The Importance of Allis Maneuver in the Management of Traumatic Posterior Hip Dislocation in Children: A Report of Two Cases
Abstract
Background: Traumatic hip dislocation happens infrequently in children. Prompt diagnosis and management are crucial to prevent complications such as osteonecrosis, osteoarthritis, and recurrent dislocation.
Case presentation: In this report, we have presented two pediatric cases of posterior traumatic hip dislocation with 5 and 6 years of age. The diagnoses were made based on the history of trauma, symptoms, and anteroposterior hip radiographs. The closed reduction in both cases was achieved with the Allis maneuver. There was no sign of joint widening in post-reduction radiographs. A 4-week Spica cast was used for immobilization and an immediate weight-bearing was advised after the cast removal. During the two-year follow-up period, the patients regained full recovery without any complications.
Conclusion: The Allis maneuver can be used as a reliable alternative for joint reduction when the gentle traction method is not successful. To exclude incomplete reduction, a post-reduction radiograph is needed, followed by a CT or MRI in the presence of any joint widening.
Keywords
Child, Hip dislocation, Pediatrics, Trauma
Introduction
Traumatic hip dislocation is an uncommon condition in children which requires prompt diagnosis and management [1,2]. Due to the laxity of the joint structures at younger age, the dislocation may happen with a low-energy trauma [3,4]. Similar to adults, the posterior dislocation is more frequent than anterior type [5].
Since hip dislocation may disturb the vascular supply of the femoral head, a vascular necrosis (AVN) is one of the most important complications in children [4,5]. There have been several reports of neglected cases with a significant incidence of AVN and recurrent subluxations which highlights the importance of timely diagnosis and management [6].
In this report, we present our experience with the management of posterior traumatic hip dislocations in two pediatric patients.
Case Presentation
Case 1
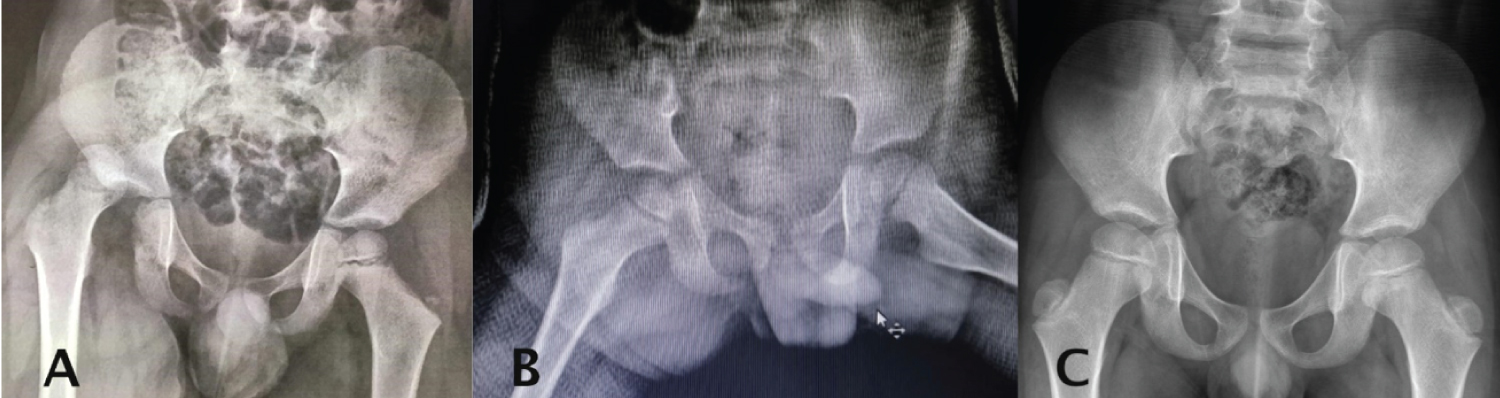
A 5-year-old boy was referred from another medical center to the Shariati Hospital (Tehran, Iran) after falling down 5 stairs. Since the chief complaint was knee pain, the hip dislocation remained undiagnosed for eight hours before referral to our center. In physical examination, the right lower limb appeared shorter than the unaffected side and was in adduction and flexion (Figure 1). There was no remarkable finding in neurological examination. The AP radiography was suggestive of posterior dislocation of the right hip (Figure 2A).
