Stay at Home Order and Psychosocial Wellbeing among Older Adults in Buenos Aires City, Argentina, during the Pandemic COVID19
Abstract
Background: This paper explores changes in the well-being of a group of people ages 65 and over in the city of Buenos Aires, Argentina during the stay at home mandated by the government in response to the COVID-19 pandemic (March to November 2020). Due to its higher level of risk, this population group was subjected to specific isolation measures.
Subjects and methods: The study objectives were 1) To identify the determinants of psychosocial well-being of people ages 65 and over, and 2) To describe the longitudinal variation in well-being in this population. Data was collected three times over a sixty-day period. A well-being scale was generated using a subset of the Clinical Interview Schedule - Revised (CIS-R) questions commonly used in the United Kingdom and validated by the World Health Organization.
Results: Statistically significant associations were found between levels of well-being and feelings of loneliness and self-reported health, gender, and exposure to mass media.
Conclusions: While the level of psychosocial well-being across the sample remained relatively constant, psychosocial well-being varied within individuals during the period under study. Self-reported health, feelings of loneliness and gender played a key role in predicting psychosocial well-being. Recommendations for public policy intervention are offered.
Keywords
COVID-19, Older adults, Psychosocial well-being, Longitudinal study, Argentina
Introduction
On March 11, 2020, the World Health Organization declared COVID-19 a pandemic. At the international level, measures were taken to restrict contagion. Different authors have referred to these measures using terms such as quarantine, lockdown or stay at home orders. Although the latter is the most appropriate to describe the Argentine situation, we will use them interchangeably. Early in the pandemic, experts warned that people experience uncertainty, frustration, fear, boredom, and confusion in situations of social isolation, as well as in epidemics and pandemics. These experiences can worsen pre-existing mental health conditions [1] and should therefore be considered when developing pandemic control policies [2]. The restriction on mobility caused a sudden and drastic change in social and individual life. Since the beginning of the pandemic in Asia and Europe, some authors pointed to the importance of mitigation policies including the key role of isolation and social distancing [3].
On March 3, the first positive coronavirus case was reported in the city of Buenos Aires, Argentina. To prevent the spread of the virus, on March 20 the national government enforced the social, preventive, and mandatory isolation (ASPO, Spanish acronym) of the population. Previously, people over 60 years of age, pregnant women and people with certain illnesses had been asked to work from home.
Argentina was one of the countries with the longest and strictest measures in the world. These included schools and workplace closures, cancellation of public events, restrictions on public and private gatherings, debt repayment suspensions, mandatory face mask wearing, stay at home orders, and restrictions on domestic and international travel among others [4].
The isolation measures initially had broad support from the population [5]. The stay-at-home order lasted eight months, and public support gradually decreased [6]. On November 8, the isolation measures ended and were replaced by mandatory social distancing measures.
Although the isolation policy was uniformly applied to the whole population, the health authorities emphasized the vulnerability of the population over 65. In the city of Buenos Aires, a measure was issued specifically aimed at people over 70 years of age that imposed on them the obligation to request an official authorization to leave the home. This measure, which was legally contested and rapidly overturned because of its discriminatory nature, was based on the greater health risks faced by the older adults whose "mortality from COVID19 can reach 80%" [7].
According to Brooks, et al. pre-COVID 19 quarantines have had negative psychological impacts that can continue after the end of the isolation [1]. Quarantine was a predictive factor of acute stress, manifested in exhaustion, strong symptoms of depression, detachment from others, anxiety, insomnia, weak concentration, and emotional instability. Those who had been in isolation due to their contact with potential infected cases experienced few feelings of happiness and predominantly expressed fear, nervousness, sadness, guilt, and confusion. Similarly, studies conducted during the COVID-19 pandemic have identified negative impacts like fear [8], increased feelings of loneliness in all age groups [9] and in older adults [10], and the deterioration of self-reported health [11,12]. Most studies focused on the general population with less attention paid to older adults.
Coincidentally, studies conducted in Argentina during the initial stages of the COVID-19 pandemic, highlighted that isolation had negative and incremental impacts on the psychosocial well-being of the population, which manifested in feelings of fear, uncertainty, anguish [13,14], and depressive and anxiety symptoms [15]. One study found that fear of contracting COVID-19 was present throughout the population, although it was less marked in people aged 70 and over compared to the younger population [16].
Much of the research published in 2020 was developed in the early stages of the pandemic and so is anchored in a specific temporal context. The study of a more advanced stage of the stay at home order opens the way to explore possible changes in psychosocial well-being over time.
Considering the consensus among researchers that quarantine is associated with negative impacts on psychosocial well-being, it is possible that we may find similar impacts in our sample of older adults. The study objectives were 1) To identify the determinants of psychosocial well-being of people ages 65 and over, and 2) To describe the longitudinal variation in well-being in this population.
Methodology
Study design
This is a longitudinal study with a fixed panel surveyed in three waves. The longitudinal design captures the changes in psychosocial well-being experienced by older adults under conditions of isolation. Fieldwork began on June 20, 2020 (i.e., the 92nd day of isolation) and ended on August 22, 2020 (i.e., the 155th day of isolation). During this period the number of daily COVID-19 cases grew steadily, reaching 1,116 cases per day (up from 541 cases per day at the beginning of the period).
