An Unusual Case of Acute Postoperative Hypokalemic Thyrotoxic Periodic Paralysis
Abstract
Thyrotoxic periodic paralysis (TPP) is an acute condition characterized by sudden onset of muscle weakness and paralysis in the setting of hypokalemia. This condition has the highest incidence in Asian males but is becoming increasingly common in individuals of different ethnicities as well. Herein, we present a unique case of a Hispanic male with no previous medical history of hyperthyroidism presenting with symptoms of TPP due to a hypothesized postoperative catecholamine surge. This case highlights the importance of recognizing and treating this condition early to prevent dangerous complications such as arrhythmias and respiratory failure.
Keywords
Thyrotoxicosis, Periodic paralysis, Hypokalemia, Hypomagnesemia, Hypophosphatemia
Introduction
Thyrotoxic periodic paralysis (TPP) is usually found in men of Asian descent in the third to fifth decade of life. TPP is typically characterized by sudden onset hypokalemia and proximal skeletal muscle paralysis affecting more commonly the lower extremities [1]. Episodes may vary in the frequency of occurrence, intensity and length of time for each episode. The duration of each may vary for a few hours to days. In the setting of hypokalemia from intracellular potassium shifts via Na+/K+-ATPase pumps, patients may also present with arrhythmia and decreased reflexes [1]. It is found that thyrotoxic patients with paralytic episodes have higher Na+/K+-ATPase activity, catecholamine surges, and elevated androgen levels. Among the known precipitating factors are carbohydrate rich meals, high sodium content meals, stress, corticosteroid use and strenuous exercise [1]. In our patient's case, we suspect postoperative catecholamine surge in the setting of undiagnosed, undetected hyperthyroidism precipitating a hypokalemic thyrotoxic periodic paralytic attack.
Case Presentation
