Ultrasound Guided Pneumatic Reduction of Intussusceptions: A Clinical Experience from Baghdad
Abstract
Background: Intussusceptions is an important cause of small bowel obstruction in children. Non-operative reduction (NOR) is the preferable method of treatment to start with as long as there are no contraindications to its use & where facilities are available. Pneumatic reduction has become a popular therapeutic method for intussusceptions instead of surgery in many centers.
Objective: To evaluate the success rate of ultrasound guided pneumatic reduction of intussusceptions and verifying the factors affecting its efficacy as initial experience in Baghdad.
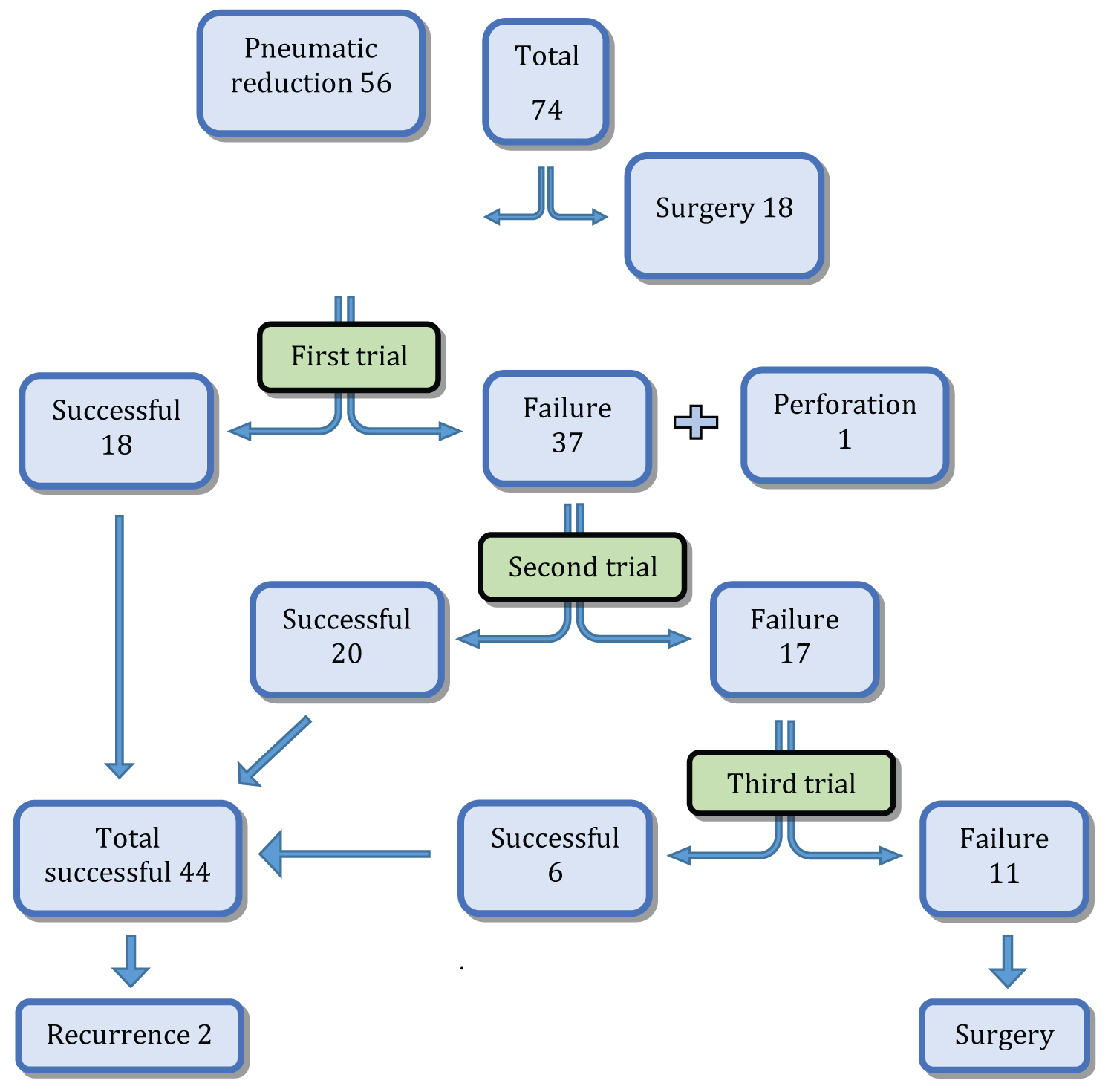
Patients and methods: A prospective study of 56 eligible patients with confirmed intussusceptions managed over the period of eighteen months from March 2016 to September 2017 in Baghdad. The procedure was performed under ultrasound guidance after adequate resuscitation. Those patients with unsuccessful first attempt of pneumatic reduction were subjected to second & third attempts before surgical intervention performed.
Results: A total 39 male and 17 female were found suitable for pneumatic reduction under ultrasound guide. Successful reduction by air insufflations was achieved in 44 patients (78.5%), whereas the procedure was failed in the remaining 12 patients (21.4%). There were only two out of 44 patients (4.5%) with successful reduction developed early recurrence of intussusceptions. One patient (2.27%) developed intestinal perforation.
