Two Week Rule Compliance: Assessing General Practice Use of the 'Two Week Rule' Referral Pathway for the Suspicion of Colorectal Cancer
Abstract
Background: The 'Two-Week-Rule' (TWR) for referring patients with a suspicion of colorectal cancer (CRC) was implemented in 2000 to improve CRC survival rates. Guidelines exist to assist general practitioners (GPs) identify patients based on high-risk symptomology. Our aim was to evaluate the effectiveness of these guidelines, to determine whether a correlation exists between individual criteria within the guidelines and CRC, and to assess GP compliance of guidelines in referring symptomatic patients.
Methods: 485 consecutive 'TWR' referrals to colorectal unit in a district general hospital and all patients diagnosed with CRC or high grade dysplasia (HGD) regardless of referral route, were prospectively collected between July and December 2015. Both lists were independently maintained and retrospectively analysed. Results were cross-examined for accuracy and main measures include: reason(s) for referral, secondary-care investigation(s) and diagnoses.
Results: GPs referred 333 patients based on symptomology suggestive of CRC; while referring an additional 152 patients (31.3%) that failed to meet NICE guidelines for TWR referral. CRC or HGD was diagnosed in 28 patients; 27 of whom (96.4%, p = 0.0005) were identified through a guideline compliant referral. During the study period 79 cases of CRC or HGD were diagnosed from all referral routes; 36.7% through the 'TWR' referral pathway.
Conclusion: Updated NICE referral guidelines for suspected CRC appear to be effective in identifying patients with CRC based on high-risk symptomology. Guideline compliance from GPs remains a barrier in the 'TWR' referral system. GPs paradoxically over-refer guideline non-complaint patients, while under-referring guideline complaint patients; reducing the effectiveness of the 'TWR' referral system.
Keywords
Colorectal cancer, Two week rule, Urgent referral, GP compliance
Abbreviations
CRC: Colorectal cancer; DOH: Department of health; TWR: Two-week-rule; GPs: General practitioners; NHS: National health service; NICE: National institute for health care and excellence; HGD: High grade dysplasia; IDA: Iron deficiency anaemia; CIBH: Change in bowel habit.
Introduction
Colorectal cancer (CRC) is a significant and increasing health problem in the western world. In 2012, 42,000 new cases of CRC were diagnosed in the UK, a rate of almost 115 cases per day [1]. Moreover, CRC remains the 4th most prevalent cancer and 2nd leading cause of cancer mortality in the UK [1]. It has long been accepted that early diagnosis and treatment improves the chances of survival [2]; yet to date, many patients still present with advanced stages of the disease and only 60% of new diagnoses have a five-year survival rate [3].
In 2000, the survival rates for colorectal cancer in the UK were lower than those in the United States and the rest of Europe [4]. The Department of Health (DOH) took steps to ensure that patients presenting with symptoms indicative of cancer could be seen within two-weeks by a hospital specialist [5]. To facilitate this 'two-week-rule' (TWR) guidelines of high-risk criteria were drafted to assist general practitioners (GPs) identify patients for fast-tracked referrals. The program aimed to reduce delays in diagnosis by identifying patients displaying high-risk symptomology at an earlier stage of disease and thus improve treatment outcomes. Simultaneously, the National Health Service (NHS) Cancer Plan required health services meet the 'TWR' for fast-track referrals in 95% of cases [6] and for the guidelines to identify 90% of all CRC patients [6,7]. Since 2005, The National Institute for Health Care and Excellence (NICE) has continued to update these guidelines, most recently in 2015 (NG12) [8] which are summarized in Table 1.
Since the implementation of referral guidelines for suspected CRC, debate regarding their effectiveness continues. In 2004, Flashman, et al. [7], demonstrated that two week urgent referral clinics provided a greater CRC diagnostic yield over routine outpatient clinics at 9.4% and 2.2% respectively [7]. A review of 24 CRC studies [9] confirmed this diagnostic yield for two week referral clinics (9.5%), while demonstrating that this accounts for only 32.2% of all CRC diagnoses. An earlier review [10] found similar results but further identified that the remaining CRC diagnoses were referred as either emergency cases (24.1%) or via other routes (52.4%). From this it is clear the majority of the colorectal cases are diagnosed outside the fast-track referral system and although studies [7,11-13] have shown a correlation between referral criteria and CRC, clinicians have remained critical of the guidelines; arguing poor specificity as a major factor in their low overall rate of CRC detection [14,15].
