Effect of Obesity and Overweight on Lung Function and Six-Minute Walking Test in Patients with COPD
Abstract
Chronic obstructive pulmonary disease (COPD) is responsible for impaired quality of life and a limitation of daily activity. Some studies have concluded that obese subjects have better respiratory function and thus a better quality of life. The aim of our work was to determine the impact of obesity and overweight on functional parameters, six-minute walking test (6MWT) performance, and severity and prognosis of COPD in this population.
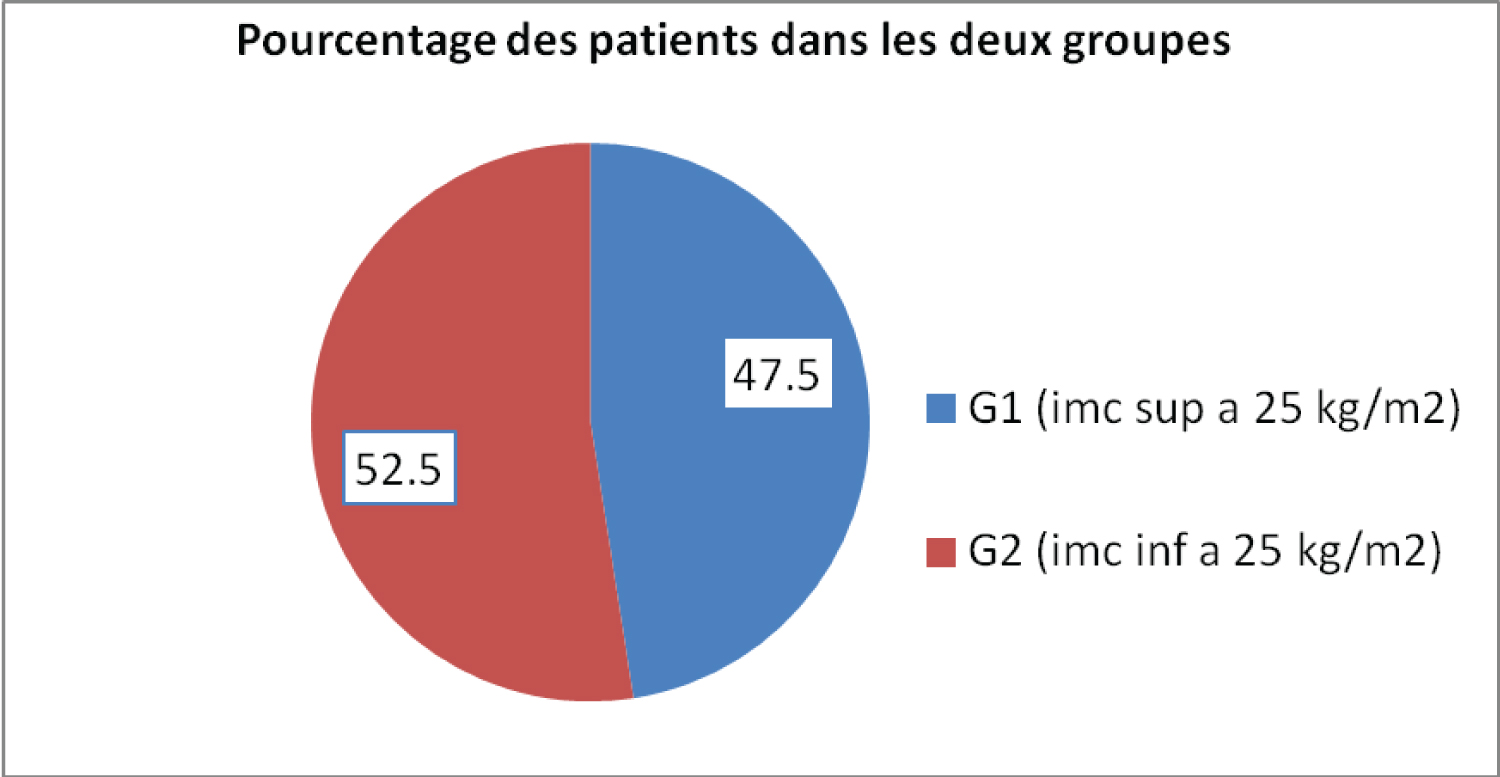
Methods: Sixty-one consecutive stable COPD patients were included after obtaining written informed consent. Demographic and clinical data, spirometric values, 6-minute walking distance, BMI and fat mass were collected for analysis.