Conclusion: Pneumatic reduction of intussusceptions under ultrasound guidance is a quick, safe, simple, with a high success rate, radiation-sparing effect. Success rate is highly affected by the duration of symptoms & location of mass. The procedure is not devoid of recurrence risk & possibility of developing tension pneumoperitoneum.
Keywords
Intussusceptions, Pneumatic reduction, Ultrasonography
Introduction
Intussusceptions is the most frequent cause of bowel obstruction in infants and toddlers and probably the second most common cause of acute abdominal pain after constipation in these age groups [1,2]. The treatment of intussusceptions is an emergency, by either non-operative or operative method. Delay in treatment will lead to ischemia and necrosis of the intestine, bowel perforation, peritonitis, shock, and possibly death [3].
Non-operative reduction (NOR) is the preferable method of treatment to start with as long as there are no contraindications to its use & where facilities are available [3]. The next logical step after failure of non-operative approach is surgery. Indeed, the choice between the two methods (operative and non-operative) depends on the general condition of the patient, the duration of illness and the availability of skilled radiological service [4]. The currently used techniques for non-operative reduction of intussusceptions include pneumatic or hydrostatic pressure enemas under fluoroscopic or sonographic guidance [1] with the advantages of decreased morbidity, cost, and length of hospitalization [2].
Objective
In this study, we aim to evaluate the success rate of ultrasound guided pneumatic reduction of intussusceptions and verifying the factors affecting its efficacy as initial experience in Baghdad.
Patients and Method
A prospective study included 56 infants and children with idiopathic, uncomplicated intussusceptions (as inclusion criteria) treated by non-operative reduction (NOR) over the period of eighteen months from March 2016 to September 2017 in Baghdad. While patients with ages more than 2 years, delayed presentation (> 72 hours), cases of recurrent intussusceptions, & features of peritonitis or shock were excluded from this study (n = 18 patients). A special data form had been used including variables of age, sex, residence, history of admission to other hospital, clinical presentation, coexisting illness, investigations, type of management in addition to postoperative notes and complications. All patients with suspicion of intussusceptions were admitted to the surgical ward, clinical evaluation and assessment of the general condition were made by a full history and physical examination, resuscitation was done by insertion of intravenous line, nasogastric tube and starting fluid therapy and antibiotics. The patients were sent for plain abdominal X-ray, ultrasound of the abdomen, and laboratory investigations (complete blood count, blood urea, serum creatinine, and serum electrolytes).
