Internalized Stigma and Quality of Life of People with Mental Illness at Dilla University Referral Hospital, South Ethiopia., 2017: A Cross Sectional Study
Abstract
Introduction
Mental illness is an important determinant of quality of life of individuals. There are different factors associated with mental illness that can potentially be a reason for lower quality of life among people with mental illness. However, only few studies are available on assessment of quality of life of people with mental illness and its determinants in Ethiopia. So the aim of this study is to assess level of quality of life and its determinants among people with mental illness at Psychiatric outpatient clinic at Dilla University Referral Hospital (DURH), South Ethiopia from June 1-October 30/ 2017.
Methods
Quantitative Facility based cross-sectional study design was employed. The data were collected by using an interviewer administered questionnaire on a total of 317 psychiatric outpatients. Quality of life was measured using quality of life assessment tool Short Form, Version -2 (SF-36 Study participants were drawn using consecutive sampling method. Data analysis was done by using SPSS version -20. Multiple linear regressions were used to test the association between factors & quality of life, and P-value of < 0.05 was considered as statistically significant.
Results
In this study, half of the studied participants had lower quality of life. Internalized stigma (Std.β = -0.041), Being female (Std.β = -0.18), lower educational status (Std.β = -2.54), lack of family support (Std.β = -0.09), lack of social support (Std.β = -1.3) and presence of side effect of psychotropic drugs (Std.β = -0.18) were factors independently associated with lower Quality of Life (QoL) of respondents.
Conclusion and recommendation
The results of this study revealed that, more than half of studied participants are suffering from lower quality of life. This also intern result in improved quality of life among people with mental illness which could be done at clinic by clinician counselors and clinical psychologists by health education, counseling and psycho education.
Keywords
Determinants, Quality of life, Mental illness, Psychiatric, Outpatients, Dilla, University, Hospital
Abbreviation
BP: Bodily Pain; DALY: Disability Adjusted Life Years; GHP: General Health Perception; ISMH: Internalized Stigma of Mental Illness; JUTH: Jimma University Teaching Hospital; MH: Mental Health; PF: Physical Functioning; PWMI: People with Mental Illness; QoL: Quality of Life; RIEP: Role Impairment due to Emotional Problem; RIP: Role Impairment due to Physical Problem; SF: Societal Functioning; SF-36: Short Form tool for measuring of QoL; V: Vitality; WHO: World Health Organization; WHOQOL: World Health Organization Quality of life
Introduction
Mental illness is a behavioral or psychological syndrome or pattern that occurs in an individual that reflects an underlying psychobiological dysfunction and the consequences of which are clinically significant distresses or disability. It must not be merely an expectable response to common stressors and losses or a culturally sanctioned response to a particular event (for example, trance states in religious rituals) & that is not primarily a result of social deviance or conflicts [1]. Worldwide around 450 million people are suffering from mental disorders and it is associated with high disease burden, disability and premature death [2]. People with mental illness (PWMI) have double problem facing them associated with their illness Quality of life (QoL) is multidimensional concept and it comprises subjective experience and objective components [3-5]. Subjective experience entails Happiness, satisfaction & well-being while objective concepts include social functioning & living condition that affect these subjective experiences. The latter involve education, employment, finance, housing, leisure activities etc. [5-9]. Quality of life of PWMI has been found to be lower compared to control groups [3,4].
Internalized Stigma is an exacerbating factor for mental illness and it affects lives of PWMI including poor help seeking behavior, social exclusion, being unemployed, economical & social ruin and premature death [2,7]. The possible factors for high prevalence of stigma are ignorance, fear of injury, derived by social conformity, internalization, cultural facts about causation of mental illness, actual (perceived) absence of treatment and preventive modalities and lack of information system to educate professional and general population [10,11]. To combat stigma and to improvement all health, some solutions are suggested by different published & unpublished researches, reports and opinions. Some of these solutions include creating awareness about mental illness to public, information, communication, expanding treatment and counseling services etc. [9,12]. Although some effort tried to reduce stigma against PWMI, stigmatization & discrimination toward PWMI, it is still persistent. A study in Jimma University Specialized Hospital (JUSH) Psychiatry clinic using the same scale also reported high prevalence of internalized stigma [5,9]. In the above study, patients who were living in rural areas were more likely to exhibit higher internalized stigma than urban residents.
