Under Pressure: Optimizing Intralesional Keloid Injections
Abstract
Background
Intralesional corticosteroid injections play an important role in the management of keloids, as a trusted and safe method of treatment.
Aims
To improve patient comfort and provider ergonomics by optimizing the methods for intralesional keloid injections.
Methods
Through assessment of the literature and experience with thousands of patients in an urban community, the following recommendations have been developed.
Results and Conclusions
The use of a 1 ml syringe as well as adjunctive measures such as larger needle gauge, cryotherapy and pulsed dye laser therapy are effective methods of optimizing intralesional corticosteroid injections for both the patient and providing physician.
Keywords
Cosmetic dermatology, Keloid, Injection, Corticosteroid, Optimizing
Discussion
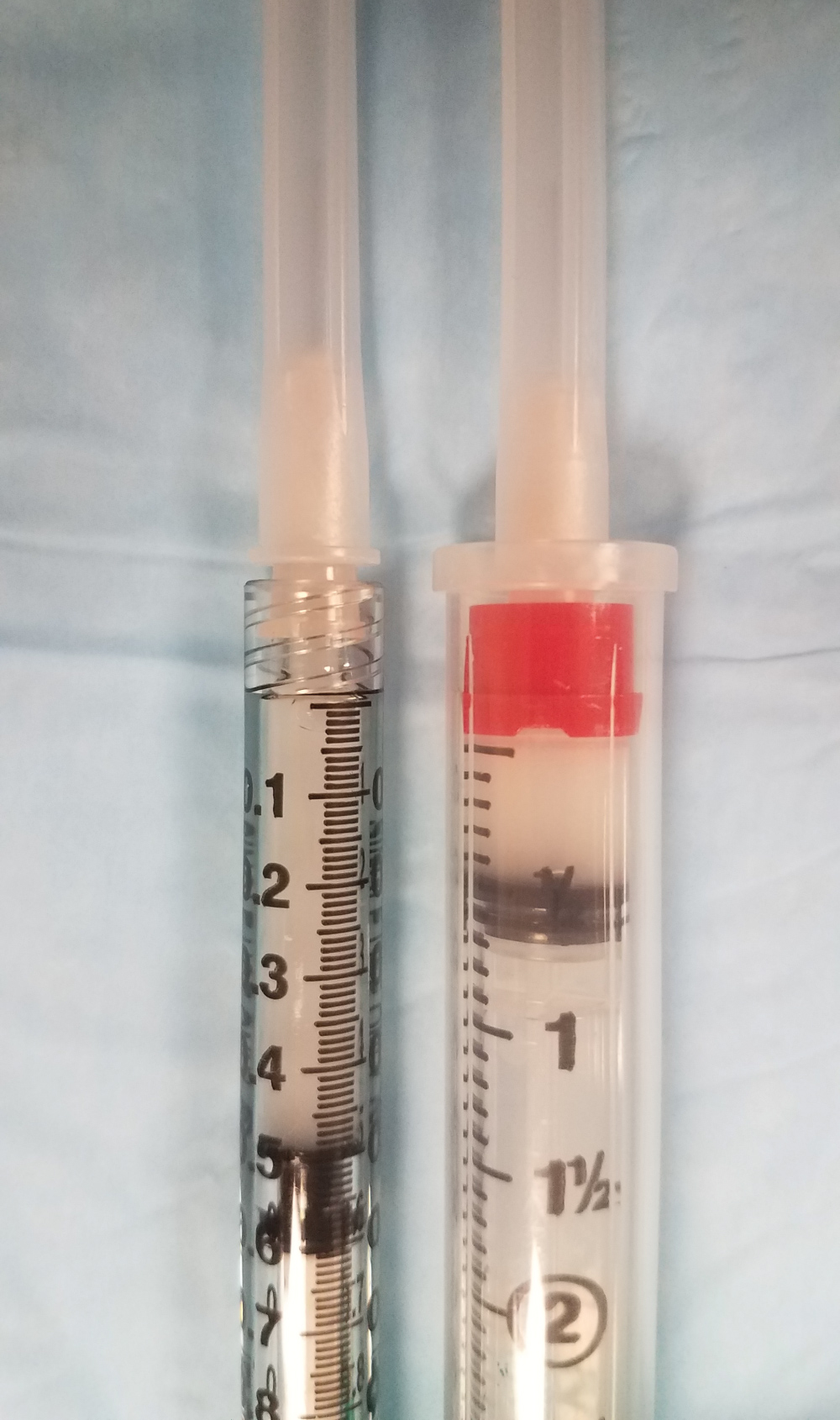
Keloids are benign fibroblastic tumors of the skin, due to aberrant tissue remodeling in predisposed individuals [1]. Although the pathogenesis is unknown, keloids are a common concern in dermatology. While numerous treatment options exist, the use of intralesional corticosteroids has endured the test of time as an effective and safe modality for management [1]. Intralesional corticosteroid injections play an important role in the management of keloids as this method is highly regarded as safe and effective, and used frequently in combination with up and coming new keloid treatment approaches. However, injecting dense tissue can cause difficulties for the provider, as well as additional pain for the patient. Consideration of syringe size can improve efficacy and overall ergonomics when injecting high-pressure tissues. Smaller syringes, due to reduced diameter, create higher injection pressures with the same manual force, increasing hydrodissection and