After confirming the diagnosis by ultrasound examination, the definitive treatment started within few hours when the general condition of patient became stable, a cross- matched blood was prepared for all patients regardless of the method used in the treatment, and written informed consent was taken from each patient’s parent or guardian for participation in the study. The study was approved by the local hospital ethical committee. Statistical analysis of the data was done using SPSS-version18 software (IMB Corporation). Using percentage, mean, & ANOVA (Analysis of variance). A p value less than 0.05 was considered statistical significant.
Technique
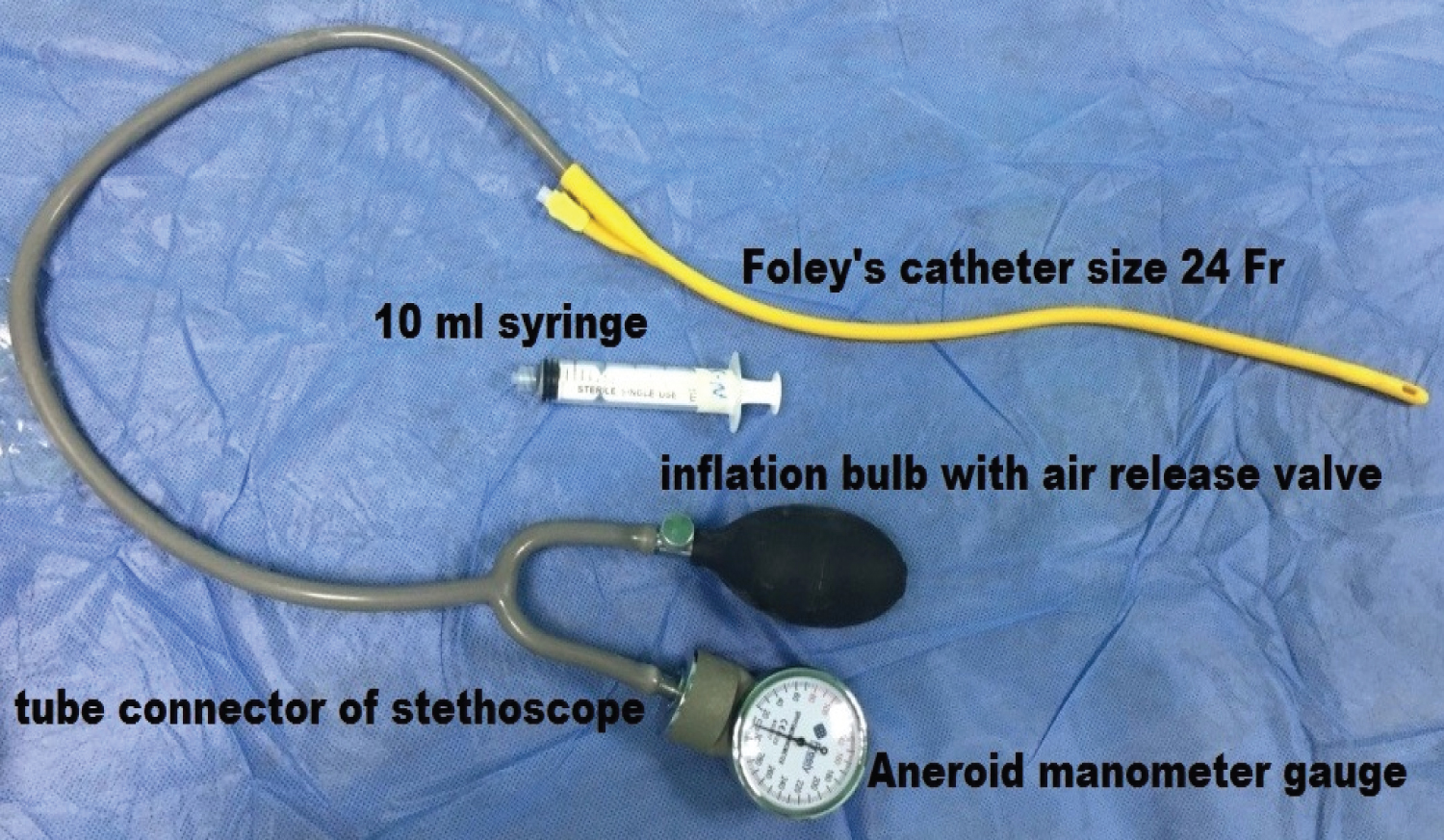
Air insufflations were used for NOR in 56 patients through the modified air insufflations device (Figure 1). Surgery was performed in patients with exclusion criteria or those patients with failed attempts of pneumatic reduction.
The procedure was done under ultrasound guidance without sedation, anesthesia & muscle relaxant by inserting a well lubricated large size Foley's catheter (22 Fr, or 24Fr) into the rectum and inflating the balloon with 25-30 ml normal saline, then pulled down to be kept as low as possible. With the patient in a supine position, the buttocks were taped together with the help of a nurse. The other end of the catheter was connected to the air insufflations device. The air was introduced into the colon by gradual squeezing the inflation bulb with maintaining pressure between 60 and 120 mmHg (The maximum air pressure for younger infants and in the first attempt of reduction was 100 mmHg while pressure of up to 120 mmHg was used for older infants and in the second & third attempts of reduction).
There is fluctuation in the measured pressure with straining & crying of the child & in between the insufflations. The reduction process is tracked by ultrasound scanning probe throughout the procedure. The increased intra-colonic pressure will reduces intussuscepted gradually through the ileo-caecal junction. The procedure is terminated once there are satisfactory clinical and ultrasound features of complete reduction of intussusceptions. Although successful reduction of intussusceptions was confirmed by ultrasound, further confirmation by plain abdominal X-ray in some patients was achieved, which showed delineation of the whole colon and terminal ileum with gases. After that, the patient was returned back to the surgical ward and kept there for about 24-48 hours for observation and detection of any complication.