Quality of life of PWMI has been found to be lower compared to control groups [11,13]. In cross-sectional assessment of quality of life of schizophrenic patients in southern Nigeria and in Finland showed studied subjects are enjoying low quality of life [11]. In studies possible factors for this undermined QoL of psychiatric patients include psychological domains including stigma, physical domains including physical illness, social relationship including support from family, independence and socio-demographic factors such as level of education.
Nowadays, the attention given for mental health is getting better than past decades. Despite the attention given for mental illness, different factors have remained a huge obstacle for successful outcomes [8,9]. In Ethiopia, there is widespread mental illness and associated deep-factors that hinders improving QoL of PWMI [12,14]. And no research has done on impact of these factors on QoL of PWMI in Ethiopia. This research will narrow this huge gap and will serve as baseline for further researches to be undertaken on the subject matter. This study will also guide in the development of strategies to improve QoL of PWMI. Last but not least, this study will identify which factors that affect the QoL of PWMI.
Methods and Materials
Study design and setting
The study was conducted from June - October 2017 at Dilla University Referral Hospital (DURH). DURH is one of oldest public hospitals in the country. Geographically, it is located in Dilla town which is located at 359 km from Addis Ababa. DURH is the one of few teaching & referral Hospitals in south of the country having 350 total beds and 650 staffs as both administrative & technical. It provides annual service for 4000 inpatient and 35,000 outpatient clients. It has also follow-up clinics for chronic illness. Psychiatry is among the 11 clinical services in the hospital serving psychiatric patients coming from Jimma area as well as patients referred from other health institutions in the southern region of the country. Over three hundred outpatients receive psychiatric care monthly. It also provides inpatient and outreach services.
A facility based cross-sectional study was carried out from June 1/2017 to October 30/2017, among Representative sample of 317 consecutive new and follow-up psychiatric services clients were included in this study. The sample size was determined by using a single population proportion statistical formula with the following assumptions:
Where: P = 25.12%; proportion of psychiatric clients who bear higher internalized stigma be 25.1% (similar previous study) [9].
d = Degree of precision (assumed to be 5%).
= Denotes the value of standard normal variable that corresponds to be 95% confidence levels (1.96.)
Then calculating the sample size
Accordingly, Minimum sample size (n) = 288. The sample size was also adjusted to compensate for non-response rate of 10%. And the final sample size was 317. Respondents were screened using the Clinical Global Impression (CGI) scale to assess their eligibility to participate in the interview for the study [15]. The scale assesses the degree of the severity of the patients' mental illness, remission of their illness and efficacy index of therapeutic and drug side effects. New patients were screened only for the severity of their illness. Using this scale and their clinical experience, the psychiatric nurses identified the eligible respondents. Patients who were severely psychotic, incoherent and too disorganized to engage in the interviews of the study were excluded. Therefore, patients included in the study were only those who were above 18-years-old and rated with at least a less severe state of mental illness, on improvement and good efficacy index by the psychiatry nurses.
Hence, total sample sizes of 317 Psychiatric clients were investigated for QoL and associated factors.
Data collection procedure
Data was collected by trained psychiatric nurses at DURH, Psychiatry clinic through interviewer-administered questionnaires and a patient chart review to identify their diagnosis and other medical information. The data collection was supervised by specialist mental health workers. Data collectors and the supervisors were trained on the contents and procedures of the data collection.
