Post-Axial Hexadactyly in Neonates and Infants Less than 3 Months Old: Surgical Management Transferred to the Outpatient Clinic in the Covid-19 Period
Abstract
Background: The current Covid-19 corona viruses pandemic has had a considerable impact on the functioning of health care facilities, so the reorganisation of interventions was a real challenge for surgeons who risk facing the establishment of large waiting lists. We present successful outpatient surgical excision procedures for a case series of post-axial type B hexadactyly in covid 19 infants.
Methods: From 1 January 2020 and 31 December 2021, a retrospective review of patients treated for post-axial type B hexadactyly was performed. The excision technique in the outpatient department was documented.
Results: Over a 24-month period, a total of twenty-eight neonates and infants were treated in the outpatient clinic for post-axial hexadactyly type B; half of the patients had bilateral post-axial hexadactyly. The mean age of the child at the time of excision was 35 days, with extremes of 7 days-3 months. Forty-two excision procedures were performed. No post-procedure complications were noted.
Conclusions: Surgical excision of post-axial type B hexadactyly at the outpatient clinic using topical anaesthesia, non-adrenalized xylocaine during tete-a-tete is a safe and effective technique. This technique is a cost-effective approach to this condition, avoiding postponement of procedures until later without the need for general anaesthesia. It gives excellent results, improves safety without sacrificing quality of care.
Keywords
Post-Axial Hexadactyly Type B, Newborn/Infant, Local Anaesthesia, Covid-19, Outpatient
Introduction
Post-axial hexadactyly type B also known as ulnar Polydactyly is the most common type of Polydactyly of the hand. It is characterised by the presence of a supernumerary digit attached by soft tissue in a pedunculated manner to the fifth finger [1]. Treatment options for post-axial hexadactyly type B include observation, suture ligation, clip ligation or surgical excision. Suture ligation can be performed in the nursery, at home or in the doctor's office. The expected result of this procedure is to produce necrosis of the rudimentary finger, followed by self-amputation of the additional gangrenous tissue. Proponents of this treatment cite its low cost and simplicity [2,3].
In recent years, however, the practice of suture ligation has been questioned by several authors who cite the associated complications and the frequency of incomplete amputations or painful neuronal [1,4]. Initial surgical excision using an elliptical incision with high ligation and retraction of the accessory digital nerve has been encouraged to avoid potential complications and improve outcomes. However, many authors believe that the surgical procedure is reserved for the block [1,5].
We report a case series of outpatient surgical excision of post-axial type B hexadactyly in response to the selective use of OR rooms in the Covid-19 period in infants under 3 months of age.
Methodology
Between 1 January 2020 and 31 December 2021, a retrospective chart review of patients with a weight of 3000g or more undergoing outpatient excision of post-axial type B hexadactyly was performed. Pre-axial Polydactyly of the hand and Polydactyly of the foot were not included in the study. The type of anaesthesia and procedures were described. The length of stay and parental satisfaction were studied. We calculated the average time from admission to discharge from the operating room for the same type of surgery in patients operated on during the period 2019.