Poor compliance with the guidelines has aided in the poor cancer detection rates and a growing number of 'TWR' referrals. Although, a positive and significant reduction in time required to see a specialist and receive treatment has occurred via the 'TWR' referral pathway [7,16], many patients diagnosed with CRC continue to miss the 62-day definitive treatment guideline [7,16,17] set out by the 2005 NHS Cancer Plan [6]. Increases in service demand due to guideline non-compliant referrals are a likely contributor to this trend. When CRC referral guidelines are used correctly, the diagnostic frequency of 'TWR' referrals has been shown to improve significantly [11,14,16,18]; in one study to nearly 86% [11]. By improperly referring patients, GPs regulate specialist resources, increase wait times for non-urgently referred patients [14,19] and delay diagnoses in high-risk patients. To date, little research has been done to explore why GPs may misinterpret or disregard referral guidelines.
Research into colorectal cancer has however, resulted in the development of a well defined histopathological classification system known as adenoma-carcinoma sequence [20]. Progression from normal intestinal mucosa to carcinoma is a step-wise genetic evolution in which dysplastic changes occur, transitioning normal colonic epithelium from adenoma to carcinoma. Although benign, adenomatous polyps increase in malignant potential with the level of dysplasia [21], from low to high grade. In large adenomatous polyps it is often difficult to determine whether the polyp is solely dysplastic or malignant due to the limited penetrability of a biopsy. Therefore, clinicians often use a similar approach when dealing with high grade dysplasia (HGD) as they do with CRC.
In light of these previous studies, and with the recent publication of updated NICE guidelines, we conducted an audit investigating the compliance and effectiveness of 'TWR' referrals pathway for patients with an urgent suspicion of colorectal cancer. Primary aims were to evaluate the effectiveness of these guidelines, to determine whether a correlation exists between individual criteria within the guidelines and CRC, and to assess GP compliance of guidelines in referring symptomatic patients. Secondary objectives were to determine the number of fast track referrals received within a set time frame, the diagnostic yield of the 'TWR' referral pathway, and how this pathway compared to other pathways in terms of diagnosing CRC.
Materials and Methods
This was a retrospective cohort study of all consecutive 'TWR' referrals received for CRC over six months period (1st July to 31st December 2015) and all patients diagnosed of CRC or HGD within the study period regardless of referral pathway in a single district general hospital. Both sets of patients were identified using prospectively maintained lists, collected independently by the regional cancer pathway supervisor and in-hospital colorectal cancer database respectively. The authors of this study had no role in maintaining either of the prospective databases; and cross-checks were carried out between both lists to ensure the accuracy of results. All patients who were referred and where a diagnosis was made were included in the study. Patients that failed to respond to either the centralized booking team's phone or written correspondence for a period of three months were classified as having declined investigation. Nineteen patients (3.9%) were excluded from the study, as they are currently awaiting investigation; having cancelled or missed appointments delaying their diagnosis or where initial investigations where inconclusive.
Microsoft Excel was used to create a database, patients' demographic data, indication(s) for referral, secondary-care investigation(s), diagnoses and respective dates were collected from patient clinical records. Clinical indication(s) for referral and diagnoses were separately assessed by one author to ensure universality and to avoid bias but consensus between authors was obtained when uncertainty arose, to avoid inter-observer variability. Non-'TWR' referrals were categorized as either: screening, A&E admission, GP admission, GP urgent referral (consultation within 4-weeks), GP routine referral (consultation within 18 weeks) or from other speciality. Chi-squared test was used for analysis and to calculate p-values. Results were considered statistically significant at p-values less than 0.05.