Measurement
For QoL assessment the Medical Outcomes Study Short Form 36, Version 2 (SF-36) was used. The SF-36 is widely used and has been found to have acceptable psychometric properties across different illness and age populations. The SF-36 has been utilized in monitoring health out-comes in patients with a variety of illnesses including mental illness as well as a wide range of diseases and chronic conditions. It is scale of 36 items with eight domains and in each domain certain types of questions from the 36s are included [16]. Cultural validity and reliability of items on the tool was done in Ethiopia on eight sub domains. The domains are: Physical Functioning (SF) which contains 10 items, Role Impairment due to Physical Problem (RIPP) which contains 4 items, Role Impairment due to Emotional Problems (RIEP) which contains 3 items, Bodily Pain (BP) which contains 2 items, Vitality (V) which contains 4 items, Societal Functioning (SF) which contains 3 items, Mental Health (MH) which contains 5 items, and General Health Perception (GHP) which contains 5 items. In this survey item internal consistency was high (Cranach's alpha > 0.7) and item discriminate variability was low for all items except for vitality which varied between 0.28 and 0.61 [17], higher score in each subdomain indicated higher Qol. Overall QoL score was obtained by summing the scores of the eight sub domains. Higher score showed higher QoL. The questionnaire was translated to Amharic & gediofa versions and then back to English by using different translators to ensure semantic equivalence. The data collectors were trained on how to administer the questionnaire, how to approach the participants & role plays by trainees was conducted to strengthen the skills of administration of questionnaire to the participants.
Statistical analyses
After the data collection, data was checked manually for completeness & consistency. It was entered, cleaned & rechecked for its completeness, anomalies & consistency again and stored in to Epidata and then was exported to SPSS window versions 20 for analysis. Descriptive statistics was done to summarize the dependent and independent variables. Bivariate & multiple linear regressions were done to explore the association of socio-demographic factors & other independent variables with QoL of PWMI after total scores calculated for QoL. Variables with p-value < 0.25 in bivarate analysis were selected as candidates for multivariate analysis. Finally variables with a p-value < 0.05 were considered as having significant association with the dependent variable.
Ethical approval
Officially written approval letter was obtained from Research and Dissemination Office of Dilla University prior to the study. Written permission was obtained from DURH clinical director and the Psychiatry clinic. Written informed consent was also obtained from each study participant. The interviewers were informed each respondents about all details of the research, what expected of them and the way information handled i.e. no information shared with third parties (except the investigator). The clients were also encouraged to fill freely and confidentiality of their responses was assured (as participants were asked in private setting and their name was not identified on the questionnaires).
Results
Socio-demographic characteristics of studied participants
Of the total 317 respondents 119 (56.5%) were urban residents with a mean age of 33.60 and with standard deviation of 9.59 years. The response rate was 100%. Nearly one-third (34.8%) were in the age range 25-34 year old, while 44.3% were age 35-49 year old, 21% were age above 49 years. As for sex, 69.4% of the studied participants were males. The data also reveals that, 23.6% of the participants were illiterate while 36.3% doped out from elementary school and 25.9% of studied participants were educated to college and above level. As regards to occupational status, 38.1% of the studied participants were farmers, 18.4% were unemployed, while students cover 8.4% of the studied participants. Considering marital status, 51.3% of the studied participants were married, 47.6% of the studied participants were single, and 1.1% of the studied participants were sum of all other marital status. About 56.5% of the studied participants were from urban area. As for ethnicity, the majority of the studied participants (44.6%) were gedio followed by 24% sidamo and guragie participants. Concerning religion of the studied participants, majority of them (45.6% and 27.6%) were protestant and Orthodox Christians respectively (Table 1).
Concerning family support of study participants, three-quarters (81.1%) received support from the family but the rest did not get any support. With regard to social support, the majority of the studied participants (51.1%) do not have any social support (Table 2).
Concerning drug side effect, majority of the respondents did not report it comprising 51.1%. With regard to drug side effect 27.9%, 13.7%, 18.5%, 1.8%, 1.2% and 0.9% of the studied participants reported weight gain, tremor, sexual problem, tremor, sedation and gait abnormality respectively (Table 3).