Under general anesthesia, we tried to reduce dislocation with gentle traction [5]. However, the successful reduction was not achieved and the Allis maneuver was employed instead. For the Allis maneuver, in the supine position, simple inline traction was applied to the injured leg with the knee flexed 90 degrees while the pelvis was stabilized. Then, the leg was gently extended while externally rotating the hip and reduction was achieved with a "clunk" [7]. After closed reduction, the hip stability was assessed by range of motion (ROM) test and fluoroscopic imaging.
A hip Spica cast was placed after detecting no obvious joint widening in the operating room. The neurologic examination was normal. No joint widening was visible in the post-reduction AP radiograph (Figure 2B). Based on the unavailability of the MRI setting for pediatric patients in the region, general hospital policy was to avoid further imaging workup with computed tomography (CT) scan or MRI in the absence of joint widening. The patient was discharged the day after surgery.
The follow-up visits were performed at three months, six months, and two years after surgery. We detected no complication during two years of follow-up (Figure 2C).
Case 2
A 6-year-old girl was admitted to the emergency department (ED) of the Robert Debre Hospital (Paris, France) after falling from a scooter. The right lower limb was in flexion, adduction and internal rotation, appearing shorter than the other leg (Figure 3). No neurological disorder was evident and her physical examination was otherwise unremarkable. The anteroposterior (AP) hip radiograph showed a right-sided posterior hip dislocation (Figure 4A).
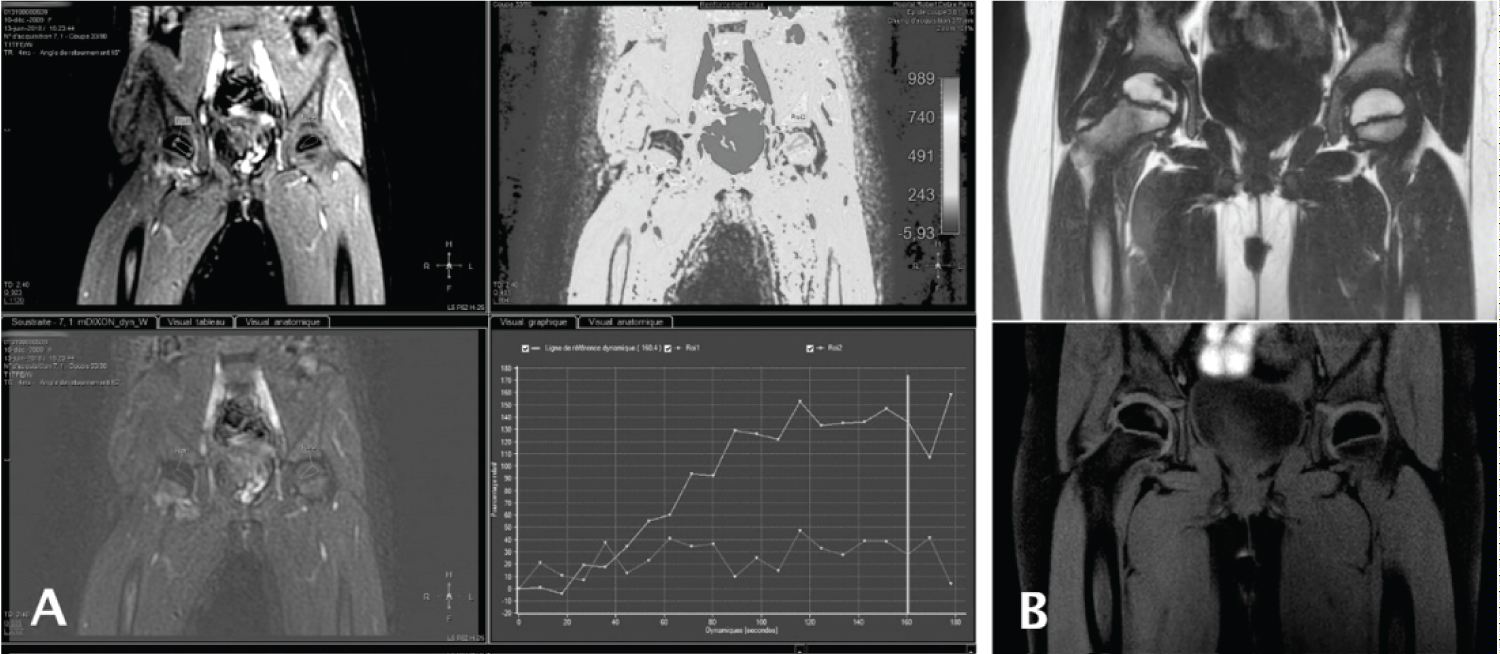
Similar to the previous case, the right hip was reduced by the Allis maneuver. The stability was checked by the ROM test and fluoroscopy. A hip Spica cast was then applied. The AP view of hip radiography showed complete hip reduction without any obvious joint widening (Figure 4B). According to our Hospital's protocol, a magnetic resonance imaging (MRI) was performed to evaluate associated pelvic fractures and study femoral head vascularization. We found a focal diminished vascularity of the right femoral head which required follow-up imaging (Figure 5A). The day after surgery, we discharged the patient after educating the parents regarding the Spica cast and necessity of the follow-up investigation.
Four weeks later, hip radiography confirmed the congruency of the joint. We removed the Spica cast and advised the patient to begin weight-bearing as tolerated. After one month, she was able to walk easily.