Sampling
A snowball sample was used. As Atkinson, et al. suggest, we made a distinction between snowball sampling as a sampling method or as a contact method and applied it in the latter sense "where techniques of 'chain referral'........ can aid entry to settings where conventional approaches find difficult to succeed" [17]. Our sample procedure initiated by reaching a list of 100 reference people -who would not be surveyed- and requesting them to provide names to form a sampling frame which totaled 603 cases. To mitigate the biases implicit in snowball sampling, the cases to be surveyed were selected by completing a sample with proportions of location, sex, and educational level like those of the population of older adults in the city of Buenos Aires. The sample comprised 356, 332 and 322 participants in the first, second and third waves, respectively, and included men and women living in 45 of the 48 neighborhoods of the city of Buenos Aires. Older adults with hearing disabilities as well as those institutionalized were excluded. The study had a retention rate of 90%.
Data collection
Phone interviewers administered an online questionnaire using the JotForm platform. The questionnaire collected the following information over three waves: symptoms of depression and anxiety [based on a subset of the Clinical Interview Schedule - Revised (CIS-R); activities inside and outside the home and any help dwellers may have received to carry them out; interest in learning the news about COVID-19; means of access to information; use of social media; opinions and feelings about the pandemic and the lockdown; health; physical activity; and fear of contracting COVID-19. Additionally, the questionnaire included questions regarding sociodemographic and housing characteristics (first wave), disability (second wave) and loneliness (third wave). Participants were asked to consider the last seven days when answering questions. Closed and open-ended questions were included in the questionnaire. The questionnaire is available upon request. The average duration of the interviews was 35 minutes. All respondents provided oral informed consent.
Data analysis
Bivariate analyses were conducted to assess the relationships between level of well-being, socio-demographic characteristics, personal situations, and activities of the participants.
A binary logistic regression analysis was conducted to investigate if self-rated health, loneliness, gender, education, COVID-19 news, and social media predicted levels of well-being among older adults. The first step to achieve this objective was the recognition of statistically significant associations between the variance of those variables and the likelihood of having symptoms of anxiety and depression, included in the model as the dependent variable.
Scale of well-being
The CIS-R is acknowledged by the World Health Organization as a tool for the detection and coding of mental illness [18,19] in its international classifier of ICD-10 and ICD-11 diseases [20]. The CIS-R considers the week prior to the interview to record the presence and frequency of symptoms that allows for a comprehensive assessment of anxiety and depression regardless of the presence of a diagnosis of a psychological disorder. It is regularly used in the UK to systematically detect the severity of common [neurotic] mental disorders and their changes in the general population [21].