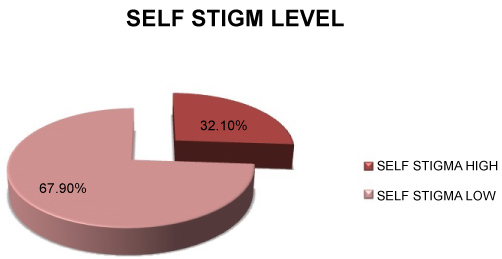
Magnitude of internalized stigma
From the studied participants, 32.1% have high level of self-stigma based on total stigma score. The mean for the overall self-stigma score is 2.26 and with standard deviation of 0.39 (Figure 1).
Relationship between self-stigma and QoL
As stigma increases by one unit in studied participants of PWMI, quality of life of them decreases by 4.1% significantly. (β1 = -0.041, 95% C.I: -0.065, 0.012). In this study self-stigma and QoL were inversely correlated (r = -0.076) which indicates stigma worsen QoL of people with mental illness. Stigma was entered in final model; multiple linear regression by controlling confounding factors. And, the association did reach statistical significance. Regarding correlation between QoL and stigma, the self-stigma scores were inversely correlated with QoL scores (r = -0.076) (Table 4).
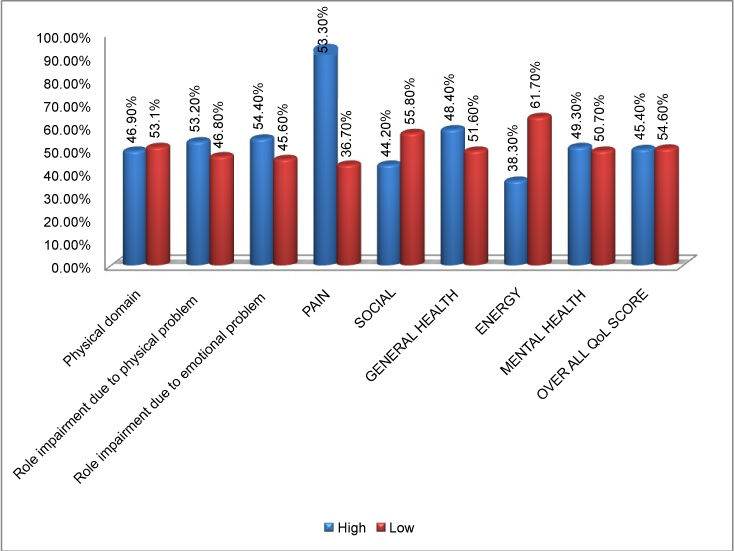
Level of quality of life of studied participants
With regard to level of quality of life, 53.1% and 46.8% of the studied participants have low quality of life in area of physical domain and role impairment of physical problem while 45.6% and 36.7% of the studied participants experienced low quality of life due to role impairment of emotional problem and pain experience, respectively. In addition, 55.8%, 61.7% and 50.7% of the studied participants were also exhibiting low quality of life in social aspect, with respect to energy, and with respect to social life. Greater than half (51.6%) of the studied participants had low quality of life related to general health. Over all, half of the studied participants 54.6% (CI (confidence interval), 41.3%-73.4%) had lower than the mean QoL score (≤ 65.5) (Figure 2).
Factors affecting quality of life of studied participants
As depicted in (Table 5), multiple linear regressions were done to identify the association of quality of life of people with mental illness and potential factors including self-stigma. As stigma increases by one unit in studied participants of PWMI, quality of life of them decreases by 4.1% significantly. (β1 = -0.041, 95% C.I: -0.065,-0.012). With regard to sex of respondents, quality of life of females was lower than their male counter parts (Std.β = -0.18, 95% C.I: -2.9,-0.12). Those who got family support were found to have better quality of life than those who did not get support (Std.β = -0.09, 95% C.I: (-5.53,-0.29)). Regarding societal support of respondents, those who get societal support had increased score of quality of life compared to those who had no societal support. (Std.β = -1.3, 95% C.I: (-2.1,-1.20). So forth, Study participants who had a better educational level were found to have a better QoL than those with lower educational level. Respondents who have completed high school had higher QoL than those who were only educated up to elementary (Std.β = -2.54 C.I: -1.33,-5.15) Participants who had side effect of medication had lower quality of life compared with those who did not have Std.β = -0.18, 95% C.I: (-2.11,-0.13) the regression model for overall quality of life explained 45% of the variability (adj.R2) (Table 5).