The follow-up visits were held similar to the previous case. A partial AVN was detected in the follow-up MRI six months after the surgery (Figure 5B), which was resolved during the two-year follow-up period without any sequela. The patient had no further complications or complaints (Figure 4C).
Discussion
In this report, we have presented two cases of pediatric traumatic hip dislocation from two different countries. Both cases were injured by a low-energy trauma and none of them had associated acetabular or femoral head fractures.
With prompt diagnosis and correct management, the overall prognosis of traumatic hip dislocation is good [4,5,8]. The history of trauma, common symptoms (e.g. pain, inability to walk, etc.), and appropriate imaging should be considered carefully to avoid misdiagnosis [6]. The mild nature of trauma or accompanying injuries can distract the physician and result in a delayed diagnosis [9]. In our first case, the concentration of pain in the child's knee (referral pain) was the source of confusion. Thus, after a minor or major trauma, the hip dislocation should be considered when there is limping, continued pain in the lower extremity (hip, thigh, or knee), abnormal extremity position, limb length discrepancy, or decreased range of motion [3]. Also, it is important to consider the possibility of associated fractures especially in the acetabulum, head and neck of the femur, and greater trochanter [10].
The complications of traumatic hip dislocation in children can happen as a result of trauma, delayed diagnosis, or failed treatment. AVN of the femoral head is an important complication with an incidence of 3-15% which can be prevented by early reduction [4,11-13]. Osteoarthritis is usually associated with other complications such as AVN and acetabular fractures [14-16]. Recurrent dislocation is more common in younger children due to the soft nature of the posterior acetabular cartilage [3,12,17]. Nerve injury (sciatic and superior gluteal nerves) can happen at the time of dislocation and has an incidence of up to 20% [18,19]. The Coxa magna is a deformity of the femoral head and usually causes no symptoms. It happens due to epiphyseal hypertrophy and is thought to be associated with younger ages, not to the magnitude of trauma [5]. In our first case, the patient did not develop any complications, despite an 8-hour delay in reduction. Similarly, the second case was symptom-free after two years, even though she endured a partial AVN at the 6-months MRI. This can demonstrate that partial AVN has a good prognosis after closed reduction of hip dislocation.