Those patients with failed first trial of reduction, another one to two trials of reduction were performed within the next 2-4 hours. High resistance to air insufflations & Persistence of the mass by ultrasound were the signs of unsuccessful reduction & indications of operative intervention.
Patients with successful reduction were sent for ultrasound examination in the next day to exclude any residual pathology or recurrence & discharged home based on the following criteria:
1. Disappearance of all symptoms and signs of intussusceptions.
2. Starting oral feeding without vomiting.
3. Passing normal bowel motion.
4. Disappearance of the mass by ultrasound.
Results
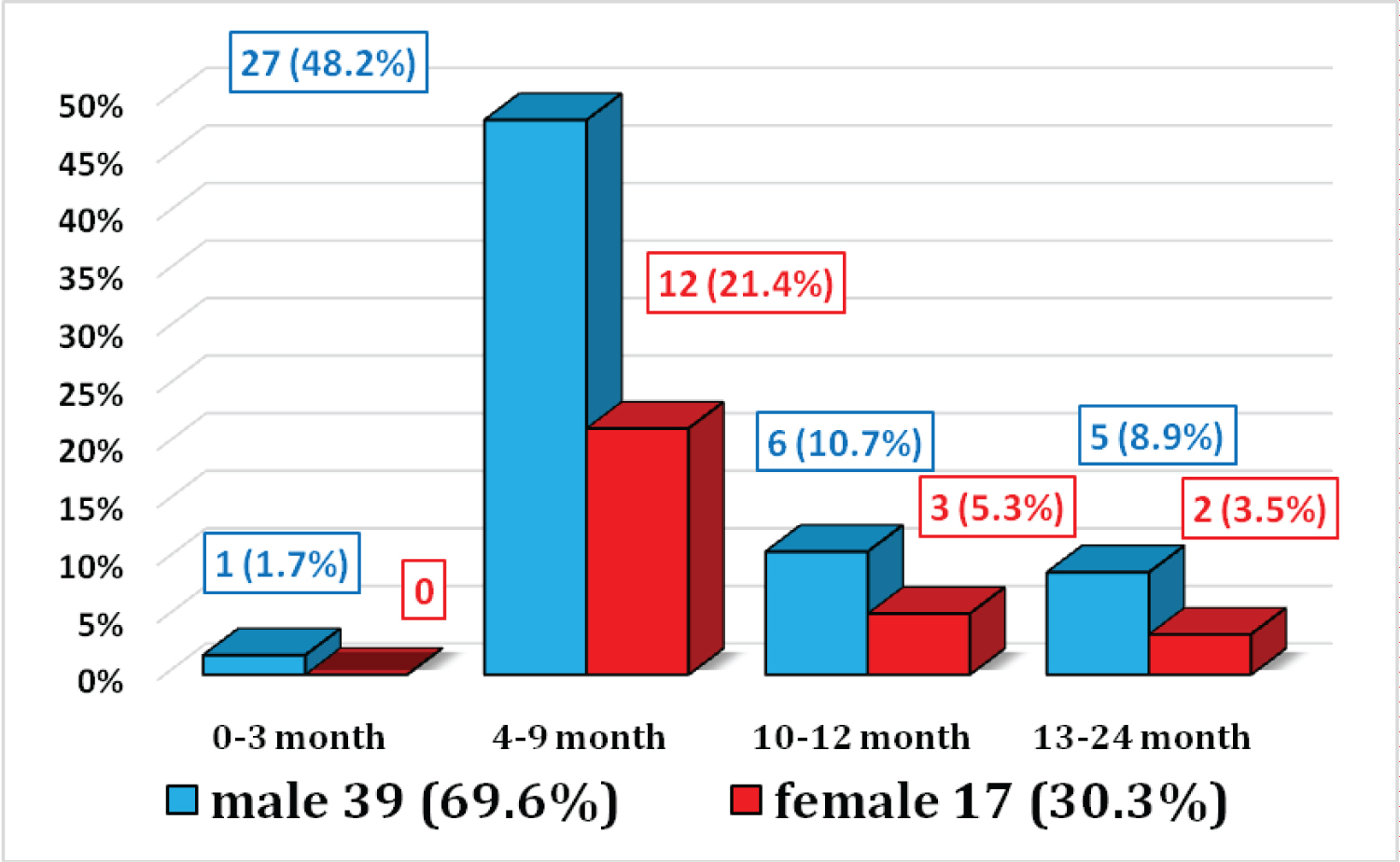
Among total 74 patients with intussusceptions managed during the study period, non-operative reduction by mean of air insufflations was attempted in 56 (75.6%) patients as initial line of treatment. The majority of patients in this study (49 patients, 87.5%) were under the age of one year, the group of 4-9 months age being the commonest age group (39 patients, 69.6%) (Figure 2). The youngest patient in this study was male aged 3 months while the oldest one was a male aged 22 months. Mean age was 7.77 month. There were 39 males (69.6%) and 17 females (30.3%), the male to female ratio in this study was 2.2:1 (Figure 2).
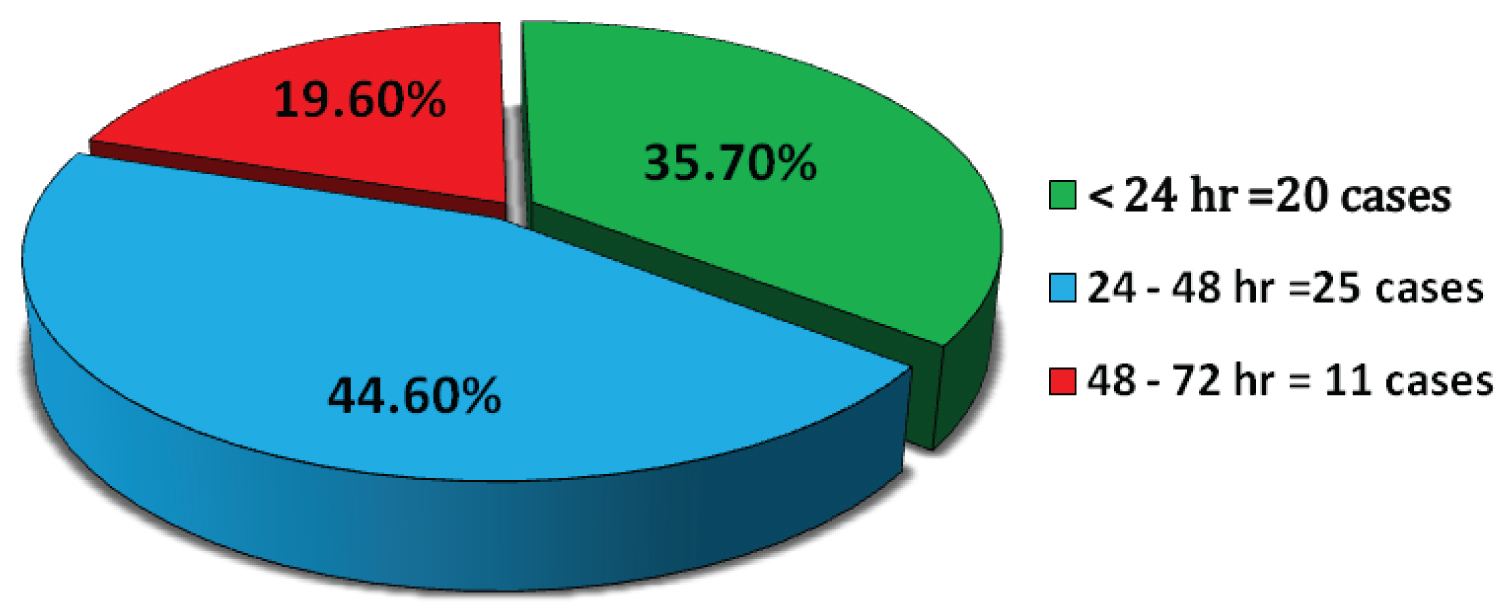
Figure 3 shows the duration of symptoms prior to presentation to hospital. Only 20 patients (35.7%) presented early within the first 24 hours of onset of symptoms. Screaming attacks (colicky abdominal pain) & repeated vomiting were the most common presenting symptoms 96% & 89% respectively. The family gave history of bleeding per rectum in 46 out of 56 patients (82%). On physical examination, abdominal tenderness was obvious in 42 patients (75%). Palpable abdominal mass was felt in only 30 patients (53.57%) while the characteristic red currant jelly stool was noticed following PR exam in 45 patients (80.3%). Abdominal distention & palpable mass per rectum or prolapsed through anus were found in the advanced cases (more than 48-hour duration of symptoms). The classic clinical trial of abdominal pain, abdominal mass and rectal bleeding occurred only in 31 patients (55.3%) (See Table 1).