Discussion
The finding revealed that a high percentage of the studied participants demonstrated low level of QoL which was 54.6%. This is in line with study findings done in turkey [18] with the overall mean QoL score of patients was 61.5 (range 24.6-89.6, SD 17.4) suggesting that patients' QoL was impaired. Considering factors affecting QoL of studied participants, the following arguments are entertained: In this study self stigma, sex, educational level, lack of support system and medication side effect were factors associated with lower QoL were associated with lower QoL of respondents. Considering factors affecting QoL of studied participants, the following arguments are entertained: As stigma increases by one unit in studied participants of PWMI, quality of life of them decreases by 4.1% significantly. (β1 = -0.041, 95% C.I: -0.065,-0.012). This result was congruent with findings of study done in Cairo [19], who reported that stigma is negatively associated with quality of life. Additionally the impairment in social and leisure functioning associated with concerns about stigma has implications for the health and well-being of persons diagnosed as having bipolar illness. Being female was significantly related to lower quality of life than their counter parts. This finding is consistent with the findings of the studies done in Jordan [20] which elaborates that women's psychosocial background in their limited access to resources, their limited status in culturally countries like Ethiopia, low role and option in mental health service seeking behavior and compliance with treatments. This consensus paper justified that co morbidity increases in prevalence and severity and will lead to high level of disability in female than males. This study finding is also consistent with findings of study in Egypt [13] which rectified that women are more likely to seek help from and disclose mental health problems in their primary health facilities where mental health professionals are not staffs while men are likely to seek mental health specialist in referral clinics which intern facilitate to take targeted medication that is one of positive predictors of QoL of PWMI in this study. In addition to this sounded justification from [21] stressed that identified gender as a factor that may affect feeling of stigma which intern explained that females were more stigmatized than males for identical behavior. And using this justification as a base and since stigma and quality of life are inversely correlated in my particular finding, this finding is also soundly acceptable. The finding of this study is also supported by study done in WHO conference [2,22] which conclude that being male is associated with higher Quality of Life with respect to physical component, social component, and mental components comparing to females. This study is in line with the study done in India [17] which showed that males had better QoL than females.
Regarding educational status of studied participants, respondents who are higher educated are living higher QoL than those who educated lower are experiencing higher quality of life. This finding is in line with a previous similar study [23] which concluded emotional and mental health of PWMI is enhanced in higher educational achievement than the lower education by justification that education can develop mental capacity and skills to cope up with mental illness vulnerability and to lower complication of mental illness which inturn reduce disability and enhance quality of life.
The finding of this study is consistent with study done by World Health Organization (WHO) [2] which stressed on the fact that education in PWMI will improve social and cognitive abilities, boosts self-stem and widened social networks and intern all these support people ability to live independently and to have a decent income. This may be due to that educated mental ill individuals acquire different skills and abilities which can refresh from their mental discomfort and to get relief from symptoms and ultimately without education and employment, PWMI face poverty, alienation, increased risk of addiction, isolation, deteriorating mental and physical health of QoL. This finding is also supported by the study done in Luxemburg [14] which stated that QoL of young PWMI which comprised emotional well-being (happiness, confidence), psychological wellbeing (autonomy, sense of mystery), social wellbeing (interpersonal relationship). And many other domains are integral outcomes from lifelong learning which overall aim is that key competencies contribute to one's personal fulfillment, social inclusion, active citizenship and employability. Considering family and social support of studied participants, the finding of this study reveal that individuals who get support from family and from the society in general are enjoying better quality of life than those studied participants who do not get support. This finding is consistent with findings from Switzerland, Geneva [10] which reported that people with mental illness who are receiving care from their family by reducing expressed emotion and who are getting friendly approach from outside society in line with their family experienced better quality of life and resulted to better general health and dramatic improvement for their societal functioning.