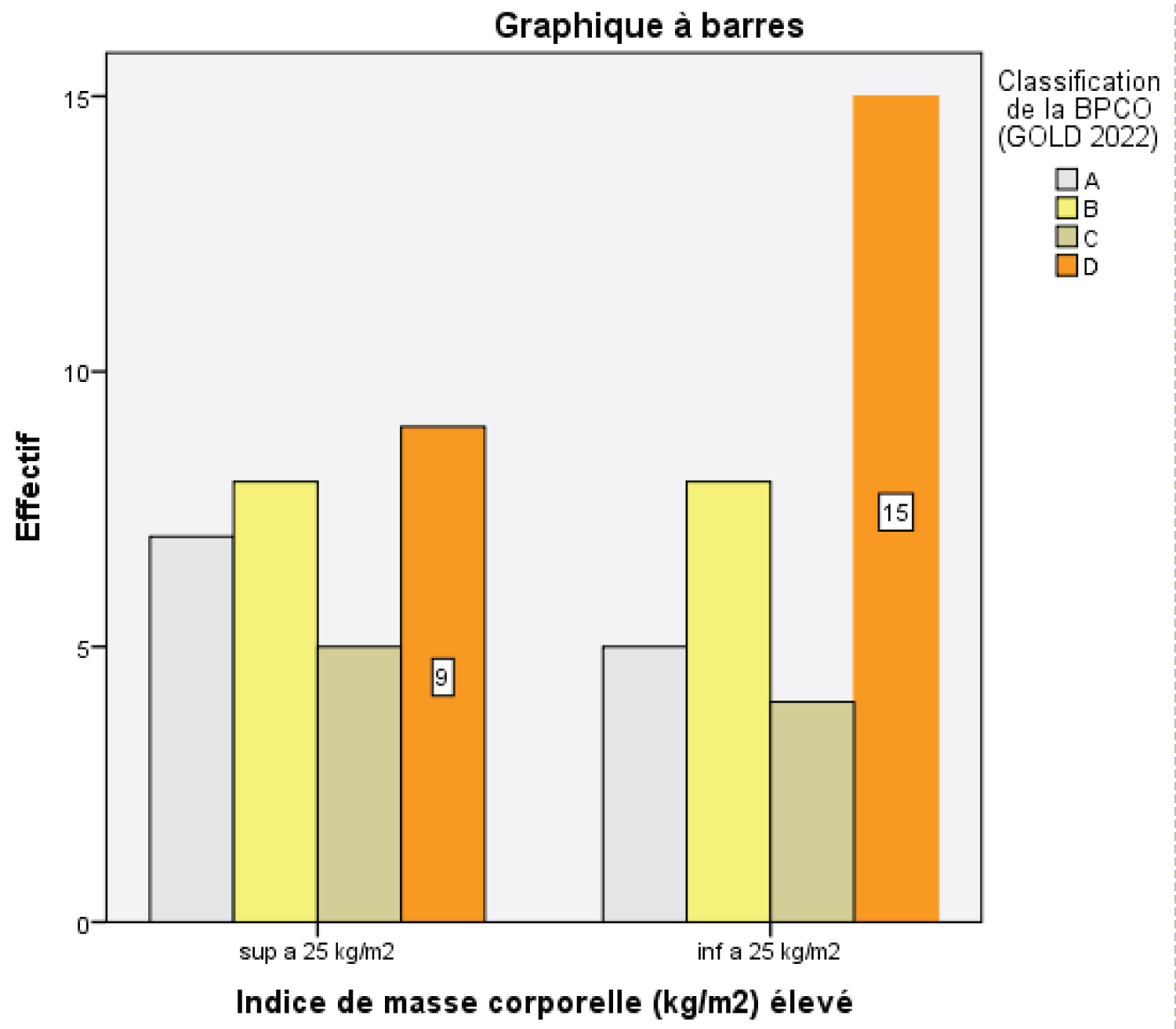
Two groups were compared: G1 group of patients with BMI >= 25 kg/m 2 ; G2 group of patients with BMI < 25 kg/m 2 . The statistical study was carried out using SPSS 20.0 software.
Results: An average BMI of 24.12 4.83 kg/m 2 , with extreme values ranging from 14.60 to 36.90 kg/m 2 .