The application of the CIS-R to systematically collected data regarding the psychological well-being of the general population has been revalidated on different occasions [22,23]. It was applied to obtain evidence of the relationship between the COVID-19 pandemic and psychiatric symptoms in Brazil [24]. The construction of well-being scales from the sum of recorded symptoms has been used and continues to be used in various studies and countries [20,25-29]. The CIS-R is considered a standardized and validated tool that can detect common symptoms of anxiety without the intervention of a specialized mental health professional.
In order to observe older adult's well-being , we used 17 questions from the CIS-R referring to: 1) Constant sadness, 2) General apathy, 3) Unjustified irritability, 4) Lack of hope, 5) Sleep problems, 6) Excessive sleep, 7) Fatigue and general reluctance to perform activities, 8) Tiredness, 9) Difficulty concentrating on basic tasks, 10) Phobias, 11) Increased unjustified appetite, 12) Lack of appetite, 13) Guilt, 14) Panic, 15) Low self-esteem, 16) Lack of meaning in life and 17) Inability to enjoy. The systematic collection of responses to CIS-R questions in the three waves allowed for the creation of a dichotomous well-being scale: high and low levels of well-being. Low level of well-being was operationalized as one or more anxiety and depression related symptoms experienced at least four days per week. High level of well-being was operationalized as cases without any symptoms experienced during most of the week.
Results
The participants in the study are socio-demographically diverse in terms of geographic distribution, educational level, types of households, residence in shantytowns and age. Predominantly, participants have a medium-high level of educational attainment, are mostly women, mostly homeowners, and dwellers in single-person and multi-person households (Table 1).
Levels of well-being according to the number of symptoms
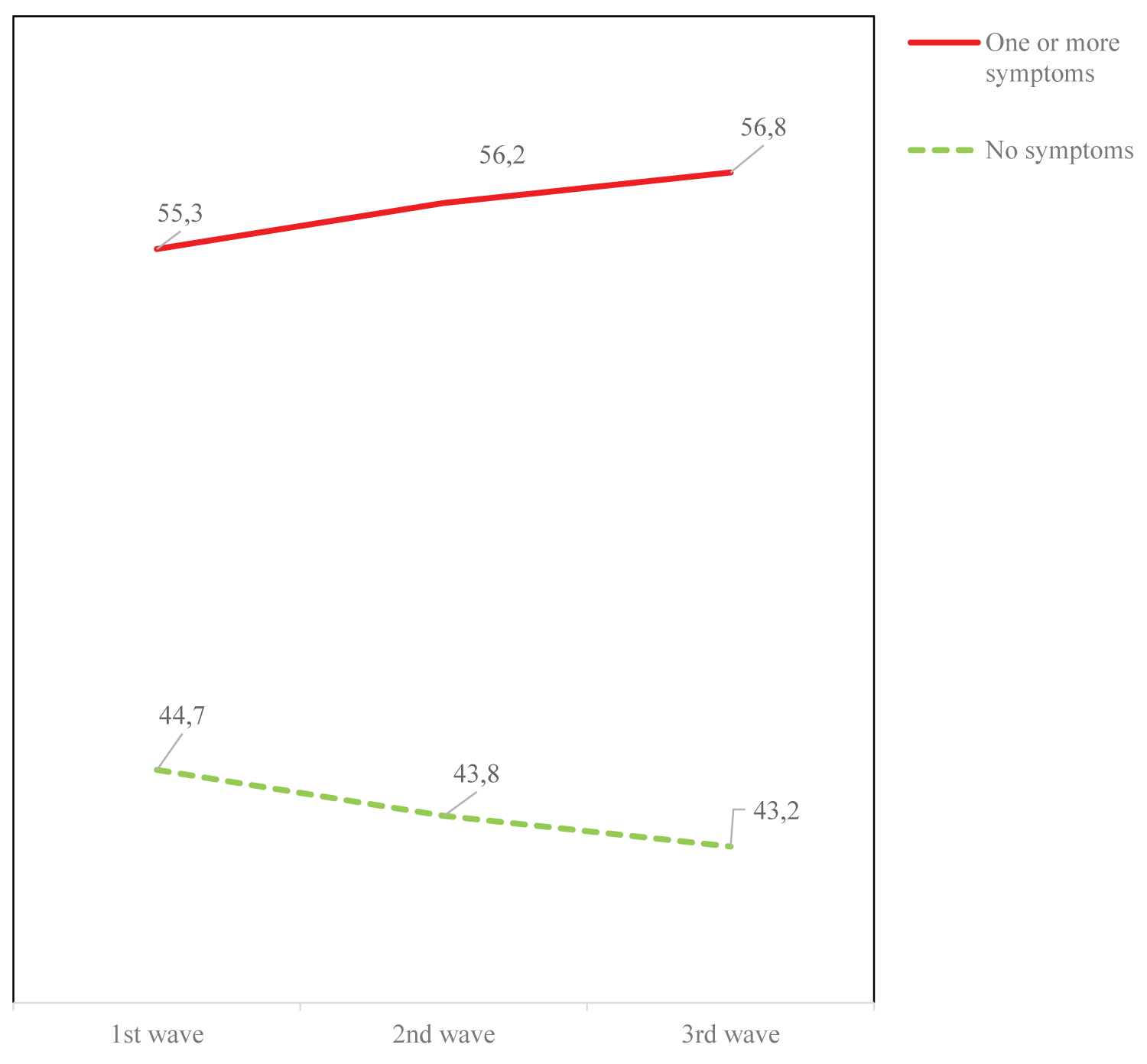
The level of well-being experienced by participants in our sample remained stable across the three waves. In the first wave, 55.3% of the participants experienced at least one of the symptoms four days or more per week. This percentage increased very slightly in the second (56.2%) and third wave (56.8). The relative weights of the two categories had similar values during the overall period of study (Figure 1). There was only a slight growth of 1.5 percentage points in the group with symptoms between the first and last waves.
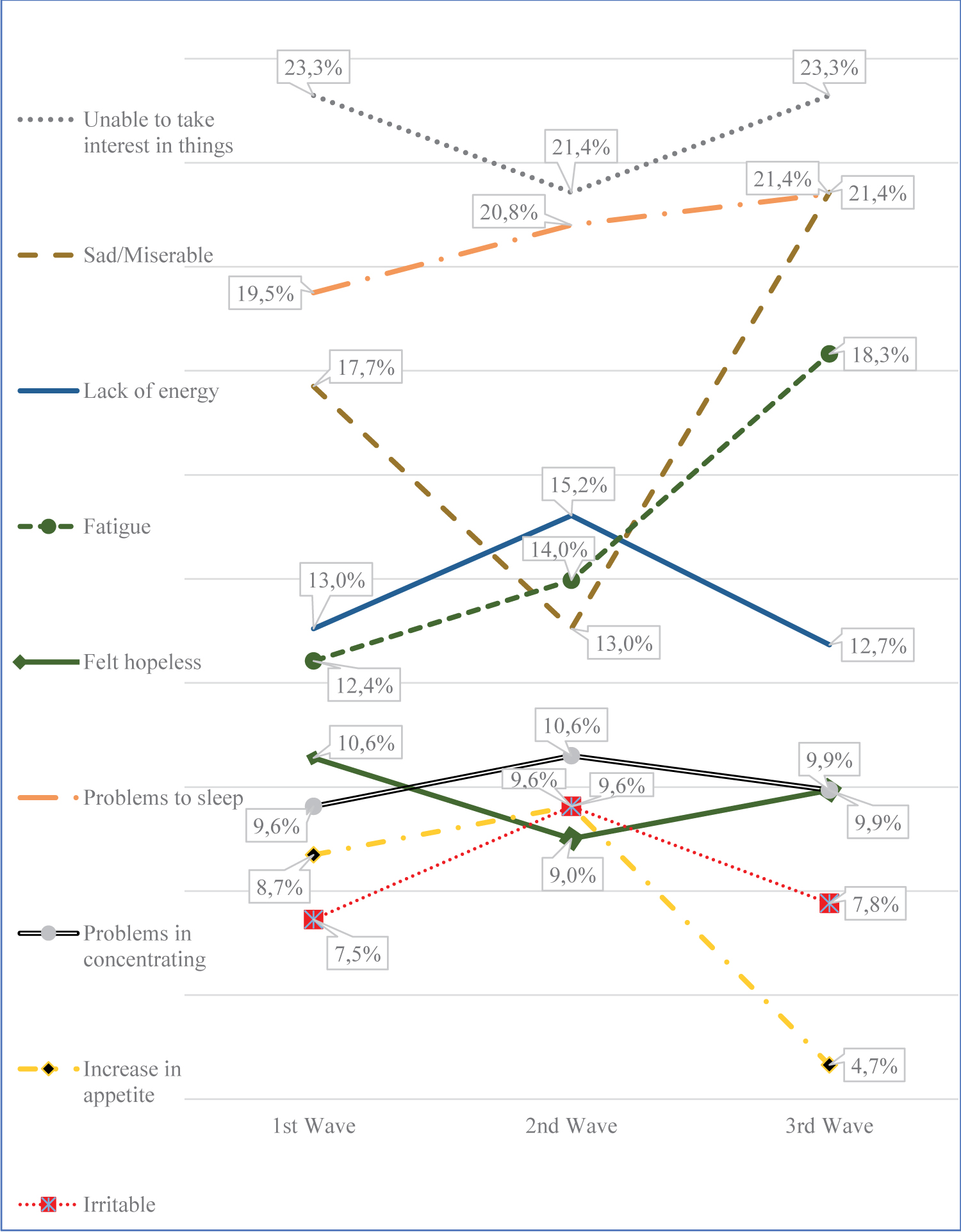
The feeling of apathy -unable to take interest in things- was the most frequent symptom and reached 23.3% of the participants in the first and third waves. Sadness and unhappiness were reported by 21.4% of participants in the third wave. This was 3.7 percentage points more than what was reported in the first wave (17.7%). Fatigue was reported by 18.3% of respondents in the third wave and experienced a growth of 5.9 percentage points over the first wave (12.4%) and is the symptom with the largest variation (Figure 2).