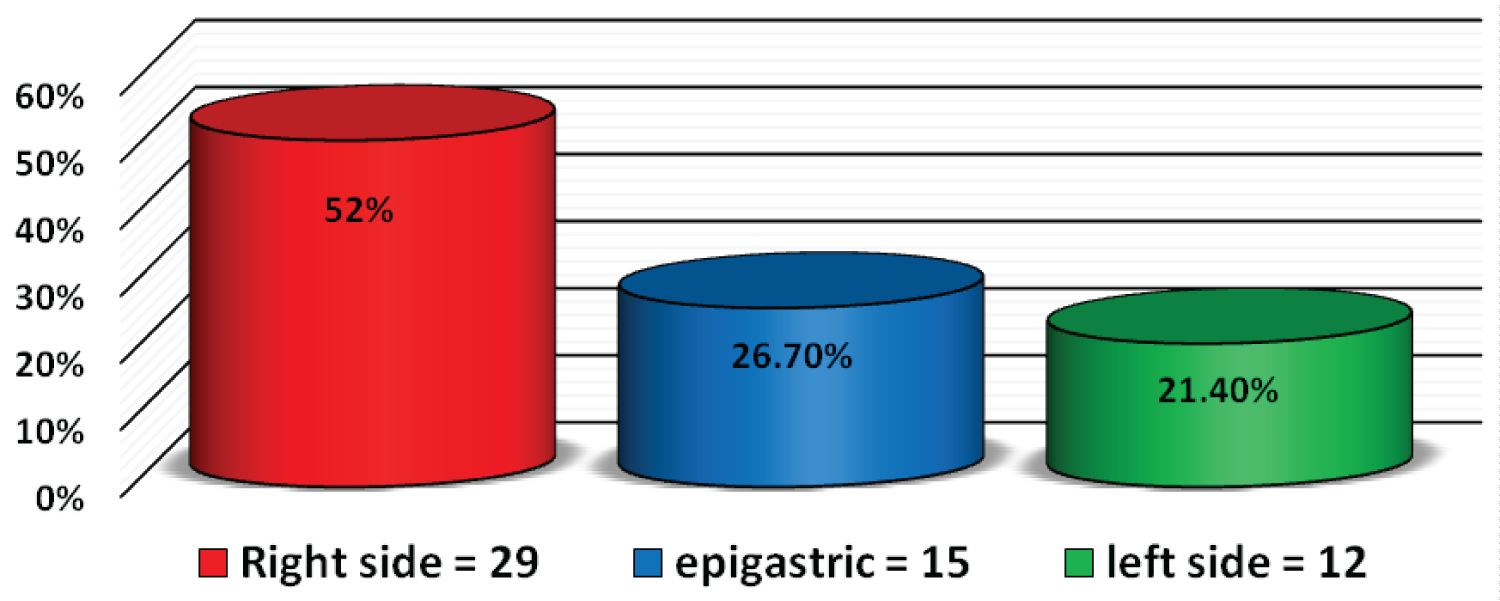
On clinical & ultrasound examination, the most common site of the mass was in the upper right side of the abdomen in 29 patients (51.7%). Central abdominal and epigastria mass was noticed in 15 patients (26.7%). While palpable mass in the left side of abdomen was noticed in 12 patients (21.4%), five of them having a mass palpable per rectal examination (8.9%) & in one case the mass was prolapsed through the anus (Figure 4).
Successful reduction by air insufflations was achieved in 44 patients (78.5%), whereas the procedure was failed in the remaining 12 patients (21.4%). On surgical exploration, the bowel at area of intussusceptions was ischemic in five patients, so underwent resection and end-to-end anastomosis. Difficult manual reduction with some serosal tear was recorded in three patients. Pathological lead points was noticed as a cause of intussusceptions in the remaining four cases (three cases of Meckel's diverticulum & one case of intestinal lymphoma), & again end with resection & anastomosis.
Regarding relation of duration of symptoms to the successful pneumatic reduction, it was an important predictive factor of successful reduction with highly significant p = 0.001. The procedure was highly successful in patients with early presentation (95%) & least successful in patients with delayed presentation (45.4%) (Table 2).