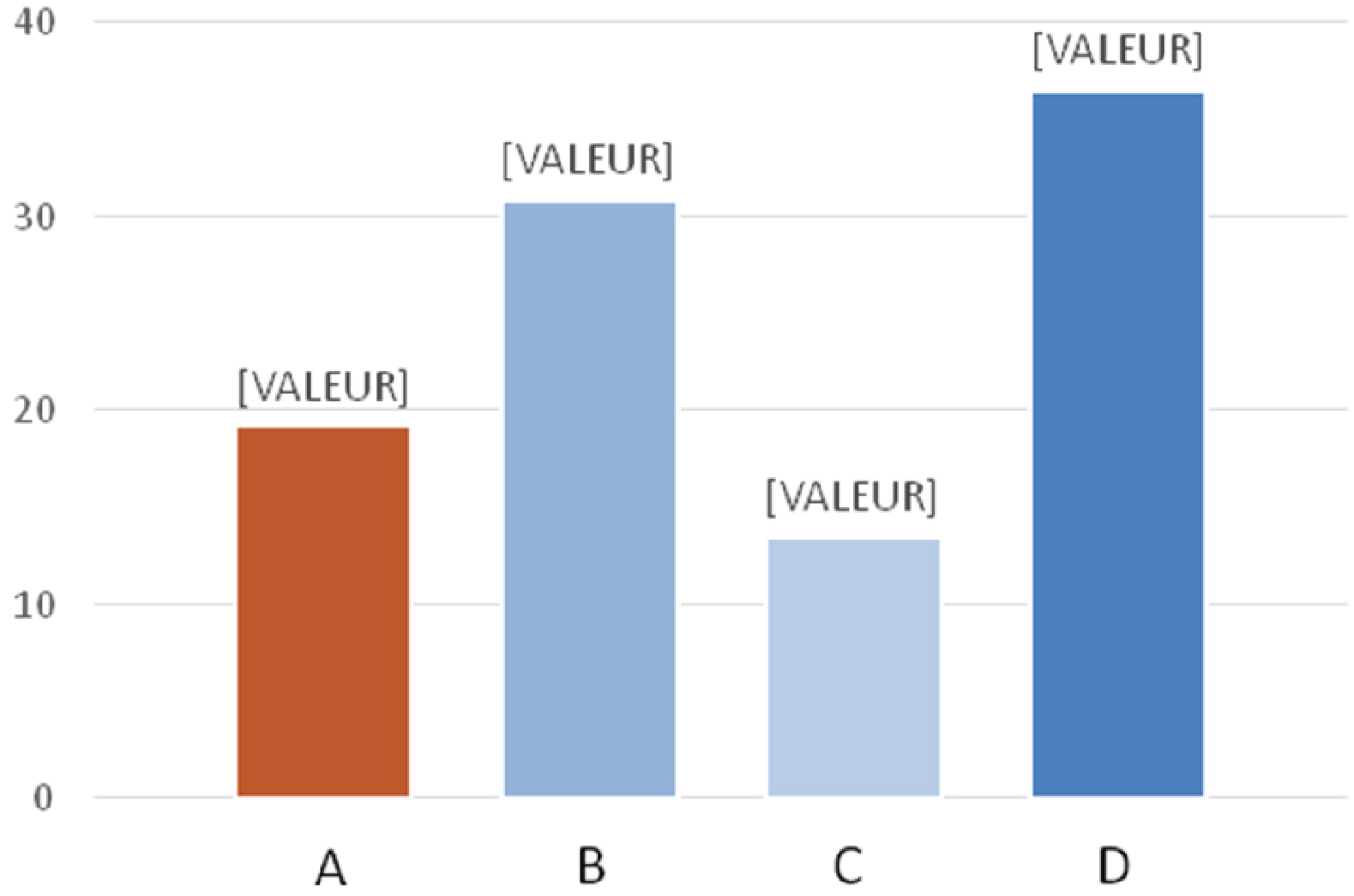
Distribution of COPD patients according to the OMS classification of obesity:
Lean: < 18.5 kg/m 2 (13.1%)
Normal: [18.5-25 kg/m 2 ] (39.3%)
Overweight: [25-30 kg/m 2 ] (36.1%)
Obesity: [30-40 kg/m 2 ] (11.5%)
Obese COPD do not have lung distension, unlike non-obese COPD.
In patients with COPD, obesity was associated with less severe airway obstruction.
The data from our work are consistent with those of the literature showing that overweight and obesity in patients followed for COPD are associated with better tolerance to exercise.
Conclusions: Contrary to expectations, obesity is not necessarily associated with adverse effects during COPD. As our results show, The data from our work are consistent with those of the literature showing that overweight and obesity in patients followed for COPD are associated with better tolerance to effort and has less severe airway obstruction.
Introduction
GOLD 2023 defines COPD as a heterogeneous lung condition characterized by chronic respiratory symptoms (dyspnea, cough, expectoration and/or exacerbations) due to airway abnormalities (bronchitis, bronchiolitis) and/or alveoli (emphysema) that cause persistent, often progressive, airflow obstruction, COPD is a major public health problem and is a leading cause of chronic morbidity and mortality worldwide.
Prevalence of COPD is difficult to assess because it requires patient cohorts representative of the entire population using spirometric measurements [1].
Studies have shown a wide geographic disparity in COPD prevalence [2]. This is due to differences in survey methods, diagnostic criteria and target populations. An estimated 384 million people had COPD in 2010 and the global prevalence is estimated at 11.7% (8.4%-15.0%) in 2015 [3].
According to the BOLD study: 10.1% of people over 40 have COPD [4].
Global Burden of Diseases (GBD) data, compiled by the World Health Organization (WHO), shows that 175 million people have chronic obstructive pulmonary disease (COPD), which represents 2.48% of the world’s population, including 70 million women. COPD was responsible for 3.2 million deaths in 2015, representing 5.71% of all deaths [5].
In Algeria, according to the results of the Breathe study, COPD prevalence is estimated at 4% in the general population and 25% among smokers [6].
COPD and obesity are two diseases whose prevalence has been increasing in recent years. Obesity is also a disease that affects the ventilatory function [7]. The literature generally suggests a prevalence of obesity in COPD ranging from 23% to 43%. This prevalence varies from country to country, and data on the impact of COPD on the disease (COPD) is still very limited.