Due to biopsy limitations associated with larger polyps, sub-group analysis was used, displaying results for both CRC and HGD, where appropriate. When assessing GP compliance, referral symptoms were assessed against the NICE Guidelines for suspected colorectal cancer and was carried out before analyzing a patient's diagnosis to eliminate any observation bias.
This study was registered with the NHS Lanarkshire Clinical Quality Project, project id: 13276. As this was a retrospective observational study patient consent was not required.
Results
Patients demographics
A total of 485 patients with mean age 65.4 years (median age 67 years) were referred via 'TWR' pathway with an urgent suspicion of colorectal cancer (Table 2). 216 were male (44.5%, age range: 29-94 years) and 269 were female (55.5%, age range: 21-95 years). During the same period, 79 patients (mean age 70.0 years, median age 73) from all referral pathways were diagnosed with either CRC or HGD; 49 were male (62.0%, age range: 33-86 years) and 30 were female (38.0%, age range 50-95 years).
Diagnostic outcomes
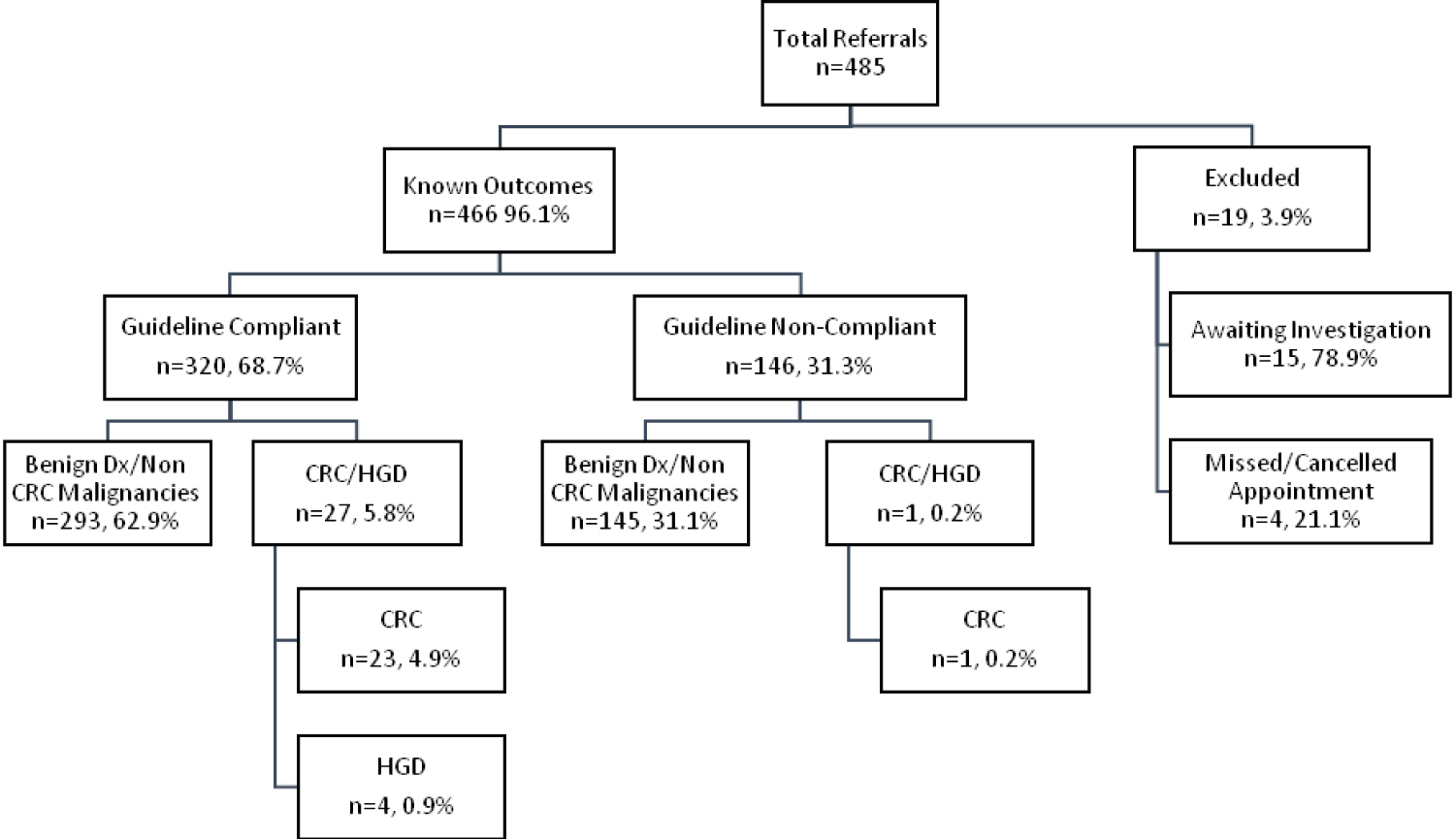
Of the 485 patients referred as TWR, 19 (3.9%) were excluded. 320 (68.7%) referrals complied with NICE guidelines and additional 146 referrals (31.3%) were non-compliant with NICE guidelines. Diagnoses, summarized in Figure 1 and Table 3, were identified in 96.1% (n = 466) of patients. CRC or HGD was diagnosed in 6.0% (n = 28, 24 and 4 respectively) of referrals; 27 of which (96.4%, p = 0.0005) were identified following a guideline compliant referral. Other diagnoses identified included: Diverticular disease (23.8%), haemorrhoids (8.2%), polyps with low grade dysplasia (8.4%), hyperplastic polyps (4.1%), and unrelated malignancy (0.9%). Polyp were completely excised but not retrieved in seven patients.
Guideline criteria
