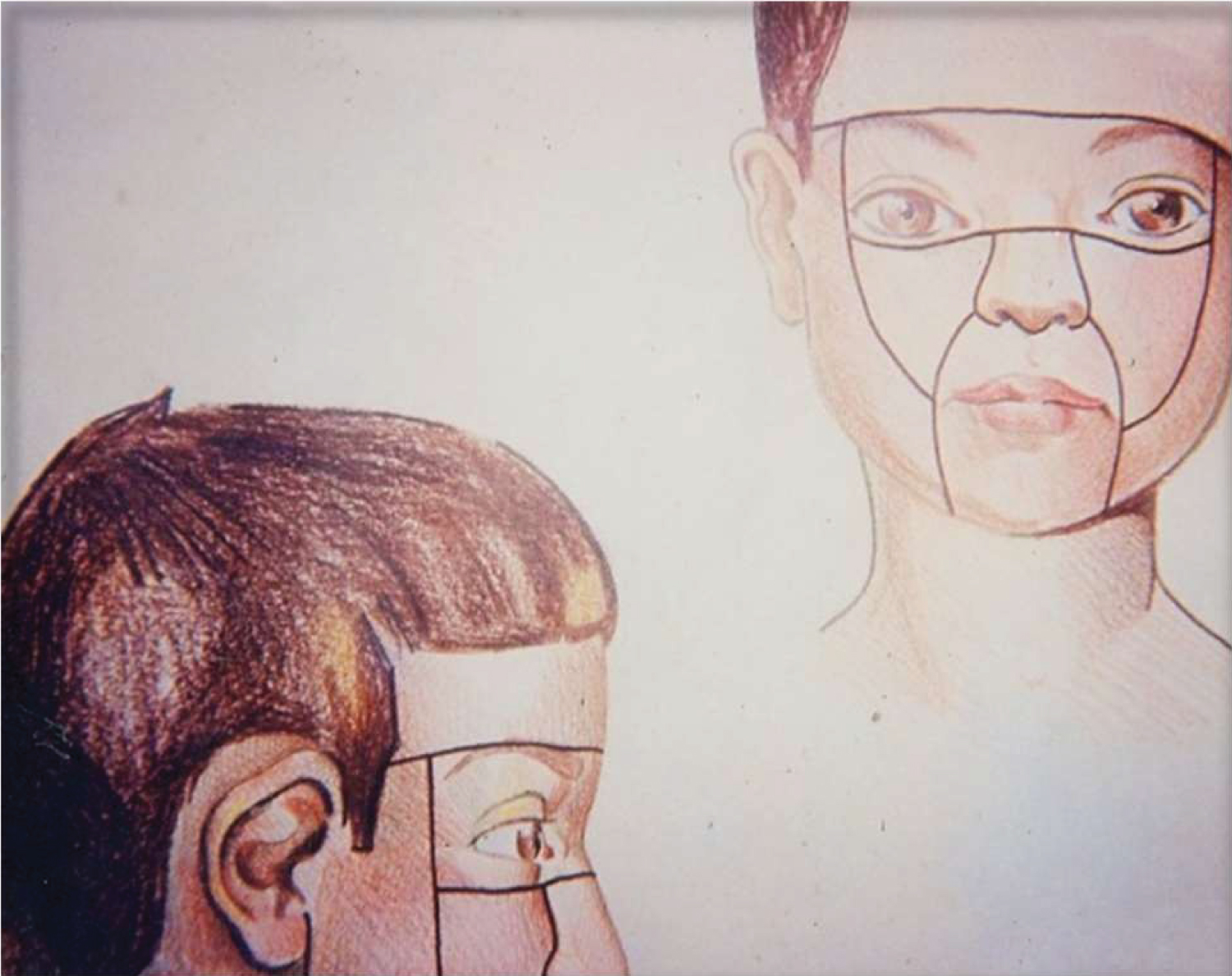
Patient, lying on his back, general anesthesia 45 was started endotracheal to change later for tracheostomy. Radical, monoblock, total facial skin resection was performed forehead, nose, red lips and lids, of which only could be saved little more that the conjunctiva). That was followed by immediate reconstruction according to the principles of the "Facial Aesthetic Units'' advised by Mário Gonzalez Ulloa, so that the lines of adjoining skin grafts would coincide with the natural skin creases. Taking into account the possibility of retraction of the skin grafts to the lids could result in lagophthalmia and ectropion, a single graft was placed in the palpebral remnants and which was maintained for 2 months (the palpebral cleft being opened then) considering the existent skin infection it was decided to use medium thickness grafts, obtained with the electric dermatome. The skin of the anterior abdominal wall was used for the mouth, so that the hole in the central part of the graft, (corresponding to the umbilicus) would correspond to the lips and open mouth. Several other plastic surgery interventions were needed, including a rhinoplasty with a tubular graft obtained from the inner part of the left arm. The treatment was completed with rotation dermabrasion of the neck.