• According to O. Bouroubi, et al. [8], the prevalence of obesity in COPD at the Constantine wilaya in 2019 was 7.4% for obesity and 31.9% for overweight (WHO definition)
• The proportion of overweight people has increased considerably in the early twentieth century in the world.
• In 2016, there were 1.9 billion overweight people (BMI over 25) and approximately 600 million overweight (BMI over 30).
The pathophysiology of increased obesity in COPD is unclear, it is possible that poor lung function increases the risk of obesity. This may be due to the following three causes:
1) Breathing difficulties in exercise-related COPD patients often result in lower levels of physical activity and therefore fewer calories burned during exercise.
2) One common side effect of long-term glucocorticosteroid drugs is weight gain [9].
3) Due to their hypoxaemia at rest and exercise, COPD patients are unable to use oxygen for beta-oxidation fatty acid degradation.
• Several studies support the hypothesis that obesity exposes individuals to a greater risk of COPD [10].
Target population
Patients with confirmed COPD with a FEV1/FVC ratio < 70% after bronchodilator [11] and followed up in the Pulmonology Department of the Constantine Regional Military University Hospital (HMRUC).
Sixty-one consecutive stable COPD patients were included after obtaining written informed consent. Demographic and clinical data, spirometric values, 6-minute walking distance, BMI and fat mass were collected for analysis.
Two groups were compared: G1 group of patients with BMI >= 25 kg/m 2 ; G2 group of patients with BMI < 25 kg/m 2 . The statistical study was carried out using SPSS 20.0 software.
Objective of the Study
The aim of our work was to determine the impact of obesity and overweight [based on body mass index (BMI) and fat percentage (% FM) on:
• The six-minute walking test (TM6) performance of patients followed for COPD.
• Lung function.
• The severity and prognosis of COPD in this population.
This is a prospective descriptive observational study conducted in the HMRUC’s pulmonology department, 61 patients participated in the study.Inclusion criteria:
All patients with COPD, aged over 40-years-old, in a stable state.
• Criteria for non-inclusion:
∘ Restrictive respiratory pathology.
∘ Progressive cardiovascular disease.
∘ Recent surgery (less than 3 months)
