A Rare Case of Rectal Duplication Cyst presenting as a Posterior Perineal Hernia, in a Neonate
Abstract
Introduction: Rectal duplication is a rare entity and posterior perineal hernia is even so. Having both entities together poses a clinical challenge, however sticking to basic surgical principles helps in such situations.
Aims: The case is being presented here with the aim of describing a rare case scenario and its successful management. Methods: We describe here a case of rectal duplication that presented as a posterior perineal hernia in the neonatal period.
Results: A 26 days old child presented to the emergency room of a tertiary care pediatric hospital with complaints of gradually increasing swellings in bilateral gluteal regions since birth and abdominal distension with bilious vomiting for one day. The child was taken for exploratory laparotomy and excision of the cyst with covering high sigmoid loop colostomy was done. The child later developed rectal stricture that was successfully managed conservatively.
Conclusions: Pediatric surgeons will keep on facing new challenges in the form of rare anomalies or combinations. Sticking to the basic principles of surgery is the key in such situations.
Keywords
Rectal duplication, Posterior perineal Hernia, Congenital, neonatal
Introduction
Enteric duplication cysts are rare entities, the history of which dates back to the year 1884 when Reginald Fitz introduced the term "Intestinal duplication".[1] Later in 1937 Ladd and Gross re-introduced them and Gross in the year 1950 classified duplication cysts. [2,3] Later Ladd coined the term "Alimentary tract duplications" for those congenital malformations that ascend from the mesenteric side of the involved alimentary tract sharing common blood supply with bowel. Out of these rare intestinal duplication cases, Rectal duplication amounts to only approximately 4 %. [4]
The presentation of rectal duplication cyst varies with the size and consistency of the lesion. Compression of the rectum may lead to constipation, intestinal obstruction or rectal bleeding [5]. Compression of the ureters or bladder neck may present as urinary outlet obstruction or even hydroureteronephrosis [6]. Zaeim M et al reported a case of rectal duplication cyst who presented with rectal prolapsed [7]