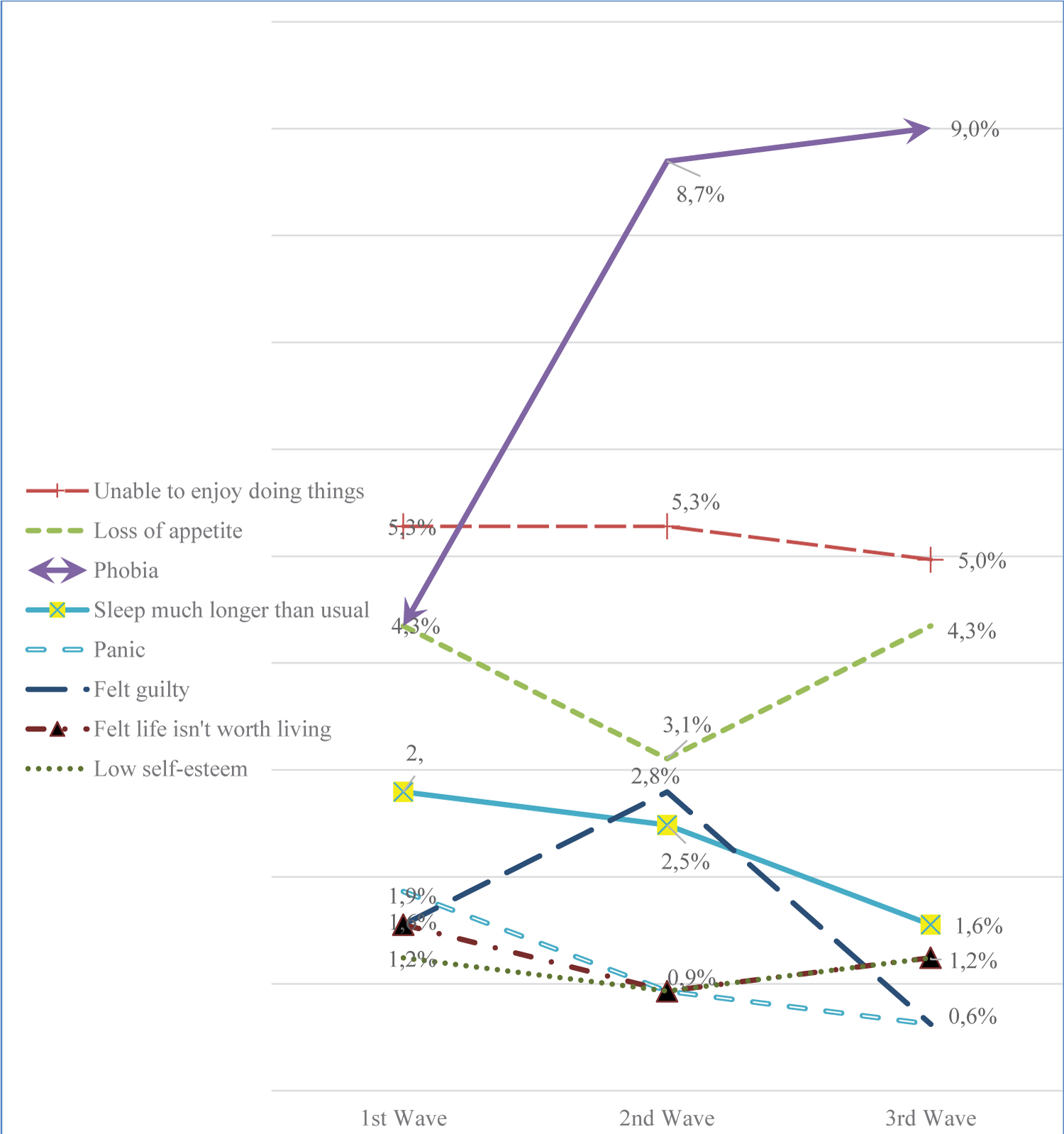
Among the less common symptoms, phobia is the only one with a more than twofold increase. Feelings of guilt, panic attacks, low self-esteem, and lack of meaning in life had been reported by less than 2% of the respondents (Figure 3).