278 (86.9%) referrals met one of the published NICE Guideline criteria, while 42 (13.1%) referrals were referred on the bases on two or more criteria. When assessing for a correlation between individual guideline criteria and CRC or HGD; patients awaiting investigations, declining or unsuitable for investigation were not included. Criteria 2 (PR bleeding, age > 50), Criteria 3 (iron deficient anaemia and/or change in bowel habits, age > 60), and Criteria 5 (rectal or abdominal mass) were seen in 33.3%, 74.1% and 14.8% of patients diagnosed with CRC or HGD respectively (Table 4); however, statistical significance was not observed.
Routes of referral
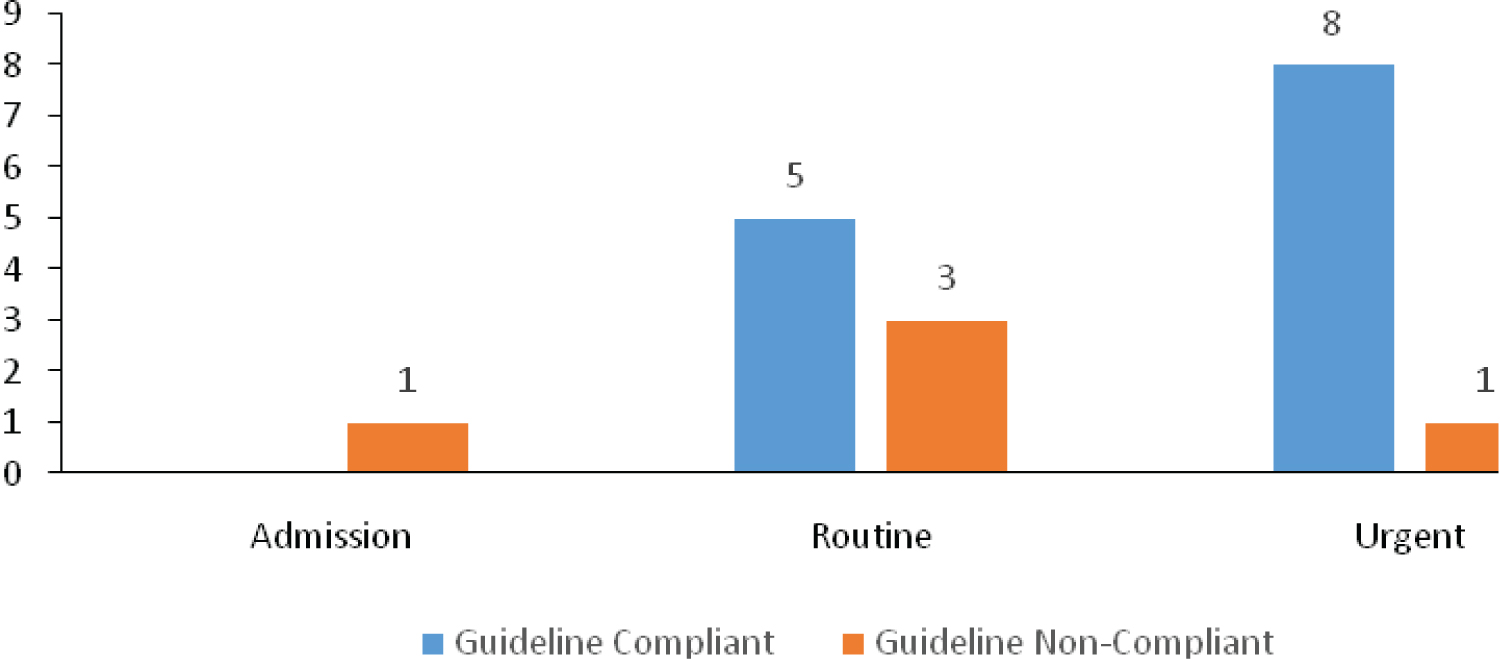
Overall, 79 cases of known CRC and HGD were diagnosed from all referral routes during the study period (Table 5). 37.9% of CRC diagnoses were diagnosed through the 'TWR' referral pathway and was higher than the 32.2% reported in a recent meta-analysis [9] from 2009. The majority of CRC diagnoses observed in our study were identified through alternative routes; with other GP referrals (24.2%), screening (19.7%) and A&E (12.1%) accounting for the majority. Of interest, 13 patients diagnosed with CRC or HGD and referred by GPs outside the 'TWR' pathway, actually met the guidelines for fast-tracked referrals (Figure 2); however they were referred as routine.
Discussion
The 'TWR' was developed with the intention of decreasing wait times while expediting diagnosis and treatment [22] in patients displaying high-risk symptomology suggestive of CRC. Current and previously published guidelines, are evidence-based and intended to assist GPs in determining the urgency of referrals.
Our audit, based on recently published guidelines, has demonstrated that 4.9% of 'TWR' referrals result in a diagnosis of CRC; accounting for a much lower proportion than the 9.5% previously reported in a review of 24 CRC studies [9]. When non-compliant referrals are removed and HGD is included, this increases to 8.4%, but remains below the published mean which includes non-compliant referrals. Although our study demonstrates a lower diagnostic yield than in previous studies, we found statistical significance with the majority of CRC or HGD diagnoses (96.4%, 27/28, p=0.0005) made following guideline-compliant referrals. Coupled with previous studies [11,16,18,22,23] this result demonstrates the value of 'TWR' system when used appropriately in identifying at-risk symptomatic patients.