He was kept with an occlusive dressing for 5 days and fed by a gastric tube for 3 weeks. The intervention lasted 8 hours and 1.500 ml of whole blood was administered.
Discussions and Results
The treatment of xeroderma pigmentosum must be fundamentally prophylactic, avoiding exposure to any type of irradiation, namely sun light (using adequate clothes, sun glasses and protective creams) [1] may eventually be useful in selected cases, mas will have, eventually, to be repeated several times.
Dermabrasion [1] may eventually be useful in selected cases, but will have, eventually, to be repeated several times.
Surgery is indicated in all localized or single lesions, being associated with the plastic surgery procedures usually required, as well as the excision by electrocoagulation of all the small suspected lesions suspected that may appear in the disseminated forms of the disease. The patients must be seen frequently advisably every two months and SOS Fortunately metastases seem to occur rarely, perhaps because the vascular blood supply to the skin seems to be scarce in these patients and there is an excess of fibrous tissue in the skin as a consequence of the disease itself.
Basically, on Patient number 3, one couldn't avoid having severe doubts about what to do and the common opinion of all contacted or that could be taken from the literature, was that it was a hopeless situation. It would not be correct cancer surgery (on even possible?) to perform the isolated removal of all the multiple malignant lesions (not only because of their frequent confluence and multiplicity) or an option for multiple surgical procedures. That led us to believe that the only possible solution would be the one stage monoblock excision of all the malignant and infected facial lesions, although that had never been performed in the world and, at that time, facial skin transplants (still today with extremely rare indications was not known [2-5].
One can say the aesthetic result is far from perfect. Nevertheless, function is normal and it was markedly rewarding to see the change in behavior and happiness of the patient, that changed from a fearing and suffering child to an active and happy human being.
Conclusions
Surgery was the treatment of choice. In the case of our most challenging patient we believe that monoblock total excision of the facial skin, followed by immediate skin grafting [1], was the right approach , although it had never been performed in the world (and, so far, has not been done again). The patient survived for many years, working as an employee in the lifts of the cancer institute (thus avoiding exposure to the sun rays). He died more than 20 years later from a brain tumor (Figure 1, Figure 2, Figure 3, Figure 4, Figure 5, Figure 6, Figure 7 and Figure 8).
Disclaimer
The paper is a single author piece and presents no conflict of interests.
Funding
No funding was received for this research.
Consent
Was given orally at the time of surgery (to be used on science work and also on any other work I would wish).
References
- Gentil Martins A (1965) The British Journal of Surgery Vol 52 Nº7 July 1965 Bristol: John Wright & Sons Ltd.
- Shammngarajah K, Hettarachy S, Clark A, et al. (2011) Clinical outcomes of facial transplantation: A reviews. Int J Surg 9: 600-607.
- Mark M (2005) The ethics of facial transplantation. AMA Journal of Ethics.
- Bueno E M, Diaz-Siso J R, Pomahac B, et al. (2011) A multidisciplinar protocol for face transplantation at brigham and women's hospital. J Plast Reconstr Aesthet Surg 64: 1572-1579.
- Atlas of Genetics and Cyto genetics in Oncology and Hematology Fri Apr 30 15:04:42 CEST 2021.
Corresponding Author
António Gentil Martins, MD, FICS, OLY, Departamento da Criança e Adolescente - Instituto Português de Oncologia de Lisboa, Francisco Gentil, Av. Almirante Reis 242 4º Dto. 1000-057, Lisbon, Portugal, Tel: 351-939555162.
Copyright
© 2022 Martins AG. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.