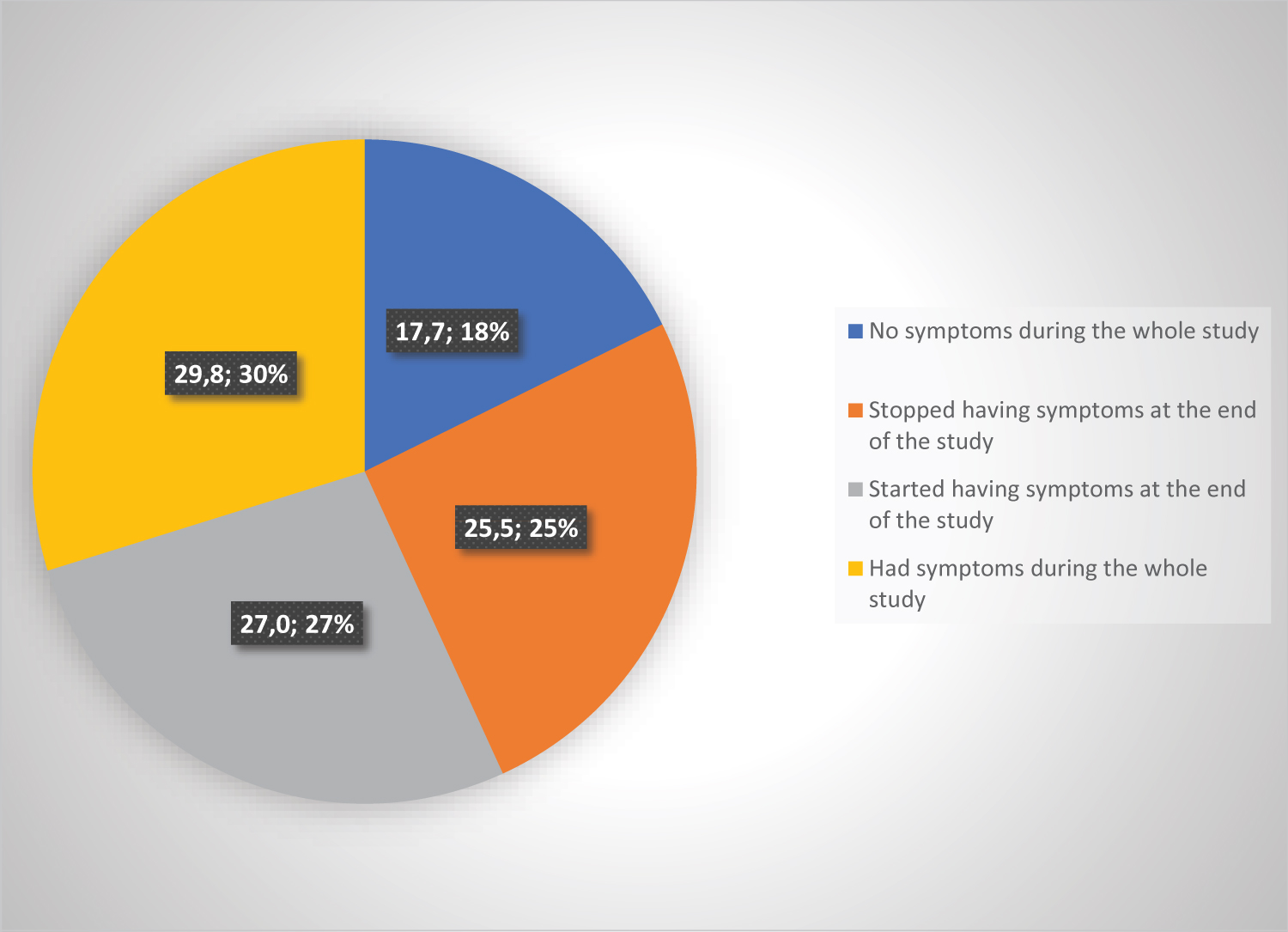
As already stated, the level of well-being remained stable across the three waves. However, the lack of a definite trend does not imply that individual situations remained unchanged. In contrast, as can be seen in Figure 4, in the interval between the 1st and the 3rd waves more than half of the individuals experienced a change in their level of well-being. More than a quarter (27%, 87 cases) of the total sample did not have symptoms in one of the first two waves, but their well-being changed and registered symptoms in the third wave. A similar percentage of people, slightly above a quarter of the sample (25.5%), experienced an improvement in their well-being. They had symptoms in one or two of the waves, but they stopped registering them in the third wave.
Bivariate analysis
Loneliness: Loneliness was measured according to the ten-item UCLA loneliness questionnaire [30] 18.4% of the sample recorded scores of loneliness between 10 and 26 points, representing moderate or high levels of loneliness. 81.6% had scores between 0 and 9 points, representing no or low levels of loneliness. The association between levels of well-being and levels of loneliness is statistically significant (p < 0.01) where the levels of greater loneliness correspond to levels of lower well-being (r = 0.281).
Self-reported health: There is a statistically significant association [p < 0.00] between self-reported health and well-being (r3 = 0.289). In the three waves, 85% of the participants reported a high self-reported health.
Gender
Spearman's coefficients for the association of well-being level and gender are statistically significant (r3 = 0.169). Men experienced greater well-being than women.
COVID-19 news
The association between levels of well-being and watching COVID-19 news is significant in the third wave, that is, after a higher frequency of exposure to the news the level of well-being decreases (r3 = 0.169).
Social media
The use of social media had a statistically significant association with the level of well-being. Social media use was associated with lower levels of well-being (r3 = 0.131).
Other variables
Education, dwelling outings and number of outings, indoor physical activity, outdoor space availability, household size, and age had no significant relationships with the level of well-being (Table 2).
Logistic regression analysis
The following table presents the results of a logistic regression that examine the predictive power of several independent variables on the level of well-being of the respondents (Table 3).