A 44-year-old Hispanic male with a past medical history of urethral stricture status post recent urologic dilation and foley insertion presented with bilateral lower extremity weakness 1 day postoperatively. The patient reported that immediately after the procedure he had no difficulty moving any of his extremities and was able to ambulate with ease. However, muscle weakness began that night on the same day of surgery, which was one day prior to hospitalization. The patient described the onset of weakness in his legs which progressed to his shoulder girdle muscles. At this time, he attributed the weakness to the anesthesia not fully wearing off. The next morning, the weakness progressed until it rendered him unable to stand or ambulate steadily, as he also experienced difficulty turning his head. He endorsed one episode of palpitations and anxiety during this time. He denied paresthesias, sensation loss, traumatic injuries, convulsions, incontinence and dyspnea. He also denied the use of medications, tobacco, alcohol, or illicit drugs. Prior to this particular episode, he had never had any symptoms associated with hypothyroidism such as temperature intolerance, hair or skin changes, hand tremors or changes in bowel habits.
Family history was only significant for a niece with unspecified thyroid problems. The patient's vital signs at this time were a temperature of 37.5 °C, blood pressure of 135/98 mmHg, heart rate of 105 bpm, respiratory rate of 18 bpm and an oxygen saturation of 95% on room air. The patient was not obese as his body mass index was 25.96.
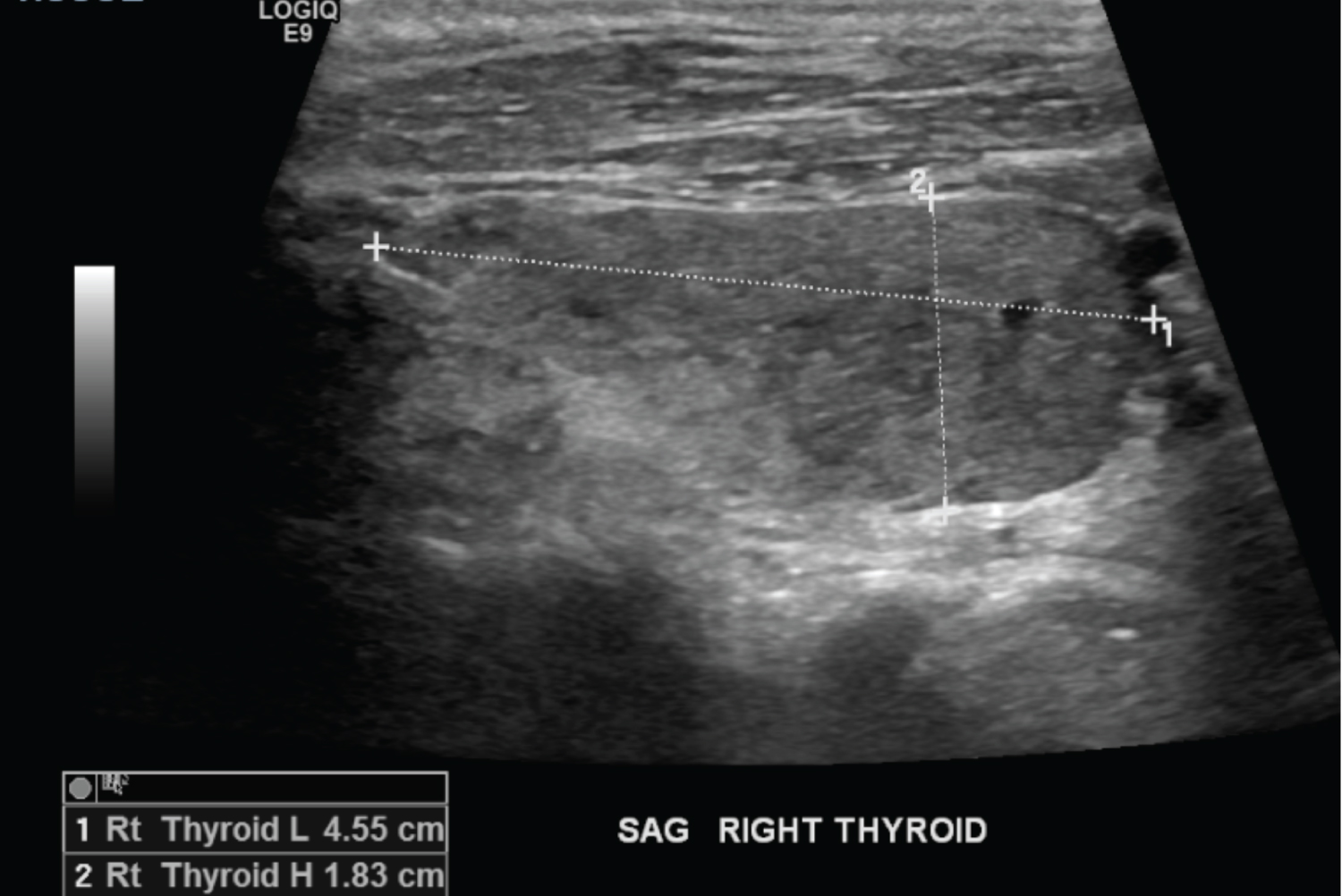
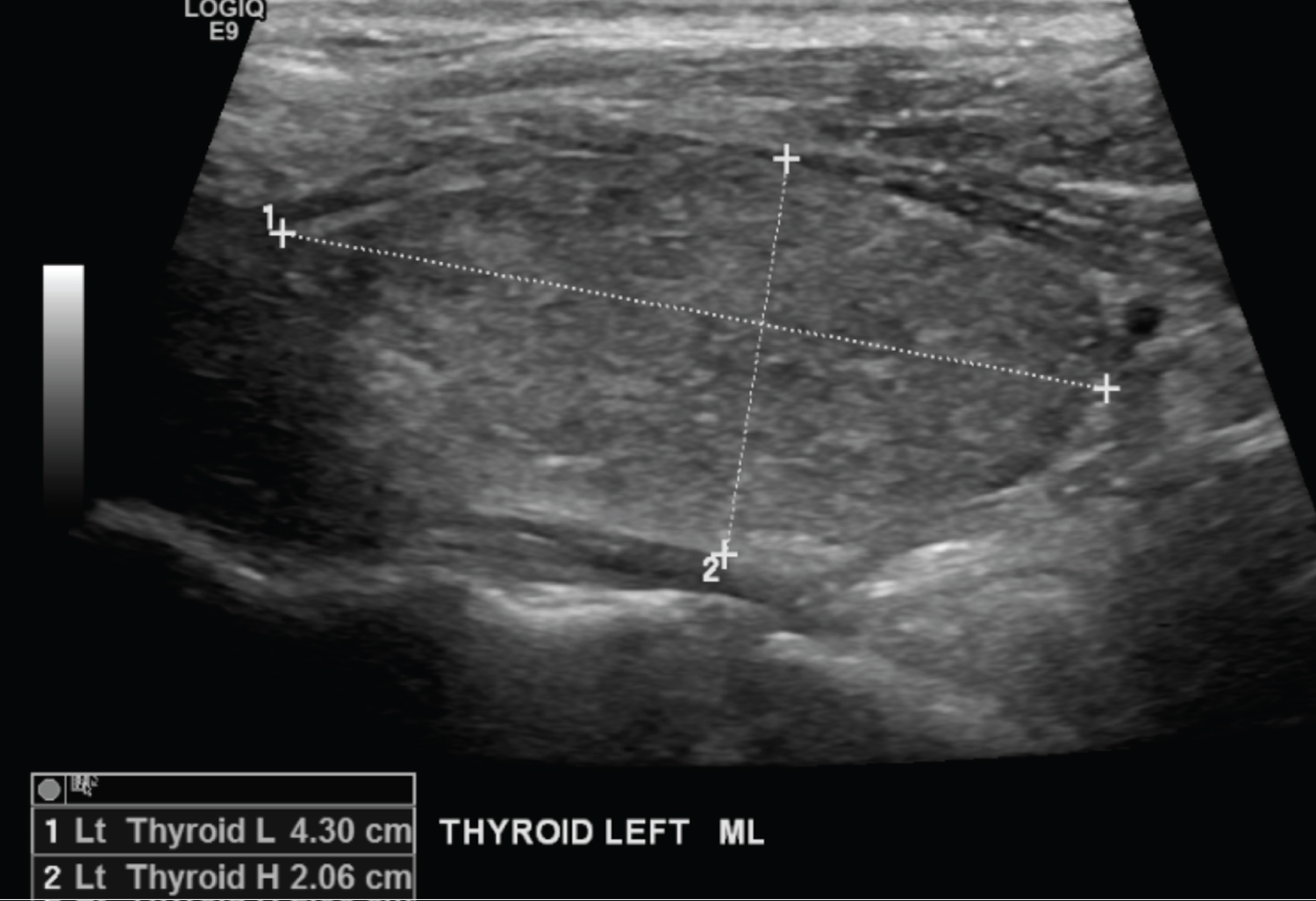
Physical exam revealed no ophthalmic or thyroid abnormalities, intact sensation, normal muscle bulk and tone, but mildly diminished reflexes with decreased strength 1/5 in the bilateral proximal and distal lower extremities. The laboratory results were significant for hypokalemia (1.7 mEq/L), hypomagnesemia (1.6 mg/dL), hypophosphatemia (1.4 mg/dL) and lactic acidosis (3.9 mmol/L). He was also found to be in a hyperthyroid state as his thyroid stimulating hormone was less than 0.01 mIU/mL, free T3 was 6.1 pg/mL, total T3 was 1.22 ng/mL and free T4 was 2.96 ng/dL. The electrocardiogram (EKG) was obtained and revealed to be normal sinus rhythm with a ventricular rate of 97, with prominent U waves, and a prolonged QTc of 524 ms. The computed tomography (CT) of the head did not reveal any intracranial pathologies. The thyroid ultrasound revealed the echotexture was somewhat heterogeneous and there was significant bilateral hypervascularity suggestive of thyroiditis (Figure 1). The right thyroid lobe was 4.5 cm in length, 1.8 cm in height, and 2.3 cm in width (Figure 2). The left thyroid lobe measurements were 4.3 cm in length, 2.1 cm in height, and 1.8 cm in width (Figure 3). The thyroid isthmus was 3 mm in thickness. Given the combination of abnormal thyroid, hypokalemia, hypomagnesemia, and abnormal QTc, the patient required intensive care unit (ICU) admission. Prior to the ICU admission, the patient was repleted in the emergency department with MgSO4 2g IV, K-Phos 15 mmol IV, and KCl 40 mEq PO. Hydration was achieved with the administration of a 2 liter normal saline bolus and the patient was started on cefepime. In the ICU ward, the patient received an additional 40 mEq of intravenous potassium. The endocrinology team was consulted immediately and they recommended the initiation of methimazole and propranolol for thyrotoxic periodic paralysis.
Cardiology was also consulted at this time due to elevated troponins and a QTc prolongation. The patient was transferred to the medical floor from the ICU after 2 days and subsequently discharged the following day after being cleared by both cardiology and endocrinology. On outpatient follow-up two weeks after discharge, the patient was clinically stable and asymptomatic.