The Results
• Obese COPD do not have lung distension, unlike non-obese COPD
• In patients with COPD, obesity was associated with less severe airway obstruction
• The data from our work are consistent with those of the literature showing that overweight and obesity in patients followed for COPD are associated with better tolerance to exercise (Table 1, Table 2, Table 3, Table 4, Table 5, Table 6, Table 7, Figure 1, Figure 2, Figure 3, Figure 4, Figure 5 and Figure 6).
Discussion
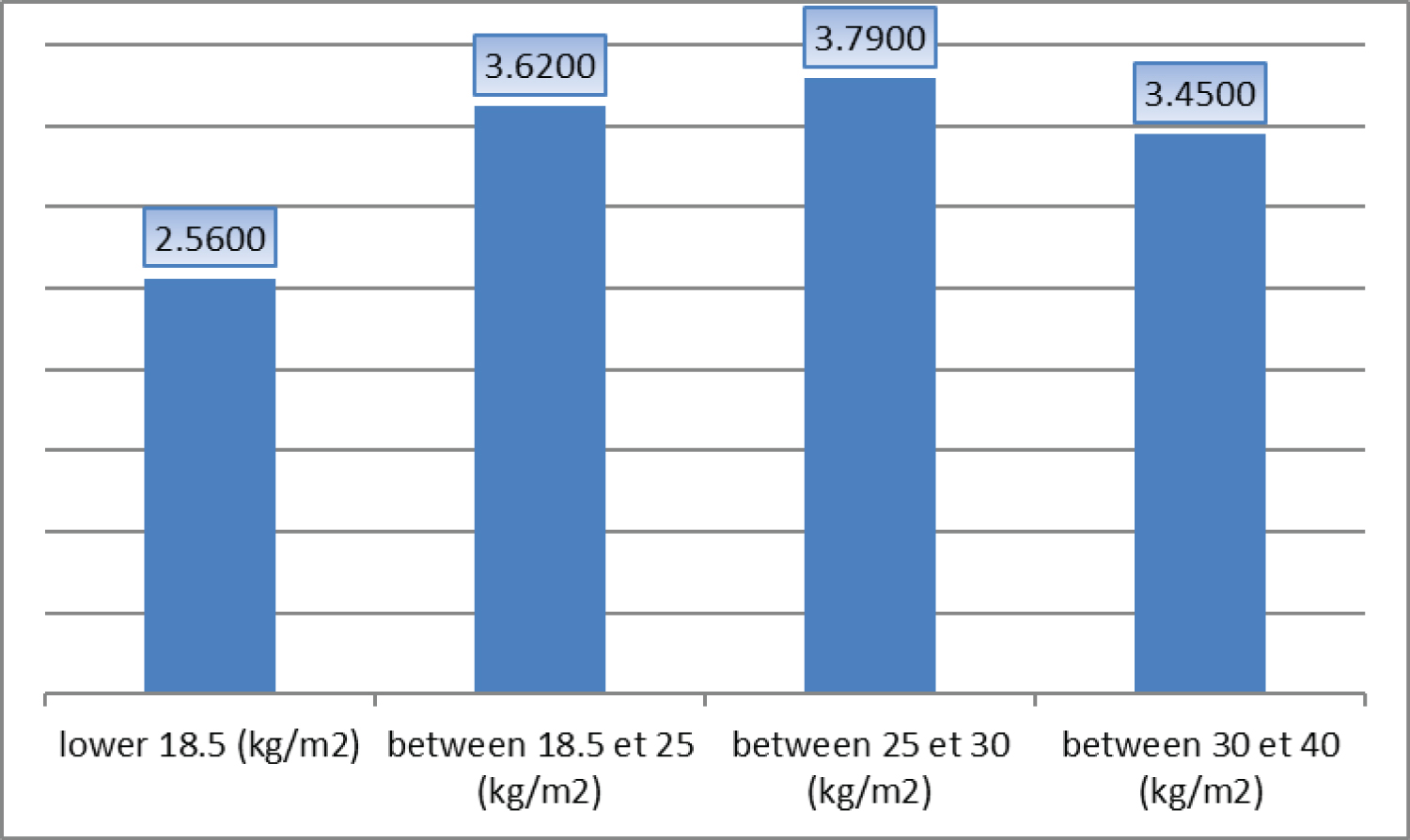
The results obtained in our study show an average BMI of 24.12 4.83 kg/m 2 , with extreme values ranging from 14.60 to 36.90 kg/m 2 . This average is comparable to that observed in the Tunisian cohort studied by Snène [12], where the average BMI was 23.41 4.8 kg/m 2 . Other international studies reported similar or divergent results. For example, El Gazzar AG, et al. [13] in Egypt found an average BMI of 25.32 2.57 kg/m 2 , while Yamada T, et al. [14] in Japan reported a slightly lower average of 22.5 2.9 kg/m 2 . In India, Ramachandran P, et al. [15] reported an average BMI of 20.6 3.5 kg/m 2 , and finally, in Turkey, Topcuoglu C, et al. [16] reported a BMI of 27.05 4.07 kg/m 2 .
These significant variations in BMI between studies, conducted in countries with different socio-economic and cultural contexts, illustrate the impact of these factors on weight status. Living standards, eating habits, access to sports facilities, health awareness and participation in physical activities can directly or indirectly influence the BMI of the populations studied.
According to the meta-analysis by Seifir, et al. [17], body mass index (BMI) of patients with COPD varies from 21.8to 31.8 kg/m 2 depending on the population studied. This study also found that the ideal weight class (BMI between 18.5 and 25 kg/m 2 ) is predominant in most cohorts, which is consistent with our results.
In our series, a negative correlation was observed between BMI and the presence of emphysema. Patients with emphysema generally had lower BMI, as shown by our statistical analysis (Student’s test: t = -3.112, p = 0.003). This relationship was also reported by Papaioannou, et al. [18] who showed that pulmonary emphysema is associated with a decrease in BMI and lean mass. This relationship can be explained by the direct or indirect effect of systemic inflammation.