The Hosmer-Lemeshow goodness of fit was not significant [p > 0.05], indicating the model is correctly specified. Additionally, the -2 log likelihood = 362.287 and the Nagelkerke R squared = 0.261. The model resulted in that independent variables, education and social media were not significant (p > 0.05); however, the independent variables self-reported health, loneliness, gender, and COVID-19 news were found to be significant. The independent variables that have more relevance for psychosocial well-being are self-rated health (OR = 8,604, 95%CI: 3.2-52.4), loneliness (OR = 4,084, 95%CI: 2.0-12.2), gender (OR = 2,109, 95%CI: 1.2-3.9) and COVID-19 news (OR = 1,996, 95%CI: 1.1-3.9).
Discussion
Cross-sectional studies carried out during the COVID-19 pandemic have agreed on the existence of observable impacts on psychological well-being in different domains of social life [e.g., economic, and financial factors, quality of life, gender attributes]. In Pakistan, significant predictors of low levels of well-being in women's status, having a chronic illness, being unemployed and fear of COVID-19 were identified, while pointing to coping strategies such as physical activities, healthy eating, participation in family life and carrying out solidarity activities, significantly associated with higher levels of well-being [31]. Another study in 27 countries in Europe concluded that the greater the uncertainty experienced in finance, employment, and housing, the more the subjective well-being and emotional health declined [32]. A study conducted in Turkey concluded that there was a negative and moderate relationship between the fear of contracting COVID-19 and the perception of well-being [33].
Longitudinal studies carried out in Argentina early in the lockdown showed negative impacts on the population. One study, exploring the feelings and expectations aroused by COVID-19 in the population over 18 years of age, identified feelings of fear, uncertainty, and anguish, which particularly affected women [14]. Another study, initiated two days after the beginning of the mandatory isolation, concluded that depression tended to increase slightly while anxiety levels and negative and positive emotions tended to decrease [15]. Unlike these, our results do not exhibit a definite trend of change. The low variation of those who experienced symptoms between the first and third waves (1.5 percentage points) could be due to the advanced moment of the stay at home order timeline in which the information was gathered, i.e., between weeks 13 and 22. Evidence of the existence of a relationship between the period of isolation and changes in levels of emotional well-being has been documented by different studies.
Longitudinal research conducted in England explored the evolution of anxiety and depression throughout the first 20 weeks of isolation. It was found that people ages 60 and over had a nonlinear pattern, in which there was a sharp decline in depressive and anxiety symptoms between weeks 2 and 5, but virtually no change in the final weeks of the study (16 and 20) [34]. More assertively, Prati and Mancini argue that cross-sectional studies do not provide an adequate design to clarify the relationship between isolation and mental health [35]. Their review of 25 longitudinal studies showed that the impacts of social isolation originated due to COVID-19 could vary between different social groups and have small effects on health symptoms. In Argentina, a study collected data at three points in time during the quarantine (days 7-11, days 50-55 and days 115-124). In that study, the symptomatology in the third period was lower than in the two previous periods [13].
In our sample, the prevailing negative feelings, and emotions [i.e., apathy, sadness and unhappiness and lack of energy] are similar to those reported in other studies conducted in the United Kingdom and Argentina [36,37].
Our data show that in the distribution of participants on the well-being scale, the subjective feeling of loneliness plays a prominent role where greater loneliness is associated with a lower level of psychosocial well-being. Our finding is in line with a systematic review of older adults conducted prior to the pandemic [38]. Loneliness was also the most important variable related to symptoms of depression and the second in importance related to anxiety found in a study conducted in Argentina during the first week of social isolation [39].
Self-reported health has been highlighted as "meaningful for contextualizing health status" [40]. As a subjective assessment, it has been consistently linked to health outcomes and to psychological well-being [41]. In our study, its positive association with levels of well-being is consistent with what is established in the literature [42]. Likewise, the lower level of self-reported health in our study is consistent with what was suggested by another research [11,12].
The differences in well-being between men and women observed on the different waves should not be attributed to a cultural issue that postulates that women are more likely to externalize and comment on their problems. This study suggests that the growing gap in the well-being of men and women could be linked to different tasks and attitudes that men and women performed during social isolation. Future studies may look at whether women carried out more domestic activities during quarantine and the potential impact of this change on their well-being.
In line with the observations of Wang, et al. [2] on the use of radio to access information about COVID-19 and higher anxiety and depression, our research also found a negative association between the level of well-being and access to newscasts to obtain information about the pandemic (p < 0.01). Using time to watch newscasts during the pandemic was found to be associated with a lower level of well-being in a study conducted in Ireland [43].
Unlike media exposure, participants increased their use of social media in our study. Social media are more than just disseminators of information and allow a more complex and active interaction with other people, especially in a context of social isolation. An early study conducted during the pandemic in Wuhan, China, concluded that a high prevalence of mental problems was associated with frequent exposure to social media [44].
The association between level of well-being and educational level is not significant, although it is observed that people with higher educational attainment [completed post-secondary education] had a higher level of well-being. This is in line with Ozmen, et al, who reported higher levels of life satisfaction in participants with a higher educational level [33].
In our sample, the number of weekly outings motivated by work activities, purchase of food, banking procedures, medical shifts, walking a pet, doing physical activity or others did not significantly influence the level of well-being. This result contrasts with what was found in a qualitative study conducted in the United States among older adults where exercises and activities outside the home were the most relevant to deal with the challenges of the pandemic [45]. Outings from the house are not associated with the differences in the level of well-being and this suggests that the participating older adults would have developed other adaptive strategies to maintain their well-being within the home, which is unsurprising as willingness to isolate increases with age [46].