Regarding relation of duration of symptoms to the number of attempts of successful reduction, 70% of those patients who presented early (less than 24 hours) having successful reduction from the first attempt, while 52% of those patients who presented after 24 hours of symptoms required 2 attempts of pneumatic reduction to achieve complete reduction. Only 18% of patients with delayed presentation have complete reduction after three attempts. The total rate of successful reduction from the first attempt was recorded in 18 out of 56 patients (32.1%), & it was varied considerably according to the duration of symptoms with statistical P = 0.000. The total rate of successful reduction from two attempts was recorded in 20 patients (35.7%) with no statistical variation (P = 0.111) among groups of duration of symptoms. While only six patients (10.7%) achieved successful reduction with third attempt (P = 0.013) (Table 2).
Regarding relation of successful reduction to the location of mass as identified by examination and ultrasound finding at the time of presentation; the procedure achieved high rate of successful reduction in the right sided & epigastria masses (86.2%, 86.6% respectively) & least rate in the left sided masses or when the mass was palpable per rectum. Again the rate of successful reduction is varied considerably according to mass location (P = 0.004) as shown in Table 3.
Regarding relation of trials of reduction to the location of mass, we found that a good number of patients (48.3%) with right sided mass have successful reduction with single attempt only, while 50% of those patients with left sided mass or mass that is palpable through rectal exam have failure reduction even after all three attempts of air insufflations (Table 3).
There were only two out of 44 patients with successful reduction (4.5%) developed recurrence of intussusceptions within less than 48 hours of successful reduction confirmed by ultrasound examination (Figure 5). Repeated air insufflations reduction was done under ultrasound guide & was successful in both cases with single attempt. One patient developed intestinal perforation (2.27%) He was 5-months-old male infant with more than 48-hour duration of symptoms.
The perforation occurred during the first attempt of reduction at pressure of 90 mmHg when we noticed sudden drop in the pressure & clinical deterioration. It was promptly recognized by the radiologist & the patient proceeded immediately to theatre where surgery done for him & we discovered a small perforation in an ischemic area of ascending colon with no peritoneal soiling. Right hemicolectomy & ileo-colic anastomosis was done & the patient then got full recovery. No mortality rate encountered during the study period.
Discussion
Non-operative reduction (NOR) of intussusceptions is the first-line of treatment if there are no contraindications to its use, it include pneumatic or hydrostatic reduction under fluoroscopic or ultrasound guidance [1]. In contrast to operative reduction, NOR have decreased morbidity, cost, length of hospitalization, and devoid of surgical complications [2]. Pneumatic reduction was first described in 1897 [5] & then gained popularity in the late 1980s when ultrasound guidance has been added to the armamentarium. Since then, many institutions have adopted this procedure because it is quick, safe and decreases the exposure time to radiation [4].
In this study, we found that the majority of patients (69.6%) were in the age group of 4-9 months & this is consistent with what mentioned in the textbooks & literatures [1,2]. The male to female ratio was 2.2:1, which is similar to the ratio reported by literatures [6,7]. Most of the patients were well-nourished and healthy supporting Hirschsprung’s classic statement: "I never saw a malnourished child with intussusceptions [1].
Only 20 of our patients (35.7%) presented early within the first 24 hours of onset of symptoms while study of Dahab, et al. [8] in Cairo & Alhasani [9] in Basra reported that the majority of their patients (60%, 54.3% respectively) presented early within the first 24 hours of onset of their symptoms. The large number of patients in this study with more than 24 hours duration of symptoms may be attributed to delayed diagnosis in some patients, misdiagnosis (as gastroenteritis, otitis media.....etc.) or due to late referral by the local general practitioner. All of the presenting features in this study were comparable with corresponding features of other studies (as shown in Table 4) [8,10-14].
We did not use anesthesia or sedation during pneumatic reduction because it could mask the signs of shock during the procedure [15]. We also did not use muscle relaxant because smooth muscle tension during the reduction procedure protects against bowel perforation Furthermore the increased intra-abdominal pressure caused by crying and straining help in rapid reduction [16-18].
The small bowel which is invaginated into the caecum will be pushed back to its place by air pressure and relieving the obstruction. The ultrasound criteria for successful reduction after deflation of air included disappearance of the intussuscepted, single concentric ring representing the swollen terminal ileum instead of the multiple concentric rings of intussusceptions, a severely swollen terminal ileum, and the abrupt transition of bowel wall thickness between the swollen terminal ileum and the proximal normal ileum on longitudinal axis scanning [15].
Successful reduction by air insufflations was achieved in 44 patients (78.5%). Recent studies in nearby countries reported rates of successful reduction range from 74% to 94.6% as shown in Table 5.
We found that as the duration of symptoms increases, the rate of successful reduction (especially from first attempt) will decrease. The success rate of pneumatic reduction was 95% when the patients presented early within the first 24 hours of symptoms & decreased to 45% when the patients presented lately after 48 hours of stating the symptoms. This has a statistical significant P value (0.001). The same thing was reported by other literatures [8-19]. The long duration of symptoms will give time to development of edema and vascular changes that make the intussusceptions so tight & decreases the likelihood of pneumatic reduction. We noticed that the duration of symptoms also correlate with the number of trials needed to achieve successful reduction, 70% of those patients who presented early achieved successful reduction with first attempt compared to 9% of those with delayed presentation, (statistical significant p value 0.000) (Table 2).