Some studies, such as those by Katz P, [19] and Ben Sassi S [20], suggest that significant weight gain may lead to increased co-morbidities, which reinforces our findings. We observed a significant correlation between the average number of comorbidities and the different stages of the OMS classification for obesity, with a p-value of 0.039.
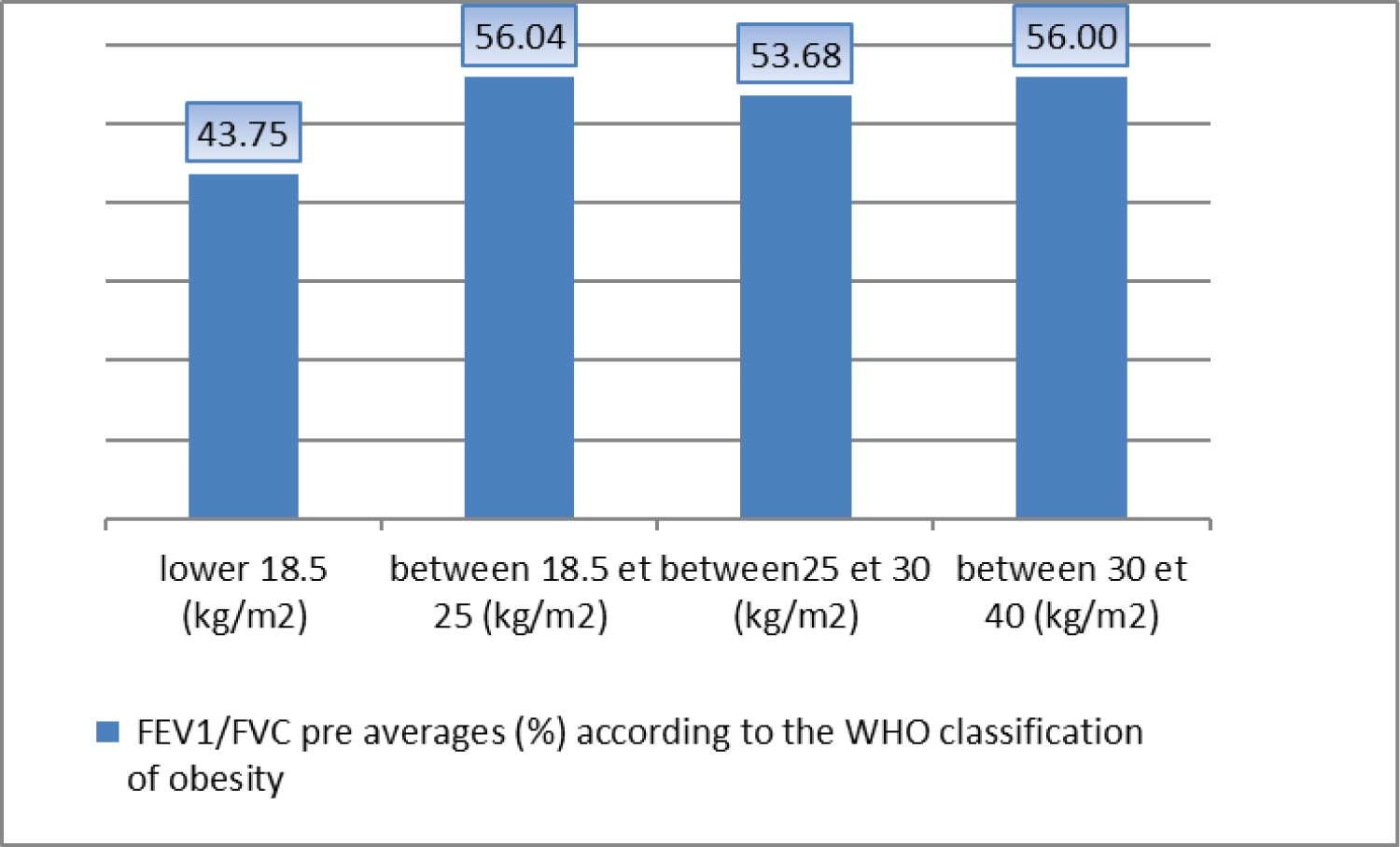
In our study, the mean BMI was higher in patients with less symptoms (groups A and C) (p = 0.014), a result that is consistent with the study by Radovanovic D, et al. [21]. It should be noted that for some authors, obesity is not necessarily associated with adverse effects in COPD. A Tunisian study, involving 95 patients [20] showed that obesity in COPD patients was linked to less severe airway obstruction.
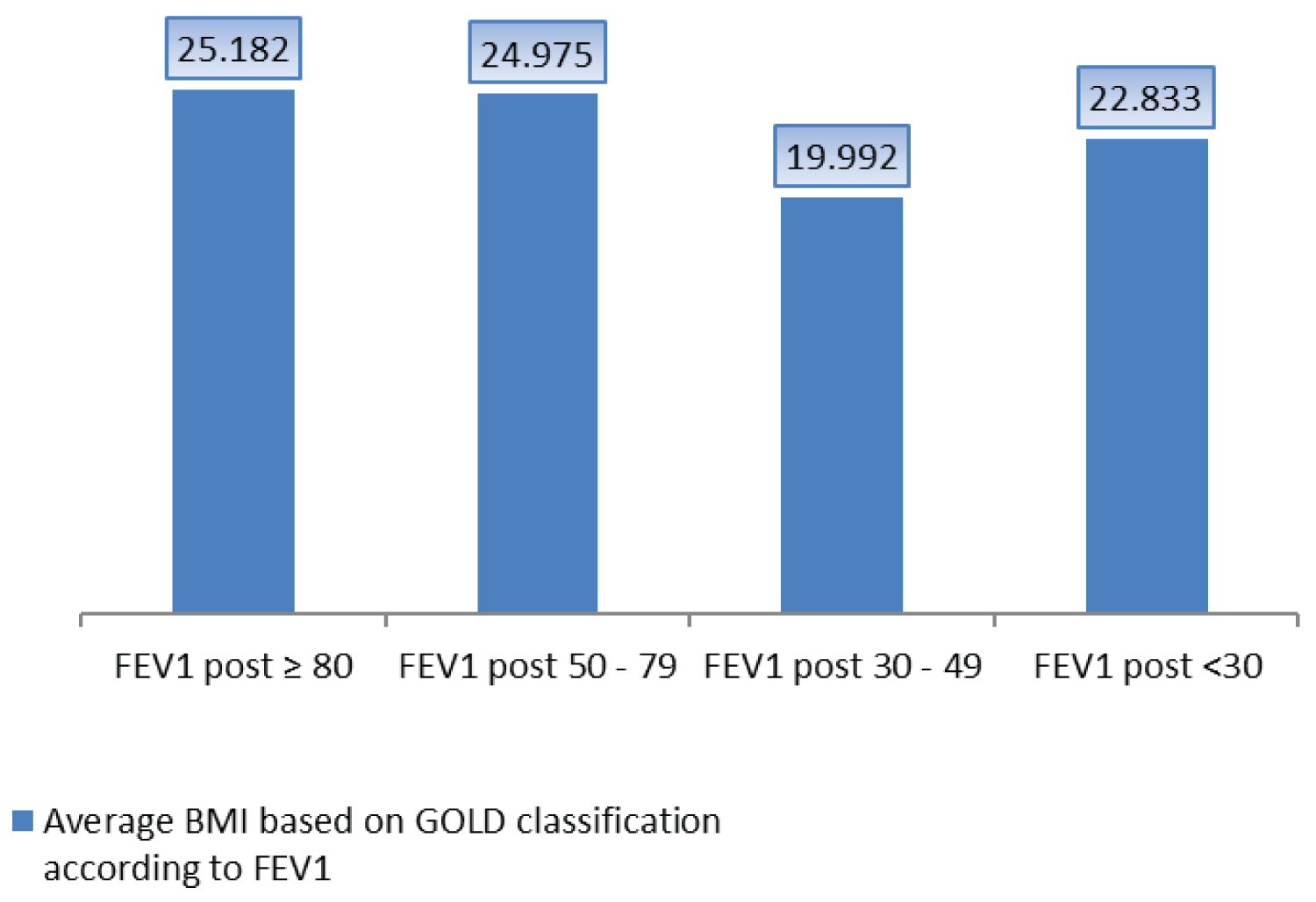
Our study also showed that the mean values of BMI, expressed in kg/m 2 , varied, according to the severity of COPD assessed by the FEV1. Patients with mild COPD had a mean BMI of 25.13 3.30, those with moderate COPD of 24.97 5.39, those with severe COPD of 19.99 4.09, and finally those with very severe COPD of 22.83 4.40. These results are in agreement with those of Chailleux E, et al. [22] and Talamo C, et al. [23], who also found a positive correlation between the severity of COPD and a lower BMI. However, they disagree with the findings of Vermeeren M, et al. [24] who reported that 73% of COPD patients had normal BMI and lean mass index. Likewise, Similarly, El-hay A, [25] did not find statistically significant differences (p > 0.05) between the different stages of COPD in terms of BMI, with mean values of 27.91 3.52 for mild COPD, 26.99 5.96 for moderate COPD, 25.09 5.13 for severe COPD, and 25.41 3.90 for very severe COPD. The control group BMI in this study was 27.50 3.82 kg/m 2 .
Our study also found a significant correlation between BMI and distance travelled in the six-minute walking test (MV6), with a correlation coefficient r = 0.318 (p = 0.013). Guenette, et al. [26] observed that obese patients with COPD were not disadvantaged compared to patients who were slimmer when exercising.
In addition, a study by Ora, et al. [27] found that obese patients with COPD have higher intra-abdominal pressure, similar operational lung volumes and ventilatory efficiency comparable to that of lean patients during physical exertion.