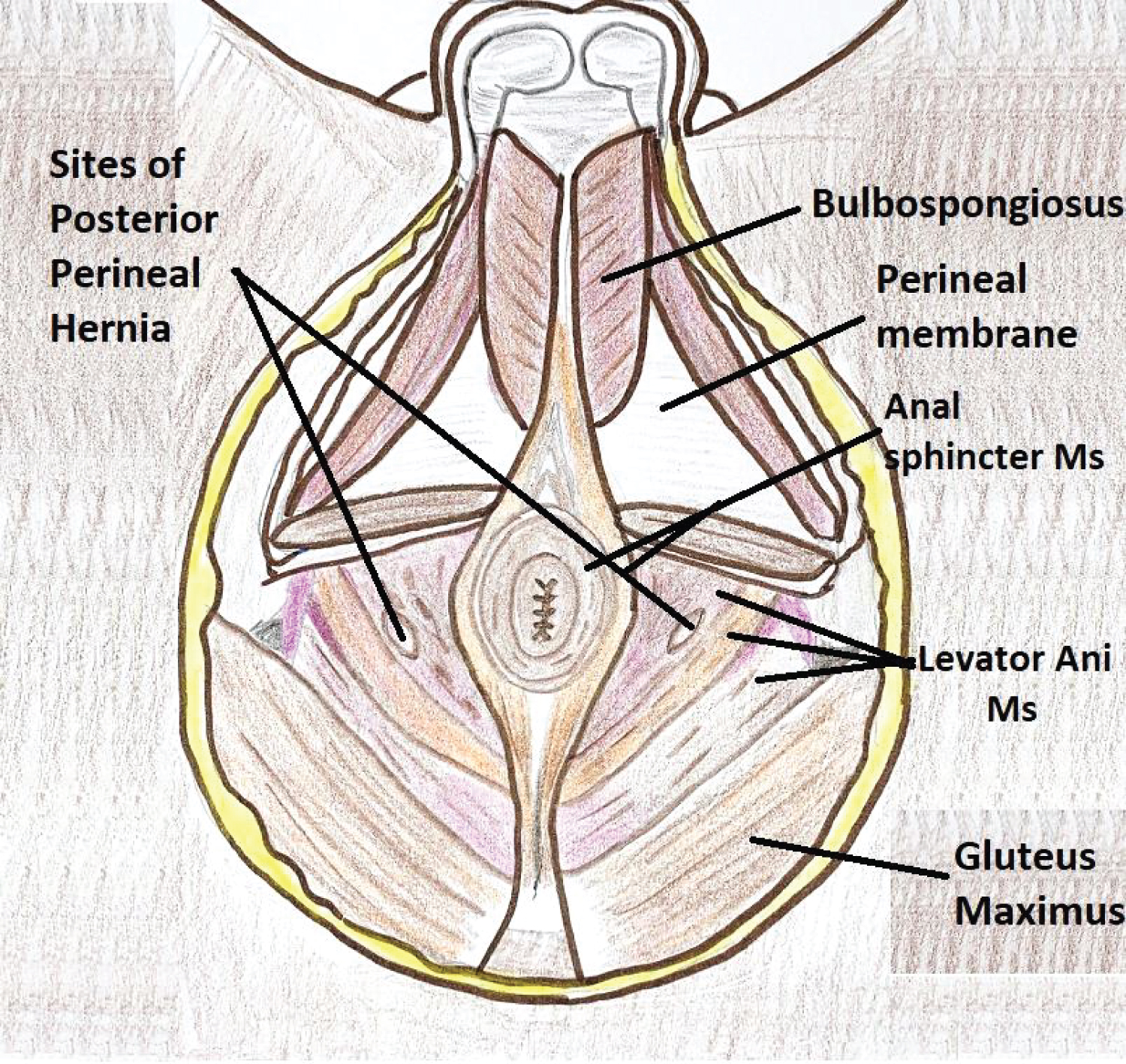
Perineal hernia (PH), defined as the protrusion of intraperitoneal or extra peritoneal contents into the perineum through a congenital or acquired defect of the pelvic diaphragm [8], is a very rare condition, more so within the pediatric population. Among the PH, an anterior and a posterior form (which is even rarer) can be delineated, based on their position relative to the transverse perineii muscle. The orifice of the posterior form is located either in the levatorani muscle itself or between the levatorani muscle and coccygeus muscle. PHsare classified into primary or secondary (Usually postoperative) [9]. Primary PH can be congenital, resulting from the developmental defect in the muscles of the pelvic floor or acquired.
Rectal duplication cyst in itself is rare and the same presenting as posterior perineal hernia makes this case a rarest of rare, which to our knowledge, has not been reported previously.
Pediatric surgeons face many rare clinical situations in their lifetime and reporting such rare case provides an insight into the unknown world. However, the case is not being presented here just to describe a rare case scenario, but also to emphasize that in the absence of a clear-cut preoperative diagnosis and treatment guidelines of rare case scenarios, it is wiser to stick to basic principles encompassing fundamental principles of surgery, anesthesia, fluid and pain management to avoid unnecessary risk and to manage such cases successfully for which no precedent is available.
In this report, we present our experience in the diagnosis and treatment of a child with a posterior perineal hernia with a rectal duplication cyst, along with a review of relevant literature, at the Super Speciality Pediatrics Hospital and Postgraduate Teaching Institute, Noida, U.P, India.
The Case
A 26 days old, male child, 3.2 kg, presented to the emergency room of a tertiary care pediatric hospital with complaints of gradually increasing swellings in bilateral gluteal regions since birth and abdominal distension with bilious vomiting for one day. The child was a product of a normal pregnancy and delivery with a birth weight of 3,000g. The bilateral gluteal swellings, which increased during crying, were discovered by the parents, after fourteen days of life.