tissue penetration. The maximum pressure created in a 1 milliliter (ml) syringe was double that of a 3 ml syringe, 363 +/- 197 pounds per square inch (psi) compared to 177 +/- 96 psi, respectively [2]. Additionally, outcomes with smaller syringes when injecting dense tissues were superior, indicating more accurate medication placement [2]. A smaller volume syringe also allows for improved visualization of fluid volumes, contributing to precision and successful aliquot placement (Figure 1). After experience with several thousand keloid injections throughout the past 10 years at an urban academic institution, in Detroit Michigan, the authors recommend a 1 ml syringe for optimum control, efficacy, and efficiency when managing keloids with intralesional corticosteroids. When using 30-gauge needles, cryotherapy or laser therapy are effective adjuncts to assist with intralesional injections [1]. Cryotherapy treatment involves the use of liquid nitrogen applied directly to the keloid for 15-30 second intervals at varying time points along with intralesional corticosteroid injections [3,4] Pulsed dye laser therapy (585-595 nm) has also been used along with intralesional corticosteroids, generally with a defined number of fixed pulses every 2-3 months. One particular study used the following settings: 4-15 J/cm2, 7 mm spot, 1.5 msec duration or pulse, 595 nm wavelength, DCD, 30 msec spray with 20 msec delay, carried out every 6-8 weeks [5]. Additionally, there are countless emerging approaches for the treatment of keloids, including CO2 laser, 5-fluorouracil treatment, and many more [4]. However, intralesional corticosteroids remains a strong combination measure in the treatment of keloids in nearly all of the new treatment modalities, and the methods used for the well-known approach of intralesional therapy should be considered.