Finally, our study found a significant negative correlation between body mass index (BMI) and dyspnea measured using the MMRC scale (r = -0.269, p = 0.036), indicating that higher BMIs are associated with less pronounced dyspnea.
However, the results of the ECLIPSE study [28] seem to contradict these observations. Indeed, this study indicates that obese patients with chronic obstructive pulmonary disease (COPD) have more severe dyspnea and overall quality of life impaired than those with normal weight. This divergence highlights the need to further explore underlying mechanisms and potential confounding factors in the relationship between obesity and dyspnea in patients with COPD.
Conclusions
Contrary to expectations, obesity is not necessarily associated with adverse effects during COPD. As our results show, The data from our work are consistent with those of the literature showing that overweight and obesity in patients followed for COPD are associated with better tolerance to effort and has less severe airway obstruction.
During COPD, weight loss is a factor in poor prognosis. Overweight or obesity, a common situation in these patients, could be a protective factor.
More research is needed to better understand the underlying mechanisms of this complex interaction between obesity and COPD.
Statement
- There is no conflict of interest among co-authors.
- The authors confirm that an institutional or independent ethics committee has approved the study and informed consent was obtained from the donor.
- Consent to publication acquired.
- Availability of supporting data.
- Authors Contribution: A. Meridj: Designed and developed the analysis; Written the article; R. Belala: Collected data; K. Tlili: Contributed to data or analytics tools; Y. Djeghri: Conducted the analysis.
- Thanks: I thank Pr Y. Djeghri for all the efforts made to complete this work.
References
- Chabot F, Zysman M, Guillaumot A, et al. (2019) La bronchopneumopathie chronique obstructive. Bulletin de l'Académie Nationale de Médecine 203: 63-71.
- Raherison C, Girodet P (2009) Epidemiology of COPD. Eur Respir Rev 18: 213-221.
- Adeloye D, Chua S, Lee C, et al. (2015) Global and regional estimates of COPD prevalence: Systematic review and meta-analysis. J Glob Health 5: 020415.