On examination, the child was sick with clinical features of peritonitis. Perineal examination revealed a normally located, normal-sized anal opening. Boggy swellings were present on bilateral buttocks, which were soft, apparently non-tender, increased during crying and were irreducible (Figure 1). Plain X-ray abdomen revealed a large radiolucent cyst occupying the central and lower abdomen (Figure 2). An abdominal ultrasound found a hernia sac extending in bilateral buttock sand containing digestive loops.
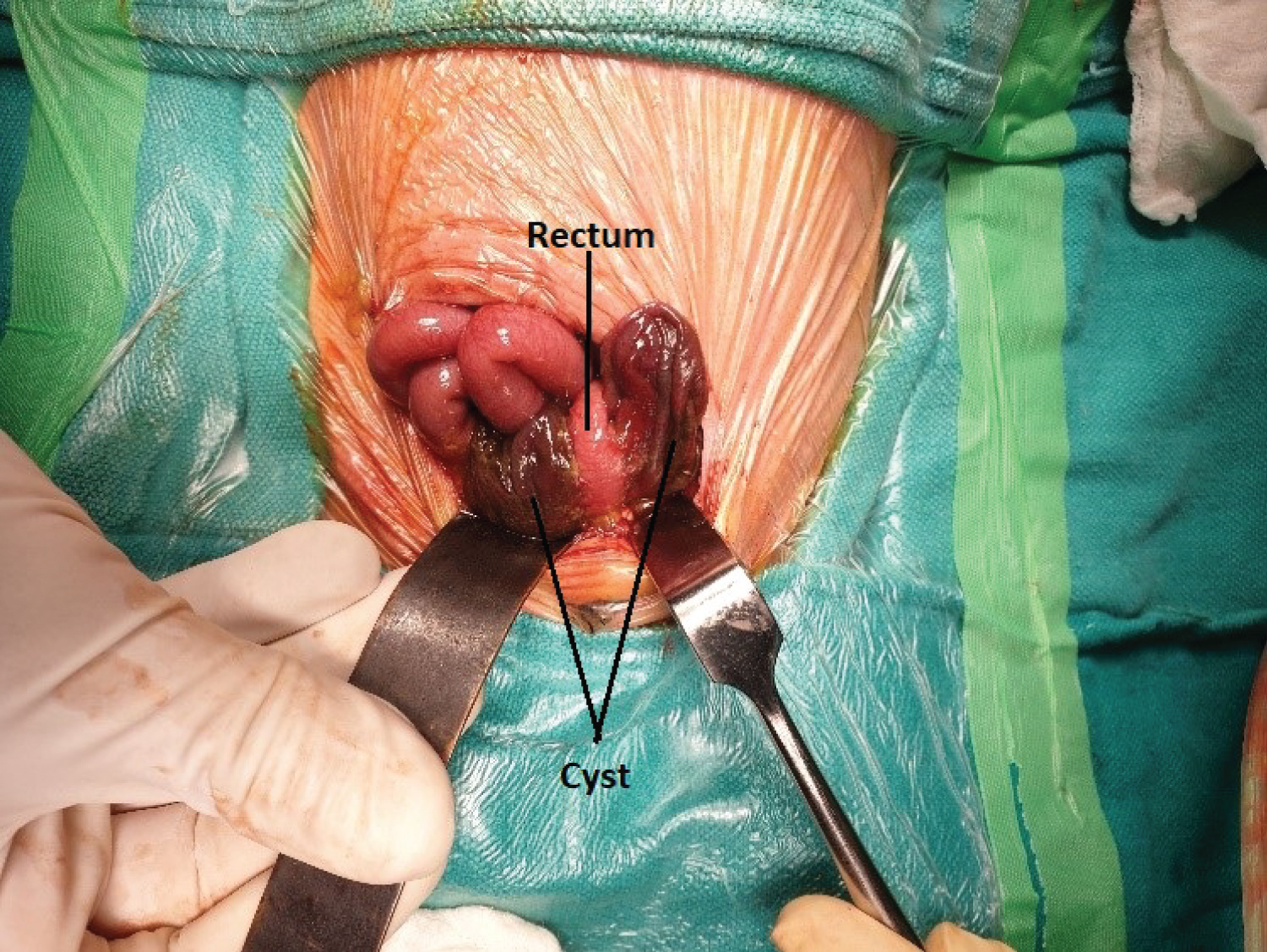
Blood investigations including a hemo gram, liver and kidney function tests and an ABG were done which revealed leukocytosis. After initial stabilization with fluids, the patient was taken for an emergency exploratory laparotomy, under anesthesia, with due risk. At surgery, via a posterior approach over the median raphe in the jack-knife position, a large enteric duplication cyst behind the rectum, occupying Para-rectal spaces on both the side (Figure -3) and hernia ting through the pelvic floor on both the sides (Figure 4) was found. It was communicating with the rectum via two openings and had a small intraperitoneal perforation. The cyst, including the mucosa, was excised and both the openings with which the rectum was communicating with a cyst were repaired primarily, and a proximal covering high sigmoid loop colostomy was fashioned.
There was no attempt made to repair the hernia defect, as it had presumably resulted due to the space-occupying lesion. Once this lesion had been excised, we expected the hernia defect to close naturally, which happened as expected. After an uneventful operative and postoperative course, the child was discharged.
Postoperatively, after 9 months, the patient developed a rectal stricture at the site of communication to the cyst. After 11 months, the patient was taken for exploratory laparotomy with revision of sigmoid colostomy (for sunken stoma) andante grade dilatation of rectal stricture.
At present,6 months after the previous surgery, the child is waiting for stoma closure and there is no residual or recurrent pelvic hernia.
Discussion
