Outcomes of Modified Second Intention Healing for Convex Craniofacial Mohs Defects
Abstract
In patients with favorable wound healing profiles and surgical defects in well-perfused locations, second intention wound healing often leads to excellent cosmetic results after Mohs micrographic surgery. Second intention healing can be modified and accelerated with the use of acellular wound matrices, serving as a foundation to facilitate re-epithelialization and formation of granulation tissue. We present two patient cases demonstrating successful wound resolution of large, craniofacial surgical defects using second intention healing aided by acellular wound matrices.
Keywords
Second intention healing, Wound repair, Mohs micrographic surgery
Introduction
Second intention healing occurs when a surgical defect is allowed to heal by natural granulation and re-epithelialization rather than closed by a planned reconstructive technique. The decision to allow a wound to heal by secondary intention requires both the physician and the patient to consider multiple factors. As granulation tissue forms and an open wound contracts, second intention healing promotes cost-effective wound management that leads to superlative cosmetic results in carefully selected cases. Patients with high activity levels who are motivated to conduct diligent postoperative wound care or wish to avoid any further procedures are more amenable to second intention healing [1]. One of the strongest predictors of positive cosmetic outcomes subsequent to second intention healing is the location of the wound.
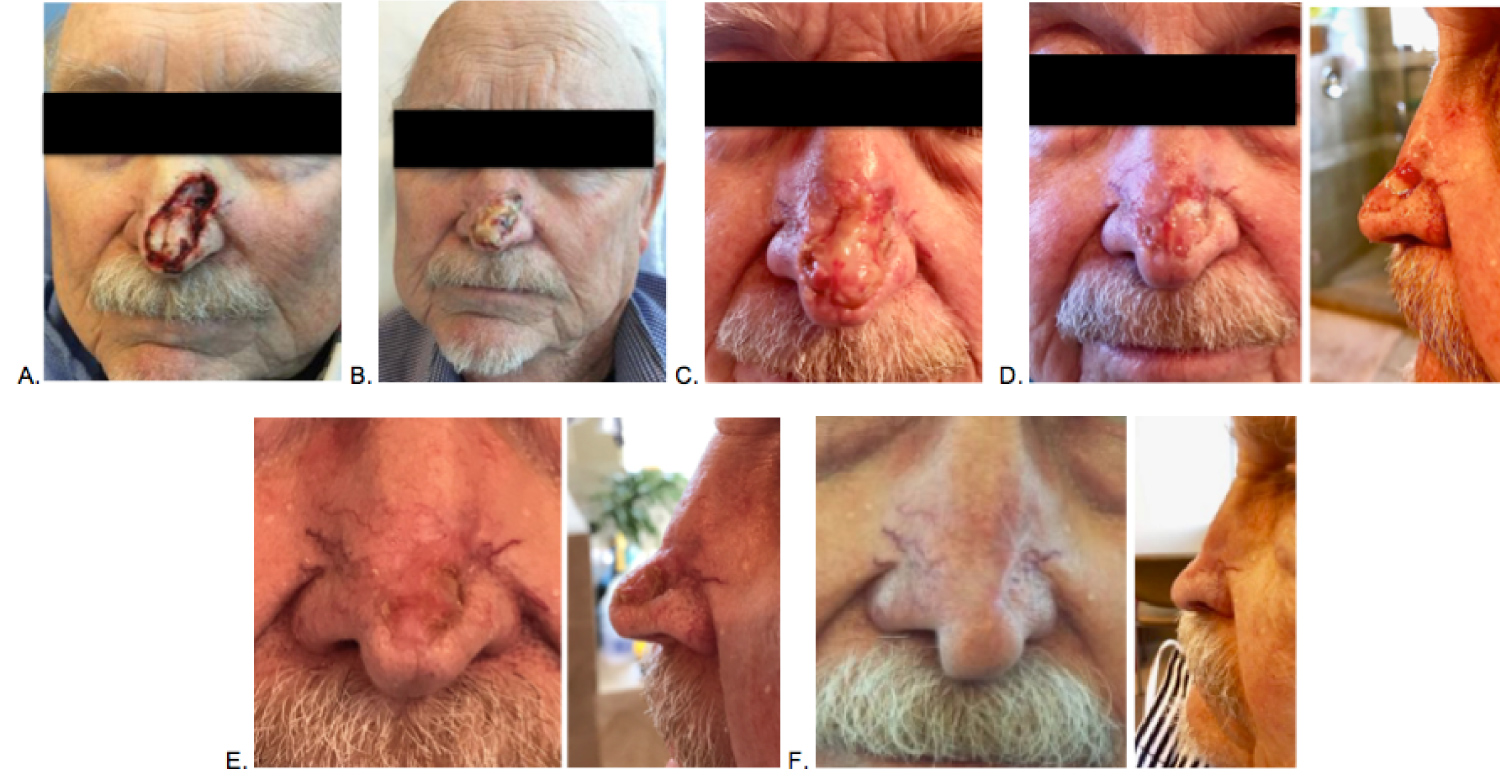
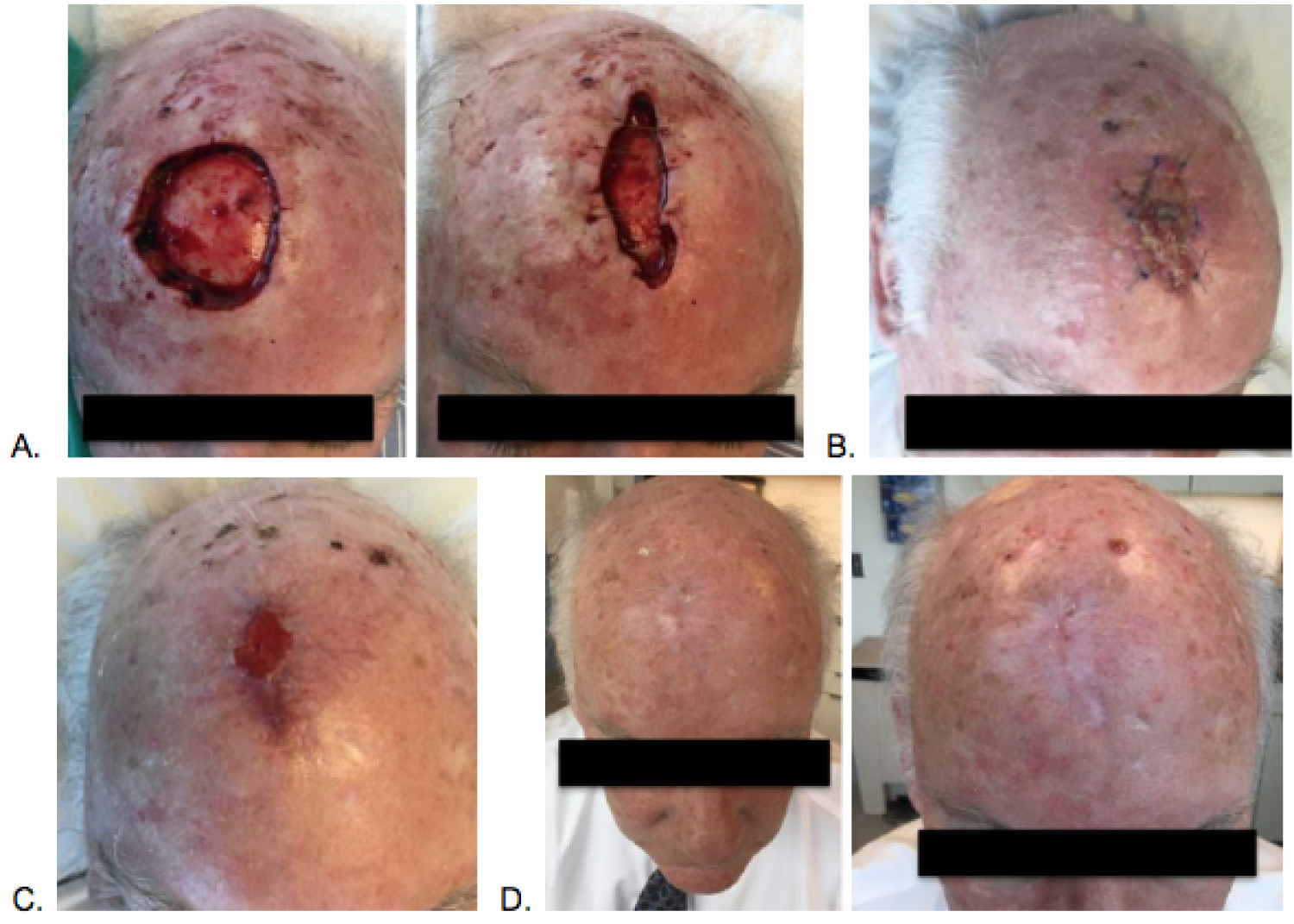
Generally, best results are seen in concave areas of the face, including the nasal alar creases and medial canthal regions, while wounds on convex facial surfaces heal with variable results, often with more prominent scar formation [2]. The following patient cases illustrate successful wound resolution by second intention following Mohs micrographic surgery in convex locations on the nose (Figure 1) and scalp (Figure 2).
Case Report
Case 1
79-year-old male with a previous history of multiple non-melanoma skin cancers presented for removal of infiltrative basal cell carcinoma located on the left nasal tip. The preoperative lesion measured 1.0 × 0.8 cm. The entire cancerous portion was removed in six stages of Mohs surgery, and the resulting surgical defect measured 3.9 × 1.9 cm. The defect was partially closed with guiding sutures after placement of acellular porcine bladder matrix (Figure 1).