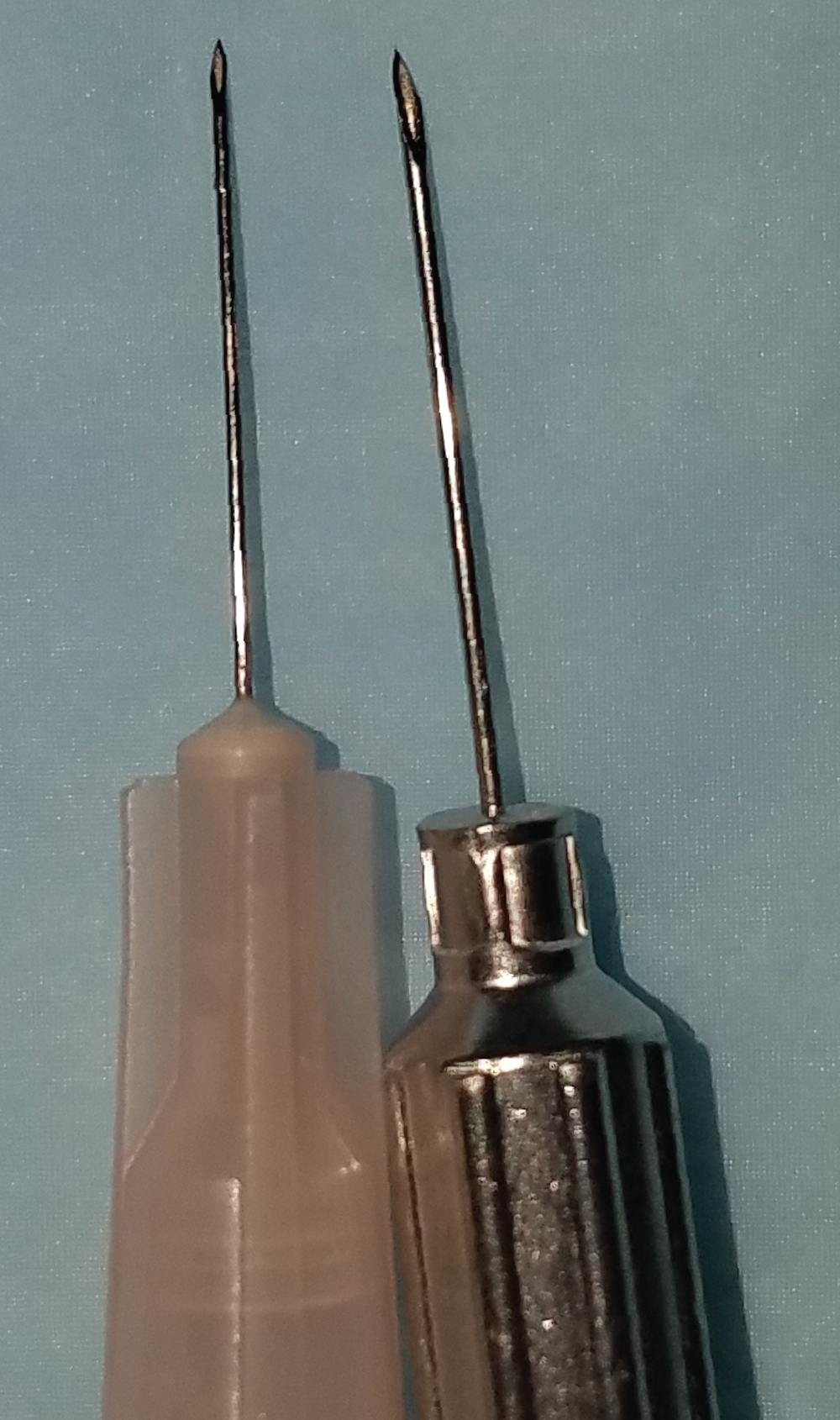
This article demonstrates that intralesional corticosteroids are widely accepted in dermatology as an effective and safe treatment modality for keloids, and provide two simple recommendations to further improve this very common practice. We recommend the use of a 1 ml syringe to assist with injecting dense tissue, as discussed above. In addition, we also recommend the use of larger needles, such as 26-gauge or greater gauge size, to help optimize corticosteroid delivery when injecting into very dense tissues (Figure 2).
Funding Sources
None.
IRB Approval Status
N/A.
Conflicts of Interest
None declared.
References
- Arno AI, Gauglitz GG, Barret JP, et al. (2014) Up-to-date approach to manage keloids and hypertrophic scars: A useful guide. Burns 40: 1255-1266.
- Hayward WA, Haseler LJ, Kettwich LG, et al. (2011) Pressure generated by syringes: Implications for hydrodissection and injection of dense connective tissue lesions. Scand J Rheumatol 40: 379-382.
- Boutli-Kasapidou F, Tsakiri A, Anagnostou E, et al. (2005) Hypertrophic and keloidal scars: An approach to polytherapy. Int J Dermatol 44: 324-327.
- Behera B, Kumari R, Thappa DM, et al. (2016) Therapeutic Efficacy of Intralesional Steroid With Carbon Dioxide Laser Versus With Cryotherapy in Treatment of Keloids: A Randomized Controlled Trial. Dermatol Surg 42: 1188-1198.
- Stephanides S, Rai S, August P, et al. (2011) Treatment of refractory keloids with pulsed dye laser alone and with rotational pulsed dye laser and intralesional corticosteroids: A retrospective case series. Laser Ther 20: 279-286.
Corresponding Author
David M Ozog, Department of Dermatology, Henry Ford Hospital, 3031 West Grand Boulevard, Suite 800, Detroit, MI 48202, USA, Tel: 313-916-2111, Fax: 313-916-5335.
Copyright
© 2019 Smith MK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.