The 'TWR' referral system relies heavily on GPs awareness and compliance of guidelines; failure to follow guidelines reduces the effectiveness of the system in achieving its intended objectives. Publications [16,18,24,25], demonstrate varying levels of referral non-compliance ranging between 25-49%, which is consistent with the 31.3% non-compliance observed, in this study. Retrospective analysis of all non-compliant referrals (n = 152), shows that 123 referrals or 80.9%, met the criteria for GPs to offer pre-referral faecal occult blood testing; an established method for screening patients to reduce colorectal cancer mortality [26]. If such testing had been carried out, more appropriate referrals for these patients could have been made; reducing the number of 'TWR' referrals received in specialty clinics, subsequent strain on clinic resources and undue stress placed on patients due to these fast-tracked referrals.
Of the patients diagnosed with CRC, 37.9% were referred via the 'TWR' pathway; which is slightly higher than the 32.2% published in a meta-analysis of 18 studies [9], but far below the 90% target established back in 2000 from the Department of Health. Further analysis of patients referred less urgently from GP and diagnosed with either CRC or HGD, indicates that 72.2% (n = 13) were incorrectly referred; having displayed high risk-symptomology and warranting of a 'TWR' as outlined in the guidelines. However, it is important to note that their downgraded referral urgency likely posed minimal risk to the patient, as research has shown that the urgency of referral fails to identify tumors at an earlier Dukes staging [18]. It does further highlight a trend towards non-compliance and questions the maximum effectiveness of the 'TWR' system.