The first line imaging for diagnosis is high-quality X-ray. However, the use of other modalities including CT scan and MRI are growing to assess the associated lesions and the vascular supply to the femoral head [3,6,19,20]. Thanacharoenpanich, et al. demonstrated that some structural injuries such as entrapment of posterior labrum and posterior unossified acetabular fractures are only detectable by MRI [21]. In an immature pelvis, MRI is the best modality to provide a comprehensive assessment of the cartilage components which is extremely helpful in cases with spontaneous or incomplete reduction (due to interposed bone or soft tissue) [3,6].
Minor trauma can lead to a transient hip dislocation that spontaneously reduces while the interposition of the capsule or labrum remains [22,23]. Therefore, it is crucial to obtain necessary imaging in children with hip, thigh, or knee pain, even after a low-energy trauma.
According to the previous studies, most hip dislocation cases in children can be reduced with gentle traction under general anesthesia [3,5]. This method failed in both of our cases. Consequently, the Allis maneuver was used for a successful reduction.
The clunk we felt during Allis maneuver may be due to the interposition of the adjacent tissues which was resolved with this technique. For a closed reduction, a maximum number of two attempts is permitted. In neglected hip dislocations, and in case of failed or incomplete reduction, an open reduction is indicated [3,19].
Detecting incomplete reduction is an important part of post-reduction evaluations. Any joint widening found on post-reduction X-ray could be a red flag for incomplete reduction and CT or MRI should be obtained to detect interposed osteochondral or capsular elements [5]. In a retrospective case series conducted by Strüwind, et al. eight adolescent patients with traumatic hip dislocation and immediate closed reduction were evaluated with either MRI or CT scan after reduction. They concluded that MRI is generally recommended for pediatric traumatic hip dislocation after a closed reduction, because CT scan was not completely successful in excluding labral lesion or interposition [20].
Although the post-reduction approach is still a matter of discussion, there is a tendency to use Spica cast for 3-6 weeks in children younger than 10 years of age and a crutch-protected non-weight-bearing period of 6-12 weeks for older children and adolescents [3,9,13,24,25]. In both of our cases, the Spica cast was used for 4 weeks and an immediate full-weight-bearing was advised with a satisfactory outcome. Further investigations are needed to determine the optimum post-reduction immobilization approach.
Conclusion
Since traumatic hip dislocation is not common in children, it is crucial for physicians to be familiar with this condition to provide correct diagnosis and prompt treatment. To avoid misdiagnosis, every orthopedic surgeon should focus on the history of trauma, common symptoms (e.g. limping, continued pain in the lower extremity, abnormal extremity position, decreased range of motion, etc.), and appropriate imaging to rule out spontaneous reduction. According to our experience, when the gentle traction method is not successful, the Allis maneuver can be used as a reliable alternative for joint reduction. To exclude incomplete reduction, a post-reduction radiograph is needed, followed by a CT or MRI in the presence of any joint widening.
References
- Gardner ROE, Worku N, Nunn TR, et al. (2020) Management of neglected traumatic hip dislocation in children. J Pediatr Orthop 40: 554-559.
- Thompson VP, Epstein HC (1951) Traumatic dislocation of the hip: A survey of two hundred and four cases covering a period of twenty-one years. J Bone Joint Surg Am 33: 746-778.
- Herrera-Soto JA, Price CT (2009) Traumatic hip dislocations in children and adolescents: Pitfalls and complications. J Am Acad Orthop Surg 17: 15-21.
- Mehlman CT, Hubbard GW, Crawford AH, et al. (2000) Traumatic hip dislocation in children. Long-term follow up of 42 patients. Clin Orthop Relat Res 376: 68-79.
- Vialle R, Odent T, Pannier S, et al. (2005) Traumatic hip dislocation in childhood. J Pediatr Orthop 25:138-144.