Regarding drug side effect of medication, those who are free from medication side effects were experiencing better quality of life compared to those who had medication side effect. the finding of this study is consistent with study finding in Egypt and Nigeria [11,19] which showed that poor therapeutic conditions such as bad experience on initial mental health contact and not taking medications lead to long term problems in which clients suffer from emotional, social and mental domains of QoL and this in turn lead to restrained by family members and make patients home bounded impaired their independency to enjoy other domains of quality of life which ultimately result to lower overall quality of life. Other variables such as marital status, ethnicity, residence, occupation, income, duration of treatment and with who studied participant live with had no statically significant relationship with QoL of studied participants in this study. This finding is supported by previous findings done in Egypt, Turkey, India [13,17,18]. This consistent finding indicated that socio demographic characteristics of studied participants has less impact on QoL than other factors like support system and psycho social factors.
Conclusion and Recommendations
Conclusion
Over half of persons with mental illness on treatment suffer from low quality of life. Factors associated with low quality of life among PWMI need to be addressed by mental health intervention programs so as to improve the life of PWMI.
Recommendations
As negative predictors, internalized stigma is associated with low quality of life of PWMI. So, great efforts have to be invested on stigma reduction strategy factors to divert low quality of life among PWMI to better one. A Lot to be done by mental health intervention programs at both clinical and community settings of DURH which includes expand training program which could empower people with mental illness toward stigma so as to improve the life of PWMI, Planning and implementation of public health awareness programs to raise the orientation toward the nature of psychiatric disorders, this programs should reach all social classes and cultures in: Schools, universities social clubs, religious institutions and mass media through outreached health education program, Psychiatric institutions should do more roles not only in medical management of patients but also in promotion of their social life. So forth, Increase patient's awareness to certain issues could protect against more feelings of stigma, Mass media should play role in de-stigmatization of psychiatric patients and psychiatric illness as well. Ministry of health should do much on mental illness awareness creation, stigma prevention and expansion of mental health services to the ground level. As addition, provide psycho education to family members on nature of mental illness and awareness creation giving support and avoiding alienated acts and expressed emotion to improve quality of life PWMI. For further study home visit based study will reduce this limitation. And at most it is better to study on self-stem as predictors of stigma and QoL in future study to reduce limitation of this study so as to improve the life of PWMI.
Ethics Approval and Consent of Participants
Officially written approval letter was obtained from Research and Dissemination Office of Dilla University prior to the study. Written permission was obtained from DURH clinical director and the Psychiatry clinic. Written informed consent was also obtained from each study participant. The interviewers were informed each respondents about all details of the research, what expected of them and the way information handled i.e. no information shared with third parties (except the investigator). The clients were also encouraged to fill freely and confidentiality of their responses was assured (as participants were asked in private setting and their name was not identified on the questionnaires).
Consent for Publication
Not applicable.
Availability of Data and Materials
The data that support the findings of this study has a sort of identifier of individual participants and researcher reserved to send it.
Competing of Interest
The author declares he has no conflict of interest.
Funding
Not applicable.
Authors Contribution
AEA: Involved idea conception for proposal development, writing up of proposal; YBW: Contributed in supervising of data collection and data quality assurance; EH: Involved in writing up of results and discussion and in writing manuscript. All authors contributed equally. All authors read and approved the final manuscript.
Acknowledgment
The authors would like to thank selected towns' administration office for their cooperation and support, Data collectors for their responsible data collection and all study participants who share their experiences.
References
- Diagnostic and statistical manual of mental disorders (DSM- V) (2016) American Psychiatric Association 7: 83-94.