Pre-operatively
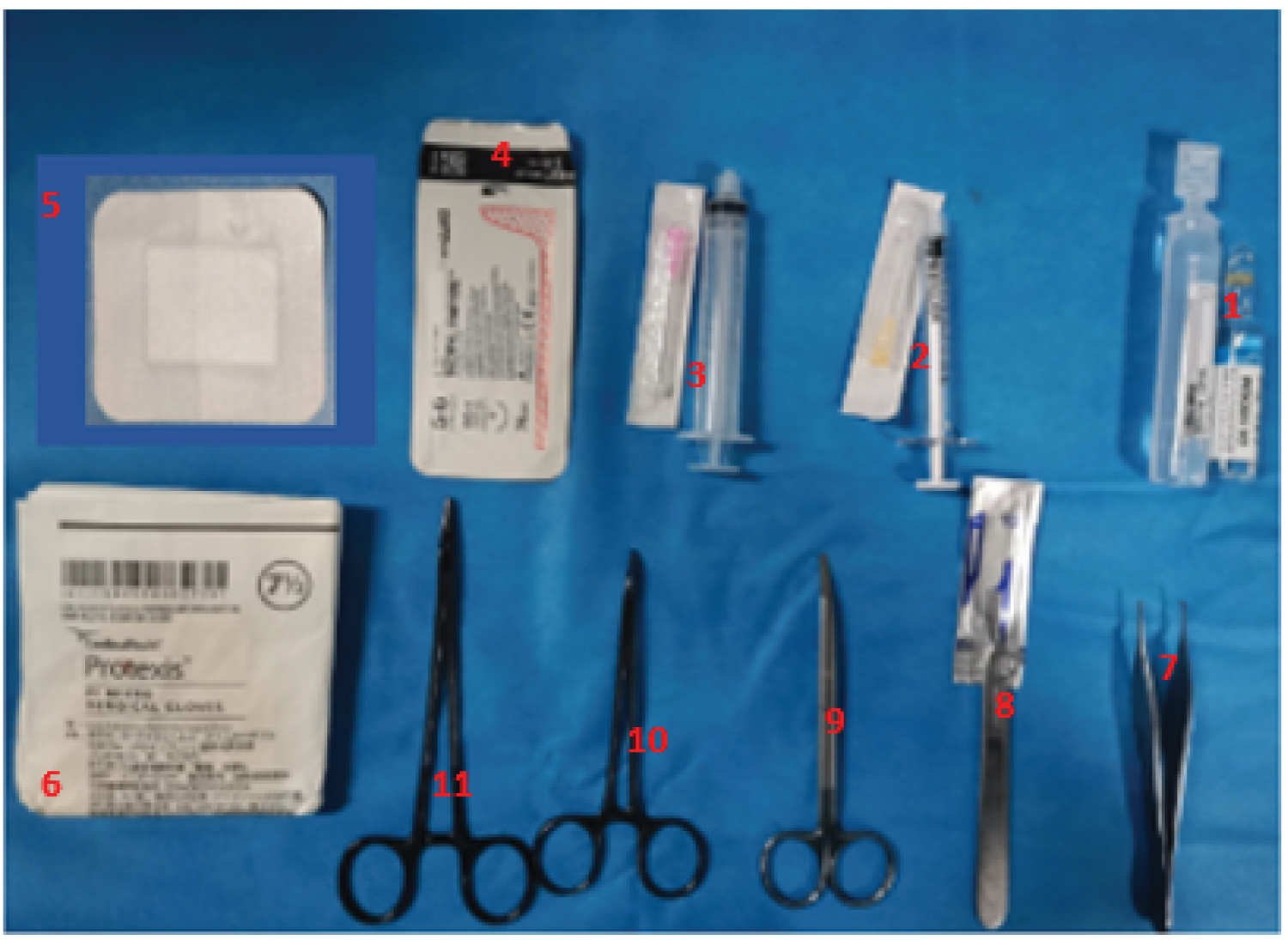
Once assessed by the surgeon either in the maternity ward, nursery, or paediatric ward. The procedure is explained to the parents and their consent is obtained. The excision is scheduled between two patients at the outpatient clinic. EMLA® topical anaesthetic (Lidocaine 2.5% and prilocaine 2.5%) was given to the parents to be applied by the mother at least 1 hour before the procedure. time before the appointment at the surgery consultation. Materials are served and prepared in advance. The supplies needed for the procedure are shown in (Figure 1) bipolar forceps set to affect 1 and power [6]. A mixture of 8 ml of non-adrenalized xylocaine and 2 ml of sodium bicarbonate to reduce the inflammatory effect of the xylocaine on the tissues.