Conclusions
This study contributes to the knowledge of the impacts of mandatory stay at home on the well-being of older adults during the COVID-19 pandemic. First, a proper understanding of this conclusion should consider that the time frame has an impact on the variability of the symptomatology. The distribution of well-being levels in older adults between days 92 and 155 of isolation remained relatively constant. Second, the steady values of psychosocial well-being between waves at the sample level coexist with individual instability, suggesting the need to deepen the analysis in that direction.
Personal situations -feeling of loneliness and self-reported health-; socio-demographic factors -gender and education-; and activities -use of social media, watching the news-, influenced the well-being of participants. The feeling of loneliness showed predictive capacity of well-being and, therefore, given that loneliness is enhanced in contexts of social isolation, its inclusion in mitigation policies is suggested. In addition, self-reported health was found to influence levels of well-being. However, subsequent studies should take into consideration the socioeconomic inequalities that affect self-reported health. Gender introduces a differentiation in welfare conditions: men register a higher level of well-being.
Our data show a lower level of well-being among those who used their time to watch newscasts as a source of information about the pandemic. Future research could explore the level of tolerance to a sustained flow of troublesome news, particularly for older adults. The association between lower levels of well-being and the use of digital platforms raises new questions. It may also be considered that the use of social media has increased simply because of the impossibility of doing other activities and that the lower well-being is associated with the lack of those suspended activities.
The strengths of the study are its longitudinal design, the recruitment technique that achieved a relatively heterogeneous participant sample and the high level of retention.
The limitations of the study are the absence of a baseline that would allow for comparing the situations before and after the beginning of the quarantine, having had a single measurement of the loneliness scale, the impossibility of generating extrapolations to the entire city of Buenos Aires and, finally, the exclusion of older adults living in geriatric institutions.
Conflicts of Interest
The authors reported no potential conflict of interest.
Ethics Statement
The Informed Consent was evaluated and approved by the Academic Committee of Bioethics of the National University of Lujan (DISPSEACAD-LUJ: 187-20). Survey participants gave their consent verbally during the telephone interviews.
Funding
This work was supported by the Agencia Nacional para la Promocion de la Investigacion, el Desarrollo Tecnologico y la Innovacion (National Agency for the Promotion of Research, Technological Development and Innovation) [Grant COVID-19 N° 195-2020].
Acknowledgements
We wish to thank Gladys Masse and Maria Cecilia Rodriguez Gauna for their contribution in conceiving the research project, recruiting the sample, and providing valuable input at different stages of the work. We appreciate the insightful comments of Diego Llovet. To Liliana Sella for her support in the analysis of information. Also, our gratitude to the Office of Development and Social Inclusion (Direccion de Desarrollo e Inclusion Social) government of the city of Buenos Aires and the many people that helped us in the recruitment and to all those that patiently answered the questionnaires.
References
- Brooks SK, Webster RK, Smith LE, et al. (2020) The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet 395: 912-920.
- Wang C, Pan R, Wan X, et al. (2020) A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain, Behavior, and Immunity 87: 40-48.
- Anderson RM, Heesterbeek H, Kinkerberg D, et al. (2020) How will country-based mitigation measures influence the course of the COVID-19 epidemic? The Lancet 395: 931-934.
- Cameron-Blake E (2021) Variation in government responses to COVID-19.
- Giacobbe A (2020) Informe mensual especial COVID-19. Buenos Aires.
- Selvarani DR (2020) Survey on people’s perceptions and attitudes. Impact of COVID-19 pandemic and government measures on everyday lives. Buenos Aires.
- G de la CA de BA (2020) Resolución conjunta N.o 16/MJGGC/20.
- Mertens G, Gerritsen L, Duijndam S, et al. (2020) Fear of the coronavirus (COVID-19): Predictors in an online study conducted in March 2020. J Anxiety Disord
- Bu F, Steptoe A, Fancourt D (2020) Loneliness during a strict lockdown: Trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc Sci Med 265: 113521.
- Theo G van Tilburg, Steinmetz S, Stolte E, et al. (2020) Loneliness and mental health during the COVID-19 pandemic: A study among Dutch older adults. J Gerontol B Psychol Sci Soc Sci 76: e249-e255.
- Peters A, Rospleszcz S, Greiser KH, et al. (2020) The impact of the COVID-19 pandemic on self-reported health. Dtsch Arztebl Int 117: 861-867.
- Szwarcwald CL, Damacena GN, de Azevedo Barros MB, et al. (2021) Factors affecting Brazilians’ self-rated health during the COVID-19 pandemic. Cadernos de Saude Publica
- Etchevers MJ, Garay CJ, Putrino N, et al. (2020) Salud mental en cuarentena. Relevamiento del impacto psicológico a los 7-11, 50-55 y 115- 124 días de cuarentena en población argentina. Buenos Aires.
- Johnson MC, Saletti-Cuesta L, Tumas N (2020) Emotions, concerns and reflections regarding the COVID-19 pandemic in argentina. Cien Saude Colet 25: 2447-2456.
- Canet-Juric L, Andrés ML, Valle MD, et al. (2020) A longitudinal study on the emotional impact cause by the COVID-19 pandemic quarantine on general population. Front Psychol 11: 1-17.
- Alomo M, Gagliardi G, Peloche S, et al. (2020) Efectos psicológicos de la pandemia COVID-19 en la población general de Argentina. Revista de la Facultad de Ciencias Medicas (Cordoba, Argentina) 77: 176-181.
- Atkinson R, Flint J (2001) Accessing hidden and hard-to-reach populations: Snowball research strategies. Social research UPDATE, University of Surrey.
- Kendrick T, Simons L, Mynors-Wallis L, et al. (2005) A trial of problem-solving by community mental health nurses for anxiety, depression and life difficulties among general practice patients. The CPN-GP study. Health Technol Assess 9: 1-140.