- Matsubayashi S, Kanzaki E, Tsujimoto R, et al. (2020) N eglected subluxation of the hip after trauma: A case report. Ann Med Surg Lond 57: 223-227.
- Dawson-Amoah K, Raszewski J, Duplantier N (2018) Dislocation of the hip: A review of types, causes, and treatment. Ochsner J 18: 242-252.
- Hougaard K, Thomsen PB (1986) Traumatic posterior dislocation of the hip-prognostic factors influencing the incidence of avascular necrosis of the femoral head. Arch Orthop Trauma Surg 106: 32-35.
- Zrig M, Mnif H, Koubaa M, et al. (2009) Traumatic hip dislocation in children. Acta Orthop Belg 75: 328-333.
- Epstein HC (1973) Traumatic dislocations of the hip. Clin Orthop Relat Res 92: 116-142.
- Barquet A, Vécsei V (1984) Traumatic dislocation of the hip with separation of the proximal femoral epiphysis. Report of two cases and review of the literature. Arch Orthop Trauma Surg 103: 219-223.
- Offierski CM (1981) Traumatic dislocation of the hip in children. J Bone Joint Surg Br 63: 194-197.
- Sulaiman AR, Munajat I, Mohd FE, et al. (2013) Outcome of traumatic hip dislocation in children. J Pediatr Orthop B 22: 557-662.
- Hougaard K, Thomsen PB (1989) Traumatic hip dislocation in children. Follow up of 13 cases. Orthopedics 12: 375-378.
- Momii K, Hamai S, Motomura G, et al. (2019) Revascularization of the necrotic femoral head after traumatic open anterior hip dislocation in a child: A case report. J Med Case Rep 16: 254.
- Guingand O, Rigault P, Padovani JP, et al. (1985) Traumatic hip dislocations and acetabular fractures in children. Rev Chir Orthop Reparatrice Appar Mot 71: 575-585.
- Muratli HH, Dağli C, Biçimoğlu A, et al. (2004) SRecurrent traumatic hip dislocation in a child. Acta Orthop Traumatol Turc 38: 149-153.
- Cornwall R, Radomisli TE (2000) Nerve injury in traumatic dislocation of the hip. Clin Orthop Relat Res 377: 84-91.
- Furuya H, Shimamura Y, Kaneko K, et al. (2014) Traumatic dislocation of the hip in a child caused by trivial force for age. Case Rep Orthop 467246.
- Strüwind CM, von Rüden C, Thannheimer A, et al. (2018) Relevance of MRI after closed reduction of traumatic hip dislocation in children. Z Orthop Unfall 156: 586-591.
- Thanacharoenpanich S, Bixby S, Breen MA, et al. (2020) MRI is better than ct scan for detection of structural pathologies after traumatic posterior hip dislocations in children and adolescents. J Pediatr Orthop 40: 86-92.
- Price CT, Pyevich MT, Knapp DR, et al. (2002) Traumatic hip dislocation with spontaneous incomplete reduction: A diagnostic trap. J Orthop 2002 16: 730-735.
- Olsson O, Landin LA, Johansson A, et al. (1994) Traumatic hip dislocation with spontaneous reduction and capsular interposition: A report of 2 children. Acta Orthop Scand 65: 476-479.
- Morris AC, Yu JC, Gilbert SR, et al. (2017) Arthroscopic treatment of traumatic hip dislocations in children and adolescents: A preliminary study. J Pediatr Orthop 37: 435-439.
- Garg V, Singh AP, Singh AP, et al. (2014) Traumatic bilateral posterior hip dislocation in 10 year old male child. J Clin Orthop Trauma 5: 154-156.
Corresponding Author
Mohammad Hossein Nabian, MD, Center of Orthopedic Trans-Disciplinary Applied Research (COTAR), Tehran University of Medical Sciences, Tehran, Iran, Tel: +989126305095, Fax: 982184901000
Copyright
© 2021 Ilharreborde B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.