Discussion
Thyrotoxic periodic paralysis (TPP) with hypokalemia and acute proximal muscle weakness is an endocrine emergency which is becoming an increasingly common condition in the western countries. While this phenomenon has the highest incidence in individuals of Asian descent, it is beginning to present with greater frequency among other ethnicities [1]. Various etiologies have been proposed for this condition, such as increased Na+/K+-ATPase activity, rapid intracellular shift of K+, increased catecholamines, and calcium-channel α1-subunit gene polymorphisms [2,3]. The etiologies of TPP can make the diagnosis challenging among patients with varying clinical presentations. For instance, only up to 50% of TPP patients show clinical signs of hyperthyroidism [2].
However, given that this condition can result in life-threatening dysrhythmias in the setting of hypokalemia and respiratory failure following flaccid muscle paralysis, it is still important to recognize this acute presentation and initiate immediate treatment [1,2]. The proposed etiology for our patient's presentation was a postoperative catecholamine surge in the setting of an undiagnosed hyperthyroidism. The patient's lower extremity and shoulder girdle weakness preceded his inability to ambulate, which began the same day following his surgery. He had no prior history of hyperthyroidism or any other endocrine pathology. It was critical the patient be hospitalized with this clinical presentation in the ICU due to the numerous life-threatening complications. Due to the severe electrolyte abnormalities, hormone dysregulation and changes in diagnostic test results, obtaining labs and imaging in a timely manner is essential to addressing the etiology and initiating therapy. This was seen in our patient as his labs revealed a decreased TSH, increased T3 and T4 hormone levels, hypokalemia, hypomagnesemia, and hypophosphatemia. Additionally, the EKG showed prominent U-waves and a prolonged QTc characteristic of a severe hypokalemic state. Shih-Hua Lin, et al. described administration of oral propranolol 3 mg/kg in 2 patients with acute TPP was able to completely terminate neuromuscular paralysis with no rebound hyperkalemia nor hyperphosphatemia [4]. Therefore, a nonselective β-blocker such as propranolol can be used to rapidly correct potassium and phosphate levels. Furthermore, antithyroid medications, radioiodine therapy, or surgical thyroidectomy may be indicated to achieve an euthyroid state and prevent TPP recurrence [2,5]. Early recognition of TPP symptoms and correction of the electrolyte disturbances associated with this condition are crucial to prevent the lethal complications that can result from its progression such as arrhythmias and respiratory failure. It is especially important to recognize the clinical picture of TPP because it is increasing in incidence among individuals of diverse ethnic groups, geographic areas, and clinical backgrounds [6].
Conclusion
Although TPP has varying presentations, obtaining laboratory studies, diagnostic testing and a thorough physical exam can aid in identifying this endocrine emergency and initiating treatment. Both electrolyte abnormalities and a thyroid ultrasound can be used in differentiating TPP from other clinically similar conditions. It is important for clinicians to keep TPP in the differential in a postoperative patient presenting with acute paralysis, as a delay in the diagnosis can be lethal due to potential arrhythmias and respiratory failure. Therefore, early recognition and management with antithyroid medications is crucial in abating progression of the illness.
Financial Disclosure or Funding
No funding was provided to any of the authors.
Conflict of Interest
The authors declare that they have no conflicts of interest.
Informed Consent
Informed consent was obtained from the patient for the purpose of this case report.
Author Contributions
All authors contributed to the literature review, production and revision of the manuscript.
References
- Lin S-H (2005) Thyrotoxic periodic paralysis. Mayo Clinic Proceedings 80: 99-105.
- Bilha S, Mitu O, Teodoriu L, et al. (2020) Thyrotoxic periodic paralysis-a misleading challenge in the emergency department. Diagnostics 10: 316.
- Kung AWC (2006) Thyrotoxic periodic paralysis: A diagnostic challenge. The Journal of Clinical Endocrinology & Metabolism 91: 2490-2495.
- Lin SH, Lin YF (2001) Propranolol rapidly reverses paralysis, hypokalemia, and hypophosphatemia in thyrotoxic periodic paralysis. Am J Kidney Dis 37: 620-623.
- Meseeha M, Parsamehr B, Kissell K, et al. (2017) Thyrotoxic periodic paralysis: A case study and review of the literature. J Community Hosp Intern Med Perspect 7: 103-106.
- Al Moteri BL, Aslam M (2017) Thyrotoxic periodic paralysis: A case report. Int J Health Sci (Qassim) 11: 1-2.
Corresponding Author
Sahil Zaveri, MD, Department of Internal Medicine, St. Joseph's University Medical Center, Paterson, New Jersey 07470, USA, Tel: 973-754-2000
Copyright
© 2022 Mora I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.