- McManus S, Bebbington P, Jenkins R, et al. (2016) Mental health and wellbeing in England: Adult Psychiatric Morbidity Survey 2014.
- Goldberg DP, Reed GM, Robles R, et al. (2017) Screening for anxiety, depression, and anxious depression in primary care: A field study for ICD-11 PHC. J Affect Disord 213: 199-206.
- Rai D, Stansfeld S, Weich S, et al. (2016) Comorbidity in mental and physical illness. In: McManus S, Bebbington P, Jenkins R, Brugha T, Mental health and wellbeing in England: Adult psychiatric morbidity survey 2014. NHS Digital, Leeds.
- Lewis G (1994) Assessing psychiatric disorder with a human interviewer or a computer. J Epidemiol Community Health 48: 207-210.
- Das-Munshi J , Castro-Costa E , Dewey M, et al. (2014) Cross-cultural factorial validation of the Clinical Interview Schedule-Revised (CIS-R): Findings from a nationally representative survey (EMPIRIC). Int J Methods Psychiatr Res 23: 229-244.
- Brunoni AR, Suen PJC, Bacchi PS, et al. (2021) Prevalence and risk factors of psychiatric symptoms and diagnoses before and during the COVID-19 pandemic: Findings from the elsa-brasil Covid-19 mental health cohort. Psychol Med 1-12.
- Brugha TS (2002) The end of the beginning: A requiem for the categorization of mental disorder? Psychological Medicine 32: 1149-1154.
- Bebbington P, Dunn G, Jenkins R, et al. (2003) The influence of age and sex on the prevalence of depressive conditions: Report from the National Survey of Psychiatric Morbidity. Int Rev Psychiatry 15: 74-83.
- Subramaniam K, Krishnaswamy S, Jemain AA, et al. (2006) The clinical interview schedule-revised (CIS-R) - Malay version, clinical validation. Malays J Med Sci 13: 58-62.
- Nunes MA, Pinheiro AP, Bessel M, et al. (2016) Common mental disorders and sociodemographic characteristics: Baseline findings of the Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Braz J Psychiatry 38: 91-97.
- Chan WC, Wong CSM, Chen EYH, et al. (2017) Validation of the Chinese version of the revised clinical interview schedule: Findings from Hong Kong mental morbidity survey. East Asian Archives of Psychiatry 27: 3-10.
- Velarde-Mayol C, Fragua-Gil S, García-de-Cecilia JM (2016) Validación de la escala de soledad de UCLA y perfil social en la población anciana que vive sola. Semergen 42: 177-183.
- Khan AA, Lodhi FS, Rabbani U, et al. (2021) Impact of Coronavirus Disease (COVID-19) Pandemic on psychological well-being of the pakistani general population. Frontiers in Psychiatry 11: 1-10.
- Lee S (2020) Subjective well-being and mental health during the pandemic outbreak: Exploring the role of institutional trust. Res Aging 44: 10-21.
- Özmen S, Ozkan O, Ozer O, et al. (2021) Investigation of COVID-19 fear, well-being and life satisfaction in Turkish society. Soc Work Public Health 36: 164-177.
- Fancourt D, Steptoe A, Bu F (2020) Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: A longitudinal observational study. The Lancet Psychiatry 0366: 1-9.
- Prati G, Mancini AD (2021) The psychological impact of COVID-19 pandemic lockdowns: A review and meta-analysis of longitudinal studies and natural experiments. Psychol Med 51: 201-211.
- Kleinberg B, van der Vegt I, Mozes M (2020) Measuring emotions in the COVID-19 real world worry dataset. Global Survey.
- P.S.A. (2020) 70 días de cuarentena: salud mental, economía y gestión política. Buenos Aires.
- Dahlberg L, Mcknee KJ, Frank A, et al. (2021) A systematic review of longitudinal risk factors for loneliness in older adults. Aging Ment Health 26: 225-249.
- Torrente F, Yoris A, Low DM, et al. (2021) Sooner than you think: A very early affective reaction to the COVID-19 pandemic and quarantine in Argentina. J Affect Disord 282:495-503.
- Brown TN, Turner RJ, Moore TR (2016) The multidimensionality of health: associations between allostatic load and self-report health measures in a community epidemiologic study. Health Sociology Review 25: 272-287.
- Ryff CD, Radler BT, Friedman EM (2015) Persistent psychological well-being predicts improved self-rated health over 9-10 years: Longitudinal evidence from MIDUS. Health Psychol Open
- Maheswaran H, Kupek E, Petrou S (2015) Self-reported health and socio-economic inequalities in England, 1996-2009: Repeated national cross-sectional study. Soc Sci Med 136-137: 135-146.
- Lades LK, Laffan K, Daly M, et al. (2020) Daily emotional well-being during the COVID-19 pandemic. Br J Health Psychol 25: 902-911.
- Gao J, Zheng P, Jia Y, et al. (2020) Mental health problems and social media exposure during COVID-19 outbreak. PLoS One
- Finlay JM, Kler JS, O’Shea BQ, et al. (2021) Coping during the COVID-19 pandemic: A qualitative study of older adults across the United States. Front Public Health 9: 643807.
- Daoust J F (2020) Elderly people and responses to COVID-19 in 27 Countries. PLoS One 15: 1-13.
Corresponding Author
Ignacio Llovet, PhD, Departamento de Ciencias Sociales, Universidad Nacional de Lujan, Argentina, Ruta 5 y Avenida Constitucion - (6700) Lujan, Buenos Aires, Argentina, Tel. (+54)-911-55633585
Copyright
© 2022 Llovet I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.