- World Health Organization (WHO) (2016) Measuring quality of life Switzerland. Critical Appraisal, Geneva, Switzerland 17: 103.
- Batinic B, Lemonis E (2014) Effects of internalized stigma of mental disorder on quality of life and selfesteem in panic disorder patients. Journal of Clinical Research and Bioethics 5.
- Karakas SA, Okanlı A, Yılmaz E (2016) The effect of internalized stigma on the self esteem in patients with schizophrenia. Arch Psychiatr Nurs 30: 648-652.
- Girma E, Möller-Leimkühler AM, Dehning S, et al. (2014) Self-stigma among caregivers of people with mental illness: Toward caregivers' empowerment. J Multidiscip Healthc 7: 37-43.
- Livingston JD, Boyd JE (2010) Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Soc Sci Med 71: 2150-2161.
- Reta Y, Tesfaye M, Girma E, et al. (2016) Public stigma against people with mental illness in Jimma Town, Southwest Ethiopia. PLoS ONE 11: e0163103.
- Girma E, Tesfaye M, Froeschl G, et al. (2013) Facility based cross-sectional study of self stigma among people with mental illness: Towards patient empowerment approach. International Journal of Mental Health Systems 7: 21.
- Girma E, Tesfaye M, Froeschl G, et al. (2012) Public stigma against people with mental illness in the Gilgel Gibe Field Research Center (GGFRC) in Southwest Ethiopia. PLoS ONE 8: e82116.
- World Health Organization (WHO) (2015) Mental health and stigma: A call for action by world health ministries, Geneva, Switzerland 7: 103.
- Aloba O, Fatoye O, Mapayi B, Akinsulore S (2013) A review of quality of life studies in Nigerian patients with psychiatric disorders. Afr J Psychiatry (Johannesbg) 16: 333-337.
- Ritsher JB, Otilingam PG, Grajales M (2003) Internalized stigma of mental illness: Psychometric properties of a new measure. Psychiatry Research 121: 31-49.
- Amin M, Abdel Aziz H, El Lawindy M (2014) Schizophrenic patients families psycho-education: Outcomes on patient quality of life and disease relapse rate. Egyptian Journal of Psychiatry 1: 59-74.
- Wodegiworgise T, Simme K (2015) National mental health strategy. Federal ministry of Health, Ethiopia 1: 33-54.
- Guy W (1976) ECDEU assessment manual for psychopharmacology. U.S Department of Health, Education, and Welfare, Rockville, Maryland.
- Kebede D, Alem A, Negash A, et al. (2014) Health related quality of life (SF-36) validation survey in Butajira. Soc Psychiatry Psychitr Epidemiol 36: 299-303.
- Deepak KM, Sarka A, Sengar KS, et al. (2014) Insight & its relationship with stigma in psychiatric patients. India: Department of Psychology 11: 10.
- Anneli P (2014) Improving quality of life of patients with schizophrenia. Uiversity of Turku 5: 133-154.
- Omnia Mohamed A, Enayat Abd El W, Zeinab Abd El H, et al. (2015) The effect of stigma on quality of life among people with mental illnesses. International Journal of Science and Research 33: 58.
- Al-Krenawi A, Graham JR, Kandah J (2000) Gendered utilization differences of mental health services in jordan. Community Ment Health J 36: 501-511.
- Dan S, Mihae M (2015) Gender disparities in mental health. Journal of Affective Disorder 86: 205-213.
- Madhukar H, Andrew A, David W, et al. (2014) Health-related quality of life in depression. Annals of Clinical Psychiatry 22: 43-55.
- Alisa L, Michael KPO, Debbie MC, et al. (2006) Impact of health literacy on HRQoL among adults with addiction. J Gen Intern Med 21: 818-822.
Corresponding Author
Alem Eskeziya Ayenalem, Department of Psychiatry, College of Health Science and School of Medicine, Dilla University, Dilla, Ethiopia.
Copyright
© 2019 Ayenalem AE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.