Kraft et al. reported a case of a duplicate anomaly of the rectum in 1962. They concluded that only 70 such cases were reported till that date and out of those 70 cases 38 cases were tubular hindgut duplications and 32 were cystic lesions [10]. Since then, less than 100 cases of rectal duplication cysts have been reported in the literature [5,7].
PH are very rare and occur through defects in pelvic floor musculature [11]. Although there are very limited reports of PH, literature is rife with confusing names ascribed to the condition. PH may be primary (congenital or acquired) or secondary (usually following reconstructive pelvic floor surgeries). The primary forms of PH are extremely rare and even rarer in the pediatric population. Of the 100 reported cases, [12] only 6 are reported in children.
The perineum, rhomboid in shape, is divided into two triangles by an imaginary transverse line, anterior to the is chial tuberosities (Figure 4). The anterior perineal triangle differs between the two genders, both anatomically and in the frequency and type of hernias encountered. The posterior triangle or anal perineum is, however, very similar in both genders.
The differential diagnoses of a perineal hernia include hematomas, lipomas, fibromas, rectocele, cystocele, rectal prolapse or abscess. The clinical presentation of PH is usually with an uncomplicated, soft, reducible mass in the perineum. The hernia rarely in car creates due to a wide neck and surrounding elastic tissue. Bilateral Posterior perineal hernias protrude below the level of the gluteus maximum or through the fibres of the levatorani muscle, manifesting as bulging of the gluteal region, as reported in our case.
Clinical diagnosis of a perineal hernia is supported by investigations, such as radiography, sonography, [13] computed tomography (CT), [11] and magnetic resonance (MR) tomography [14].
However, we were unable to get these confirmatory tests done, as the PH was complicated by the presence of, intestinal obstruction with peritonitis, which warranted emergency exploratory laparotomy, in our patient.
The management of perineal hernia is very controversial, both in terms of methods for approach and technique of closure, due to the complex anatomy of the pelvic floor. In children, various authors have reported success with the perineal approach and primary closure for perineal hernia [15,16].