Case 2
65-year-old male with a previous history of multiple non-melanoma skin cancers presented for removal of basal cell carcinoma located on the anterior scalp. The initial lesion measured 2.0 × 2.6 cm. All cancerous tissue was removed after four stages of Mohs surgery, and the resulting defect measured 4.5 × 4.7 cm. After the acellular porcine bladder matrix was adhered, the wound was partially closed with guiding sutures (Figure 2).
Discussion
When chosen in the appropriate clinical context, second intention wound healing can lead to excellent results and obviate the need for additional surgical reconstructive procedures. Selection of reasonable wounds begins with assessment of defect location. Second intention healing is not recommended for areas in close proximity to free anatomic margins in which the skin is discontinuous from surrounding structures, such as the lips or eyelids. As open wounds contract, these areas are prone to distortion due to uneven distribution of tensile strength [1]. In order for wound contraction to take place, the skin surrounding the surgical defect must offer sufficient laxity. Skin in elderly patients is associated with decreased elasticity and more pronounced wrinkling, allowing for significant contraction [3]. However, the skin in convex areas of the face is characterized by increased tension and decreased mobility, which is less likely to accommodate for acceptable contraction [4]. Anatomic distortion can often be minimized in larger defects by using guiding sutures [1-3].
While the nasal tip and scalp are not traditionally optimal locations for second intention wound healing, certain patient characteristics facilitate successful wound resolution by second intention. The patients were agreeable and healthy candidates to attempt healing by granulation. After numerous Mohs procedures, the patients previously demonstrated satisfactory healing without complications after primary surgical closures. Both patients had favorable wound healing profiles as immunocompetent, non-diabetic, non-smokers at a healthy BMI. By contrast, wound healing is commonly impaired in patients with compromised immunity, chronic disease, obesity, or an extensive smoking history [1].
Successful second intention healing depends on adequate blood circulation to the defect, which in turn allows for faster granulation tissue formation and re-epithelialization. For surgical defects that expose cartilage or bone, granulation tissue forms more efficiently over intact perichondrium or periosteum. If the periosteum is removed, creating pores in the surface of exposed bone can uncover bleeding vessels to stimulate the development of an overlying extracellular matrix, serving as scaffolding over which granulation tissue may develop and second intention healing can proceed [2-5]. Any crust or fibrous tissue that deposits over the wound surface during the healing process should be removed to prevent restriction of granulation tissue growth. Alternatively, use of skin substitutes can promote revascularization within the wound bed, stimulating rapid formation of granulation tissue in response to the enhanced blood supply [6]. Acellular porcine bladder matrix was placed in the surgical defects to simulate the architecture of an intact extracellular matrix. The skin substitute provides structural support to guide fibroblast migration to the site of injury, resulting in deposition of collagen, elastin, and other proteins that fortify the wound and establish the initial stages of granulation tissue. In the later phases of the healing process, fibroblasts differentiate into myofibroblasts, which contract to reduce the size of an open wound [7,8].
The interpretation of cosmetic results is subjective, and satisfaction with the final results varies greatly between each individual patient. Therefore, in addition to selection of wounds as candidates for second intention healing based on objective characteristics, patient preference is paramount - after discussion of all viable repair options to determine the ideal reconstructive technique.
Acellular porcine bladder matrix ACell wound matrix = Acell®
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- Lam TK, Lowe C, Johnson R, et al. (2015) Secondary intention healing and purse-string closures. Dermatol Surg 41: S178-S186.
- Zitelli JA (1983) Wound healing by secondary intention: A cosmetic appraisal. J Am Acad Dermatol 9: 407-415.
- Zitelli JA (1984) Secondary intention healing: An alternative to surgical repair. Clin Dermatol 2: 92-106.
- Becker GD, Adams LA, Levin BC, et al. (1999) Secondary Intention Healing of Exposed Scalp and Forehead Bone after Mohs Surgery. Otolaryngol Head Neck 121: 751-754.
- Odland PB, Murakami CS (1993) Healing by secondary intention. Operative Techniques in Otolaryngol Head Neck 4: 54-60.
- Greaves NS, Morris J, Benatar B, et al. (2015) Acute cutaneous wounds treated with human decellularised dermis show enhanced angiogenesis during healing. PLoS One 10: e0113209.
- Moreno-Arias GA, Izento-Menezes CM, Carrasco MA, et al. (2000) Second intention healing after Mohs micrographic surgery. JEur Acad Dermatol 14: 159-165.
- Tracy LE, Minasian RA, Caterson E, et al. (2016) Extracellular Matrix and Dermal Fibroblast Function in the Healing Wound. Adv Wound Care 5: 119-136.
Corresponding Author
Rachel Graubard, Department of Dermatology, Baylor College of Medicine, 1977 Butler Blvd, Houston, TX 77030, USA, Tel: 713-798-6131, Fax: 713-798-3252.
Copyright
© 2020 Graubard R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.