The location of mass can predict the chance of successful reduction & the number of trial needed to achieve it. We found that the more distally located mass of intussusceptions have less rate of successful reduction with statistical significant P = 0.004. This is similar to that reported by S. Kritsaneepaiboon, et al. [19].
In general, about one third of all patients under the study have successful first attempt of reduction, which is much lower than that reported by the others like Salih, et al. [10] (85%), Arsalan, et al. [11] (91%), Kritsaneepaiboon, et al. [19] (76%), Hosni, et al. [20] (58.3%), and Omar Bin Hassan, et al. [21] 79%. This low success rate of first attempt reduction in our study may be due to the low pressure applied initially and the less experience with this modality of treatment in our department. In the second attempt, we increased the pressure to 120 mmHg so we had a higher success rate of 35.7% which is higher than that reported by the Dahab, et al. (12%) [8]. The low pressure used initially in the first attempt can explain this. In the third attempts, the success rate in our study was 10.7%, which was similar to that reported by the others. For unsuccessful reduction with first attempt, several studies have shown improved reduction rates using a second attempt after waiting between 30 minutes to 24 hours after the initial attempt [22]. In some instances, this is done in the operating room prior to laparoscopy or in conjunction with laparoscopic reduction [23].
Several risk factors have been found in literature to decrease the success rate of pneumatic reduction [1] such as younger ages (less than three months), longer duration of symptoms (more than two days) & the type of intussusceptions; Enema reduction has a higher failure rate in patients with ileoileocolic intussusceptions [1]. Ultrasonography findings of trapped fluid within the intussusceptions and the intussuscepted reaching the rectum are other conditions associated with less successful enema reduction [24].
In our study, immediate recurrence of intussusceptions was recorded in (4.5%). The recurrence neither rate following initial NOR is reported to be as high as 10% to 15% of patients. But, it is much lower following surgical reduction (1% to 3%) [25-28]. Indeed, adhesions created by the operative manual reduction, & ileocolic resection are factors responsible for this lower recurrence rate after surgical reduction [29]. Recurrence neither following NOR may be due to incomplete reduction (but that is less likely under fluoroscopy or ultrasound guided reduction) or due to the presence of a pathological leading point. Niramis, et al. reported about a 3-fold increase in the incidence of lead points in children with recurrent intussusception. We reported no cases of pathological lead points in the two patients with recurrence & they treated successfully with a further pneumatic reduction. Current concepts suggest that the initial management of recurrent intussusceptions should be non-operative treatment, even if they recur after previous operative reduction [29,30].
Bowel perforation occurred only in one patient who presented lately after 2 days of onset of symptoms. Although repeated or delayed second attempt of reduction is a risk factor for bowel perforation [31], the late presentation appears to be more risky according to our data. Dahab, et al. [8] reported one case of perforation on the third attempt of reduction after 10 hours from the first attempt, while in our study all of the second & third trials were performed within the next 2-4 hours from the initial attempt as recommended by others [31]. No mortality has been encountered during the procedure.
The ultrasound guidance has added the advantages of avoiding radiation exposure, providing more information about monitoring of reduction process, visualizing all components of intussusceptions including the post-reduction edematous ileo-caecal region. However, ultrasonography has some limitations; it is operator-dependent so that an expert radiologist or adequate training is required. Furthermore, it has low specificity in detecting pneumoperitoneum [32] & need ultrasound machines with high-quality images to detect intra-peritoneal free air [33].
In summary, ultrasound guided pneumatic reduction of intussusceptions is feasible in all children less than 2 years unless contraindicated. The procedure can be done without sedation or general anesthesia safely & has high success rate, radiation-sparing effect, minimal risk of bowel perforation with less peritoneal contamination, moreover accurate pressure measurement is possible. The success rate is highly affected by the duration of symptoms & location of mass, so that early diagnosis & referral to pediatric surgical centers will improve the results. Second & third attempts of reduction are encouraged after unsuccessful initial attempt. The procedure is not devoid of recurrence risk & possibility of developing tension pneumoperitoneum.
Acknowledgement
None.
References
- Columbani PM, Scholz S (2012) Intussusceptions. In: Coran AG, Adzick NS, Thomas Rummel TM et al. Pediatric surgery. Volume 2, Seventh edition. Philadelphia, 1093-1110.
- Maki CA, Fallat ME (2014) Intussusceptions. In: Holcomb GW, Murphy JP, Ostlie DJ, et al. Pediatric surgery. (6th> edn), Elsevier Saunders, 531-538.
- Hesse AAJ, Abantanga FA, Lakhoo K (2011) Intussusceptions. In: Ameh EA, Bickler SW, Lakhoo K, et al. Pediatric surgery: Comprehensive text for Africa. 2: 404-411.
- Guo JZ, Ma XY, Zhou QH, et al. (1986) Results of air pressure enema reduction of intussusception: 6,396 cases in 13 years. J Pediatr Surg 21: 1201-1203.
- Holt LE (1897) The Diseases of Infancy and Childhood: For the Use of Students and Practioners of Medicine. New York: Appleton.