However, our patient, with a rectal duplication presenting as posterior perineal hernia, both rare entities in a single case and that too in a neonate, posed unique challenges. Aware of all the different alternatives available in the treatment of perineal hernias, but our case, being a case of secondary hernia due to rectal duplication cyst, a primary hernia repair was not attempted. The hernia orifice was expected to close naturally after the cyst excision, as is the principle followed for many congenital hernias. The desired result was observed later in our case, thus approving the decision taken during surgery.
Conclusion
In summary, a posterior perineal hernia, a rare occurrence may confront the physician with a diagnostic dilemma. A secondary perinea hernia with a rectal duplication cyst is the rarest of rare case. In the absence of a clear-cut preoperative diagnosis and presence of diagnostic dilemma, it is essential to stick to basic surgical principles encompassing fundamental principles of surgery, anesthesia, fluid and pain management to avoid unnecessary risk and to manage such cases successfully for which no precedent is available.
Funding Statement
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- Fitz RH (1884) Persistent omphalomesenteric remains: Their importance in the causation of intestinal duplication, cyst formation and obstruction. Am J Med Sci 88: 30-57.
- Ladd WE, Gross RE (1937) Duplications of the alimentary tract. Southern Medical Journal 30: 363.
- Gross RE (1953) Duplications of the alimentary tract. In: The Surgery of Infancy and Childhood. Philadelphia: Saunders 221-245.
- Stringer MD, Spitz L, Abel R, et al. (1995) Management of alimentary tract duplication in children. Br J Surg 82: 74-78.
- Mboyo A, Monek O, Massicot R, et al. (1997) Cystic rectal duplication: a rare cause of neonatal intestinal obstruction. Pediatr Surg Int 12: 452-454.
- Park WH, Chai SO, Park KK et al. (2001) Cystic rectal duplication: a rare cause of neonatal bladder outlet obstruction and hydronephrosis. Pediatr Surg Int 17: 221-223.
- Zaiem M, Zaiem F, Zaiem F et al. (2018) Rectal duplication cyst presenting as rectal prolapse in an infant. Journal of Pediatric Surgery Case Reports 32: 49-52.
- Stamatiou D, Skandalakis JE, Skandalakis LJ, Mirilas P (2010) Perineal hernia: surgical anatomy, embryology, and technique of repair. Am Surg 76: 474-449.
- Penkov N, Damianov D, Asenov Y, et al. (2015) Recurrent Perineal Hernia - Case Report and Review of the literature. Chirurgia1 10: 81-83.
- Kraft RO (1962) Duplication anomalies of the rectum. Ann Surg 155: 230-232.
- Lubat E, Gordon RB, Birnbaum BA, et al. (1990) CT diagnosis of posterior perineal hernia. AJR Am J Roentgenol 154: 761-762.
- Skandalakis J (1994) Perineal hernias. In: Bend avid R, editor. Prostheses and abdominal wall hernias. Austin: RG Landes Company 556-567.
- Singer AA (1994) Ultrasonographic diagnosis of perineal hernia. J Ultrasound Med 13: 987-988.
- Singh K, Reid WM, Berger LA et al. (2001) Translevator gluteal hernia. IntUrogynecol J Pelvic Floor Dysfunct 12: 407-409.
- Wakeley C, Wakeley J (1989) Rare types of external abdominal hernias. Schwartz SI, Ellis H, Husser WC, editors. Maingot's abdominal operations. Norwalk: Appleton & Lange 1650-1660.
- Pearl RK (1989) Perineal hernia. In: Nyhus Lm, Condon RE, editors. Hernia. Philadelphia: JB Lippincott 441-446.
Corresponding Author
Dr. Pramod Kumar Sharma, Additional Professor and Head, Dept. of Pediatric Surgery, AIIMS, Bhopal, M.P. India, 462020, +91-8889222200
Copyright
© 2022 Sharma PK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.