- Buist A, Vollmer W, McBurnie M (2008) Worldwide burden of COPD in high-and low-income countries. Part I. The Burden of Obstructive Lung Disease (BOLD) Initiative. Int J Tuberc Lung Dis 12: 703-708.
- WHO (2016) Global health estimates (GHE). WHO: Geneva, Switzerland.
- Uzaslan E, Mahboub B, Beji M, et al. (2012) The burden of chronic obstructive pulmonary disease in the Middle East and North Africa: Results of the BREATHE study. Respir Med 106: S45-S59.
- Pelosi P, Croci M, Ravagnan I, et al. (1998) The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg 87: 654-660.
- Bouroubi O, Khelifi S, Belkadi L, et al. (2019) Profil inflammatoire du BPCO obèse algérien. Revue des Maladies Respiratoires 36: A100.
- Franssen F, O'Donnell S, Goossens G, et al. (2008) Obésité et poumon: obésité et BPCO. Thorax 63: 1110-1117.
- Behrens G, Matthews CE, Moore SX, et al. (2014) Taille corporelle et activité physique en relation avec l'incidence de la maladie pulmonaire obstructive chronique. CMAJ 186: E457-E469.
- Agustí A, Celli BR, Criner GJ, et al. (2023) Global initiative for chronic obstructive lung disease 2023 report: GOLD executive summary. Am J Respir Crit Care Med 207: 819-837.
- Snène H, Rafrafi R, Salah N, et al. (2021) Anxiety and depression in Tunisian patients with COPD. Tunis Med 99: 623-631.
- El Gazzar AG, Essawy TS, Ebaid HH, et al. (2022) Integrated use of transthoracic ultrasound and echocardiography in evaluating patients with chronic obstructive pulmonary disease. The Egyptian Journal of Hospital Medicine 88: 3668-3675.
- Yamada T, Minami T, Yoshino S, et al. (2023) Diaphragm ultrasonography: Reference values and influencing factors for thickness, thickening fraction, and excursion in the seated position. Lung 202: 1-8.
- Ramachandran P, Devaraj U, Patrick B, et al. (2020) Ultrasonographic assessment of skeletal muscle mass and diaphragm function in patients with chronic obstructive pulmonary disease: A case-control study. Lung India 37: 220-226.
- Topcuoglu C, Yümin ET, Hizal M, et al. (2022) Examination of diaphragm thickness, mobility and thickening fraction in individuals with COPD of different severity. Turkish J Med Sci 52: 1288-1298.
- Safiri S, Carson-Chahhoud K, Noori M, et al. (2022) Burden of chronic obstructive pulmonary disease and its attributable risk factors in 204 countries and territories, 1990-2019: Results from the Global Burden of Disease Study 2019. BMJ 378: e069679.
- Papaioannou AI, Mazioti A, Kiropoulos T, et al. (2010) Systemic and airway inflammation and the presence of emphysema in patients with COPD. Respir Med 104: 275-282.
- Katz P, Iribarren C, Sanchez G, et al. (2016) Obesity and functioning among individuals with chronic obstructive pulmonary disease (COPD). COPD 13: 352-359.
- Ben Sassi S, Rouis H, Moussa C, et al. (2022) Impact de l’obésité sur la sévérité de la bronchopneumopathie chronique obstructive. Revue des Maladies Respiratoires Actualités 14: 94.
- Radovanovic D, Contoli M, Marco FD, et al. (2019) Clinical and functional characteristics of COPD patients across GOLD classifications: results of a multicenter observational study. COPD 16: 215-226.
- Chailleux E, Laaban J-P, Veale D (2003) Prognostic value of nutritional depletion in patients with COPD treated by long-term oxygen therapy: Data from the ANTADIR observatory. Chest 123: 1460-1466.
- Tálamo C, de Oca MM, Halbert R, et al. (2007) Diagnostic labeling of COPD in five Latin American cities. Chest 131: 60-67.
- Vermeeren MAP, Creutzberg EC, Schols AMWJ, et al. (2006) Prevalence of nutritional depletion in a large out-patient population of patients with COPD. Respir Med 100: 1349-1355.
- El-hay A, Ibrahim AE-h, Abd Elnaby HEH, et al. (2019) Ultrasonographic assessment of diaphragmatic function and its correlation with chronic obstructive pulmonary disease severity. The Egyptian Journal of Hospital Medicine 76: 4524-4532.
- Guenette JA, Jensen D, O'Donnell DE (2010) Respiratory function and the obesity paradox. Curr Opin Clin Nutr Metab Care 13: 618-624.
- Ora J, Laveneziana P, Wadell K, et al. (2011) Effect of obesity on respiratory mechanics during rest and exercise in COPD. J Appl Physiol 111: 10-19.
- Exuzides A, Colby C, Briggs AH, et al. (2017) Statistical modeling of disease progression for chronic obstructive pulmonary disease using data from the ECLIPSE study. Med Decis Making 37: 453-468.
Corresponding Author
A. Meridj, Pulmonology Service, Constantine Regional Military University Hospital, Algeria.
Copyright
© 2024 Meridj A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.