Intra-Operatively
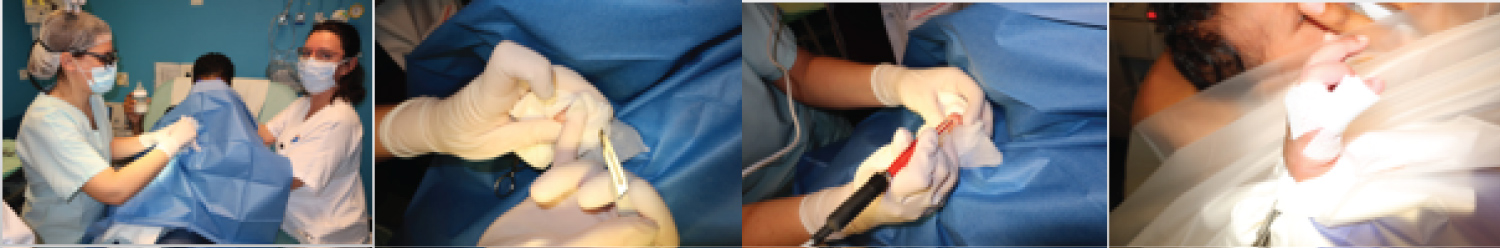
The mother is placed with her baby on the treatment table. The patient's hand and forearm are prepared with swabs and sheets are placed to achieve sterility of the field. The mother is allowed to breastfeed or bottle feed the baby before the injection of the anaesthetic begins. Injection doses of lidocaine varied from 0.3 to 1 ml depending on the thickness of the base of the polydactyl finger and the number (single or bilateral). The surgeon grasps the supernumerary digit in gentle extension and injects the anaesthetic at its base before making an incision at its base. The neurovascular pedicle is cauterised. The skin is closed with 5-0 quick vicryl. Dressing (Figure 2).
Post-Operative Management
The infants were sent home once the surgical centre's guidelines had been met. Instructions for surgical site management and contact information were provided to the family.
Results
Over a 24-month period a total of 28 patients were treated for post-axial hexadactyly type B in the outpatient department. There were 18 girls and 10 boys. The mean age was 25 days with extremes of 2 days and 3 months. Half of the patients had bilateral post-axial type B hexadactyly. The total number of accessory fingers excised was 42. All children seen for post-axial type B hexadactyly during the study period were scheduled and operated on.
All procedures were performed between two consultations twenty minutes apart or at the beginning of a consultation without discomfort at the next one. No post-operative complications were noted. The excised fingers were disposed of as medical waste. Total satisfaction was reported by all parents.
Discussion
The current corona virus pandemic (COVID-19), linked to the SARS-CoV virus, has precipitated an unprecedented global crisis. In France since 24 January 2020, and following the passage of the disease to stage 3, in order to face the gravity of the health situation, a strict confinement was decided by the national public authorities from Tuesday 17 March 2020 at noon [6]. Five days before, the government activated the white plan and asked health professionals to immediately deprogram any non-urgent surgical activity. The regularisation of delayed interventions will be a real challenge for surgeons but also for our health system in general, which risks to be confronted with the establishment of important waiting lists. In our case we decided to transfer the surgical management of post-axial hexadactyly type B initially excised in the block under local anaesthesia to the care room of the paediatric surgery outpatient department; this allowed us to anticipate as soon as possible these major changes in order to adapt and offer the best management for our patients in COVID-19 secure channels.
EMLA® contains two amides: lidocaine 2.5%, prilocaine 2.5%, and an oil and water emulsion forming a cream, each gram of which contains 25 mg of lidocaine and 25 mg of prilocaine. The combination of local anaesthetic and sodium bicarbonate in a percutaneous procedure can reduce the pain of subcutaneous injection of the local anaesthetic if given alone [7]. After discussing the therapeutic procedure with the parents and obtaining their agreement, an EMLA cream was given to all parents for application at 1 hour's notice to attend the consultation. This was highly beneficial in minimising the traumatic effect of the needle during the injection of xylocaine. Ahmad, et al., [7] and Kim, et al., [8] performed excisions of post-axial type B hexadactyly in neonates using a mixture of local anaesthetic cream and xylocaine injection. The authors mention that the only pain experienced by the child is during the injection of the local anaesthetic. In our context we chose this time to put the child to the breast or bottle just before the injection in order to direct his attention to his feeding.