- Korkmaz M, Yazgan H, Budan K, et al. (2012) Pneumatic reduction in the treatment of childhood intussusception cases. Gaziantep Medical Journal 18: 56-60.
- Al-Meflh W, AbuQuraa A, Khaswneh G, et al. (2016) Pneumatic Reduction of Pediatric Intussusceptions: Experience at Queen Rania Al-Abdullah Hospital for Children. J Royal Med Serv 23: 13-9.
- Dahab MM, AbouZeid AA, Mohammad SA, et al. (2012) The second trial pneumatic reduction for idiopathic intussusceptions: Therapeutic effect and hazards. Ann Pediatr Surg 8: 77-79.
- Alhasni AA (2016) Assessment of intraoperative manual reduction of intussusceptions in children. Bas J Surg 22: 69-76.
- Saleh G, El-saket MD, Eassa O, et al. (2005) Pneumatic reduction versus surgical reduction in cases of neonatal Intussusception. El-minia Med Bull 16: 39-48.
- Arslan S, Turan C, Doganay S, et al. (2014) The effectiveness of pneumoreduction for intussusceptions. Ann Ital Chir 85: 459-463.
- Al-Shahwani AR (2001) The use of Air Insufflations in managing intussusceptions. J Fac Med Baghdad 43: 173-178.
- Zain AZ (2012) Management of intussusceptions in children. Iraqi J Comm Med 1: 40-43.
- Gata HK, Ejrish AA (2016) The role of ultrasound in diagnosis of intussusceptions in children in Baghdad 2012-2013. MJB 13: 85-94.
- Yoon CH, Kim HJ, Goo HW, et al. (2001) Intussusceptions in children: Us-guided pneumatic reduction - initial experience. Radiology 218: 85-88.
- Rosenfeld K, McHugh K (1999) Survey of intussusceptions reduction in england, scotland and wales: how and why we could do better. Clin Radial 54: 452-458.
- Zheng JY, Frush DP, Guo JZ, et al. (1994) Review of pneumatic reduction of intussusceptions: Evolution no revolution. J Pediatr Surg 29: 93-97.
- Zulfiqar MA, Noryati M, Hamzaini AH, et al. (2006) Pneumatic reduction of intussusceptions using equipment readily available in the hospital. Med J Malaysia 61: 199-203.
- Kritsaneepaiboon S, Sankhathat S, Kanngurn S, et al. (2011) Pneumatic reduction of intussusceptions: Factors affecting outcome in thailand. Asian Biomedicine 5: 235-241.
- Ahmed HM, Ahmed O, Ahmed RK, et al. (2015) Adding a custom made pressure release valve during air enema for intussusceptions: A new technique. Afr J Paediatr Surg 12: 232-235.
- Hasan O, Farees SN, Ibrahim M, et al. (2015) Ultrasound guided pneumatic reduction of intussusceptions in children - a case series. Int J Rec Sci Research 6: 4204-4207.
- Daneman A, Navarro O (2003) Intussusceptions. Part 1: A review of diagnostic approaches. Pediatr Radial 33: 79-85.
- Kao C, Tseng SH, Chen Y, et al. (2011) Laparoscopic reduction of intussusceptions in children by a single surgeon in comparison with open surgery. Minim Invasive Ther Allied Techno 20: 141-145.
- Yamout SZ, Caty MG, Glick PhL, et al. (2009) Complications of surgery of the stomach, Duodenum, and Small Intestine. In: Complication in pediatric surgery informa healthcare. New York, 257-285.
- Champoux AN, Del Beccaro MA, Nazar-Stewart V, et al. (1994) Recurrent intussusceptions risks and features. Arch Pediatr Adolesc Med 148: 474-478.
- Stringer DA, Ein SH (1990) Pneumatic reduction: Advantages, risks and indications. Pediatr Radiol 20: 475- 477.
- Renwick AA, Beasley SW, Phelan E, et al. (1992) Intussusceptions: recurrence followings (oxygen) enema reduction. Pediatr Surg Int 7: 361-363.
- Daneman A, Alton DJ, Lobo E, et al. (1998) Patterns of recurrence of intussusceptions in children: A 17-year review. Pediatric Radiology 16: 913-919.
- Niramis R, Watanatittan S, Kruatrachue A, et al. (2010) Management of recurrent intussusceptions: nonoperative or operative reduction?. J Pediatr Surg 30: 2175-2180.
- Kaiser AD, Applegate KE, Ladd HP, et al. (2007) Current success in the treatment of intussusceptions in children. Surgery 142: 469-77.
- Sandler AD, Ein SH, Connolly B, et al. (1999) Unsuccessful air-enema reduction of intussusception: Is a second attempt worthwhile? Pediatr Surg Int 1: 214-216.
- Chen SC, Wang HP, Chen WJ et al. (2020) Selective use of ultrasonography for the detection of pneumoperitoneum. Acad Emerg Med 1: 643-645.
- Hefny AF, Abu-Zidan FM (2011) Sonographic diagnosis of intraperitoneal free air. J Emerg Trauma Shock 4: 511-513.
Corresponding Author
Loay Saleh Salman, Pediatric Surgeon, FICSP, Abn Al-Baladi hospital, Baghdad, Iraq
Copyright
© 2022 Salman LS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.