This study did not attempt to determine why GPs appear to disregard guidelines; however, heavy workloads within general practice [27] have been suggested. Some studies have elaborated, suggesting guidelines require additional work on the part of GPs [28], a lack of awareness of the guidelines [29] or an incorrect interpretation [9] as possible reasons. GPs have also shown a desire to expedite wait-times for patients displaying low-risk symptomology [9] and indicative of other colorectal pathologies; patients who would be otherwise non-urgently referred. When warranted however, this is the role of an 'urgent' referral and not a 'two-week' referral, as the 'TWR' pathway is uniquely intendment for patients with a suspicion of CRC.
Analysis of 'TWR' referrals, yields variable results with regards to correlation between referral criteria and a diagnosis of CRC. Existing research suggests that PR bleeding [13], a change in bowel habits [13], and iron deficient anaemia [12] as having a correlation. In our study however, results failed to show statistical significance when comparing a diagnosis of CRC/HGD and benign/non-CRC malignancy, against individual criteria within the guidelines. When 74.1% of patients diagnosed with CRC/HGD and 60.9% with a benign condition or non-CRC malignancy, are referred based on the same clinical indication (iron deficiency anaemia and/or change in bowel habit, age > 60 years), there is little doubt that current symptomatic criteria lack specificity, and are common to a number of colorectal pathologies.
Although valuable information has been gained from this study, its major limitation is its relatively small sample size and a single centre study. This limits our ability generalise results as to the true effectiveness of updated NICE guidelines; a problem that could be overcome with a multicentre study, from various regions around the UK. The accuracy of patient data, specifically diagnoses, depends on the thoroughness of the documenting clinician; while referrals represent only a snapshot of a patient history and depend on both patient and GPs for accurate reporting. These problems are however, not unique to this study and do not invalidate our findings.
Guideline specificity and compliance remain major concerns and diminish the efficacy of the 'TWR' System. Regardless, the merits of the 'TWR' pathway are unquestionable. Continued research is therefore required to identify CRC specific symptomology and to determine why compliance is limited; so that guidelines compliance can be improved. Further work must also focus on ensuring patients are appropriately identified when displaying high-risk symptomology. These efforts will reduce the number diagnosed through other pathways and improve diagnostic yields. Efforts to increase public awareness as to the risks associated with CRC must continue; to increase personal agency, improve screening uptake, promote timely use of GP services and to increase adherence to risk reducing behaviours. Combined, these efforts should maximize the effectiveness of the 'TWR' pathway, inevitably providing the best opportunity to improve CRC survival rates.
Conclusion
Our study suggests the effectiveness of newly published NICE referral guidelines for CRC, in identifying patients with high-risk symptomology and in need of fast-tracked investigation. Inconsistent use of the guidelines, over-referral of guideline non-complaint and under-referral of guideline complaint patients, reduces the effectiveness of the system. Effort should be made to maximise the compliance with NICE 'TWR' guidelines to ensure that both patients and the NHS benefits from the referral guidelines and the 'TWR' pathway.
Acknowledgement
None.
Conflict of Interest
The authors declare that they have no competing interests.
References
- (2012) Bowel cancer statistics - Cancer Research UK.
- Jones R, Crosland A, Tait C (1993) How can doctors diagnose colorectal cancer earlier? BMJ 307: 503.
- (2012) Statistics and outlook of bowel cancer - Cancer Research UK.
- Sikora K (1999) Cancer survival in Britain is poorer than that of her comparable European neighbours. BMJ 319: 461-462.
- (1997) The New NHS Modern. Dependable. The Department of Health, London.
- (2000) The NHS cancer plan. Department of Health, London.
- Flashman K, O'Leary DP, Senapati A, et al. (2004) The department of health's "two week standard" for bowel cancer: Is it working? Gut 53: 387-391.