When treating patients with post-axial type B Polydactyly, the goals include complete removal of excess tissue, prevention of neuronal, minimisation of aesthetically unpleasant residual tissue and avoidance of common adverse effects (infection, bleeding, and complications from anaesthesia). When suture ligation is used as a treatment technique, the accessory nerves of the extra finger occasionally protrude through the skin to produce a painful neuronal [8]. In a cohort of infants treated with this approach, 40% had a residual tender bump at the ligation site on postoperative examination [2]. Initial surgical excision using an elliptical incision with high ligation and retraction of the accessory digital nerve has been encouraged to avoid potential complications and improve outcomes [7,9].
In our series, we chose the surgical option for all patients with post-axial type B hexadactyly at the consultation. Excision in the consultation ward of post-axial type B hexadactyly in infants meets the objectives of surgical excision and significantly reduces costs without any decrease in the quality or safety of the procedure. The use of general anaesthesia in young children is not without risk. Multiple studies link exposure to general anaesthesia in patients under 3 years of age [10,11]. Although no formal analysis of costs and exact duration has been done, the reader can imagine the savings of avoiding general anaesthesia and the cost of transporting patients to the pharmacy and operating rooms. For an excision in the outpatient department the time spent on the procedure itself is about 10 to 15 minutes. You can see how this is a huge under-use of a surgeon's time to perform an excision in the operating room. In our series, all parents reported satisfaction with the management procedure. No postoperative complications were recorded.
Conclusion
Surgical excision of post-axial type B hexadactyly at the outpatient clinic using topical anaesthesia, non-adrenalized xylocaine during suckling is a safe and effective procedure. This technique is a cost-effective approach to this condition, avoiding postponement of surgery until later. It gives excellent results and improves safety without sacrificing quality of care.
Disclosure
All authors declare no conflict of interest.
Acknowledgement
All the surgeons would like to thank the nurses of the consultation, in particular Fanny Elicaste, for their adaptation and help during this period.
References
- Ing C, DiMaggio C, Whitehouse A, et al. (2012) Long-term differences in language and cognitive function after childhood exposure to anesthesia. Pediatrics 130: 476-485.
- Friedan IJ, Chang MW, Lee I, et al. (1995) Suture ligation of supernumerary digits and ’tags’: An outmoded practice? Arch Pediatr Adolesc Med 149: 1284.
- Watson BT, Hennrikus WL (1997) Postaxial type-B polydactyl. Prevalence treatment J Bone Joint Surg Am 79: 65-68.
- Abzug JM, Scott H (2013) Treatment of Postaxial Polydactyl Type B, The Journal of Hand Surgery 38: 1223-1225.
- Pinar U, Anract J, Duquesne I, et al. (2020) Impact de la pandemic de COVID-19 sur l’activité chirurgical au sein des services d’urologie de l’Assistance Publique - Hôpitaux de Paris de Paris 30: 8-9 439-447.
- Soledad Cepeda M, Tzortzopoulou A, Thackrey M, et al. (2010) Adjusting the pH of lidocaine for reducing pain on injection Base de données Cochrane Syst Rev 8: 12.
- Mise à jour dans: Cochrane Database Syst Rev. 2015;5:CD006581. PMID: 21154371.
- Bjorklund KA, O’Brien M (2021) Local Anesthesia Alone for Postaxial Polydactyl Surgery in Infants. Hand 25.
- Ahmad Z, Park AJ (2014) The milk anesthesia management of neonatal accessory digits: The 6 year Coventry and Warwickshire experience. J Med Soc 28: 149-53.
- Frieden IJ, Chang MW, Lee I (1995) Suture Ligation of Supernumerary Digits and 'Tags': An Outmoded Practice? Archives of Pediatrics and Adolescent Medicine 149: 11.
- Sprung J, Flick RP, Katusic SK, et al. (2012) Attention-deficit/hyperactivity disorder after early exposure to procedures requiring general anesthesia. Mayo Clin Proc 87: 120-129.
Corresponding Author
Mamadou Madiou Barry, Doctor of Medicine, Paediatric Surgeon (CHU Dakar/Conakry), Intern in Paediatric Plastic Surgery/CHU Montpellier, France, Tel: (0033)-748635540
Copyright
© 2022 Barry MM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.