- National Institute for Health and Care Excellence (2015) Suspected cancer: Recognition and referral. London.
- Thorne K, Hutchings HA, Elwyn G (2009) The Two-Week Rule for NHS gastrointestinal cancer referrals: A systematic review of diagnostic effectives. The Open Colorectal Cancer Journal 2: 27-33.
- Thorne K, Hutchings HA, Elwyn G (2006) The effects of the Two-Week Rule on NHS colorectal cancer diagnostic services: A systematic literature review. BMC Health Serv Res 6: 43.
- Debnath D, Dielehner N, Gunning KA (2002) Guidelines, compliance, and effectiveness: A 12 months' audit in an acute district general healthcare trust on the two week rule for suspected colorectal cancer. Postgrad Med J 78: 748-51.
- Majumdar SR, Fletcher RH, Evans AT (1999) How does colorectal cancer present? Symptoms, duration, and clues to location. Am J Gastroenterol 94: 3039-3045.
- Padwick RT, Bajwa AA, Shaw A, et al. (2013) The Two-Week Referral System for colorectal cancer--not fit for purpose. Int J Colorectal Dis 28: 1531-1534.
- Rai S, Kelly MJ (2007) Prioritization of colorectal referrals: A review of the 2-week wait referral system. Colorectal dis 9: 195-202.
- Barwick TW, Scott SB, Ambrose NS (2004) The two week referral for colorectal cancer: A retrospective analysis. Colorectal dis 6: 85-91.
- Chohan DP, Goodwin K, Wilkinson S, et al. (2005) How has the 'two-week wait' rule affected the presentation of colorectal cancer? Colorectal dis 7: 450-453.
- Dua RS, Brown VS, Loukogeorgakis SP, et al. (2009) The two-week rule in colorectal cancer. Can it deliver its promise? Int J Surg 7: 521-525.
- Eccersley AJ, Wilson EM, Makris A, et al. (2003) Referral guidelines for colorectal cancer-do they work? Ann R Coll Surg Engl 85: 107-110.
- Pullyblank AM, SM, Cook TA (2003) Failure to recognise high-risk symptoms of colorectal cancer in standard referral letters leads to a delay in initiation of treatment. Colorectal dis.
- Vogelstein B, Fearon ER, Hamilton SR, et al. (1988) Genetic alterations during colorectal-tumor development. N Engl J Med 319: 525-532.
- Shussman NW, Wexner SD (2014) Colorectal polyps and polyposis syndromes. Gastroenterol Rep 2: 1-15.
- Walsh S, Bruce C, Bennington S, et al. (2002) The fourteen-day rule and colorectal cancer. Ann R Coll Surg Engl 84: 386-388.
- Harinath G, Somasekar K, Haray PN (2002) The effectiveness of new criteria for colorectal fast track clinics. Colorectal Dis 4: 115-117.
- Jones R, Rubin G, Hungin P (2001) Is the two week rule for cancer referrals working? BMJ 322: 1555-1556.
- Smith RA, Oshin O, McCallum J, et al. (2007) Outcomes in 2748 patients referred to a colorectal two-week rule clinic. Colorectal Dis 9: 340-343.
- Towler B, Irwig L, Glasziou P, et al. (1998) A systematic review of the effects of screening for colorectal cancer using the faecal occult blood test, hemoccult. BMJ 317: 559-565.
- Cabana MD, Rand CS, Powe NR, et al. (1999) Why don't physicians follow clinical practice guidelines? A framework for improvement. Jama 282: 1458-1465.
- Van den Berg MJ, de Bakker DH, Spreeuwenberg P, et al. (2009) Labour intensity of guidelines may have a greater effect on adherence than GPs' workload. BMC family practice 10: 74.
- John SK, Jones OM, Horseman N, et al. (2007) Inter general practice variability in use of referral guidelines for colorectal cancer. Colorectal Dis 9: 731-735.
Corresponding Author
Dr. Khurram Shahzad Khan, Department of General Surgery, University Hospital Hairmyres, East Kilbride, G75 8RG, Scotland, UK, Tel: 00-44-7533-537292.
Copyright
© 2021 Khan KS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.