Periosinus Abscess Mimicking Sinus Vein Thrombosis
Abstract
Sigmoid sinus vein thrombosis is a rare but life-threatening complication of acute otitis media and mastoiditis. In this case, a 7-years-old male patient who was admitted to our pediatric emergency department with complaints of headache, blurred vision and slippage in the eye was diagnosed with perisinus abscess mimicking right sigmoid sinus vein thrombosis after examination and radiological evaluation and followed up with acetosalamide and dmah. During the follow-up, lumbar puncture (LP) was performed several times for diagnostic and therapeutic purposes and lumboperitoneal shunt placement was required.
Keywords
Sigmoid sinus thrombosis, Perisinus abscess, Lumboperitoneal shunt
Introduction
Cerebral vein thrombosis (CVT) consists of partial or complete occlusion of a sinus or cerebral vein [1]. CVT accounts for 0.5-1% of all ischaemia [2]. CVT may be observed in all age groups, but it is more common in the neonatal and childhood periods. The estimated annual incidence of CVT in childhood is 0.7 per 100,000 [3]. Although it is difficult to make a diagnosis, it is being recognised more and more thanks to the widespread use of advanced imaging techniques such as CT venography, MR venography and digital substraction angiography [1].
Two systems have been defined regarding the distribution of dural venous sinuses. The superficial system includes the superior sagittal sinus and cortical veins; the deep system includes the transverse (lateral) sinus, vein of Galen, straight sinus, sigmoid sinus. After all of them merge, they join the systemic circulation as the internal jugular vein in the more distal part. The most common thrombosis sites are transverse sinuses, superior sagittal sinuses, sigmoid sinuses, deep venous system and cortical veins [4,5].
CVT typically causes severe headache. In addition, visual problems, seizures, focal neurological deficits, confusion and death may also be observed [1,6,7]. Commonly reported risk factors for paediatric CVT include birth complications, sepsis, respiratory failure, otitis media, head and neck infections, cancer, head trauma, acquired or inherited thrombophilia and use of hormonal contraceptive methods [3,6-11]. Among laboratory tests, there is no specific serological marker to confirm the diagnosis of CVT, but routine examination of haemogram, biochemistry and coagulation values is recommended. Although a high serum level of D-dimer supports the diagnosis, a normal level does not rule out the diagnosis. Although increased CSF pressure and mild elevation in protein and cells are observed, lumbar puncture has no place in the diagnosis. There are three main targets in patients with CVT. These are anticoagulation, reduction of intracranial pressure and treatment of the underlying cause [12-14].
A brain abscess is defined as a pus-filled area of infection confined within the brain. It is a life-threatening infection of the brain parenchyma and there is a risk of neurological deficit among survivors. Head trauma, neurosurgical intervention, cyanotic congenital heart disease, chronic ear infection, mastoiditis, dental infections have become important predisposing conditions in brain abscess. Brain abscess continues to be a difficult disease as it may require neurosurgical drainage and high dose antibiotic treatment [15].
Case Report
A 7-year-old male patient presented to the ophthalmology outpatient clinic in an external centre with complaints of headache, blurred vision and slipping of the eyes approximately 1 week after adenoidectomy and tonsillectomy operation. Papillary stasis was detected and the patient was referred to our clinic. It was learnt that the patient's complaints of severe headache and eye shifting started 1 week after the operation and she had an ear infection before the operation. There were no findings except bilateral inward gaze limitation in the eyes. Nuchal rigidity was not detected. Laboratory results at the time of admission were unremarkable.
The patient was hospitalised and clexane (enoxaparin sodium) and diazomide (acetazolamide) treatments were started. Papillary oedema was detected on ophthalmological examination. LP was performed for diagnostic and therapeutic purposes. Bos pressure was measured as 21 cmH 2 O and the cavity was drained. Protein c, protein s, antithrombin 3, homocysteine, and genetic thrombophilia panel were sent from the patient, and the results were normal. The patient was thought to have sinus vein thrombosis on the background of mastoiditis. The patient was followed up with anticoagulant, diazomide and antibiotic treatment during hospitalisation. The patient was discharged with anticoagulant and diazomide. Two weeks after discharge, the patient re-presented to our emergency department with complaints of headache, shifting eyes and vomiting. Grade 3-4 papillary oedema was detected. MRI of the patient revealed "subacute-chronic phase thrombus at the level of the right jugular bulb". MRI revealed "bilateral mastoid sinus and middle ear cavity effusion, mucosal thickening in the paranasal sinuses and partial emptycella with increased optic nerve perineural CSF distance (intracranial hypertension?)". LP was performed. Bos pressure 90 cmH 2 O was measured. Ceftriaxone was started when 10 mm 3 /lt leucocytes were observed in the CSF. Diazomide and clexane treatments were continued. The patient was evaluated by otorhinolaryngology (ENT). Mastoiditis was not considered. Eye examinations were continued. Two weeks after hospitalisation, the papillary oedema regressed and the patient was discharged and continued to be followed up in the outpatient clinic. In the outpatient follow-up, papillary oedema increased and the patient was evaluated by neurosurgery and LP was performed. Bos pressure was measured as 11 cmH 2 O. The neurosurgeon advised that no operation was required and the patient should continue to be followed up. During outpatient follow-up, grade 4 papillary oedema was found again and the patient was interned and LP was performed again. Bos pressure was measured as 82 cmH 2 O. Diazomide and clexane treatments were continued. The patient was told by neurosurgery that a lumboperitoneal shunt should be inserted and the shunt was inserted. After shunting, diazomide dose was decreased and control imaging was performed. On MRI, the appearance of partial empty sella and increased perineural CSF distance of the optic nerve described in the previous MRI was not observed in the current examination. The appearance suggestive of chronic thrombus at the level of the right jugular bulb and slow flow in the right transverse sinus persist. '' was reported as ''. The patient's anticoagulant was changed to coumadin (warfarin sodium) and the patient was externised.
Approximately 1 month after discharge, the patient presented to the paediatric emergency department again with severe headache and eye pain. Neurological examination revealed no nuchal rigidity. Blood samples were unremarkable. MRV and CT venography were performed.
They were evaluated as normal. Diazomide treatment was discontinued in the outpatient clinic follow-up and diazomide was restarted when papillary oedema was detected on ophthalmological examination. Ceftriaxone was started because of a history of mastoiditis. ENT stated that the mastoid process was normal and no sinus vein thrombosis was observed. In the follow-up of the patient, there was an increase in temperature, hyperaemia and discharge at the shunt incision site. Ultrasonography (USG) revealed "Increased thickness and echogenicity in the fatty tissue around the catheter and oedematous appearance.
A fluid collection with dense content up to 6 mm in the thickest part around the catheter was observed. Pediatric surgery was consulted in terms of abscess around the catheter and it was not evaluated as abscess and no drainage was required. Antibiotherapy was organised for the patient whose shantogram and CT scan were reported as normal. There was no growth in the wound culture taken from the shunt incision site. No abscess was observed. The lumboperitoneal shunt of the patient who had no thrombosis and no need for shunt was removed. Antibiotherapy was completed for 10 days and the patient was discharged to be followed up in the paediatric neurology outpatient clinic. Outpatient follow-up of the patient continues.
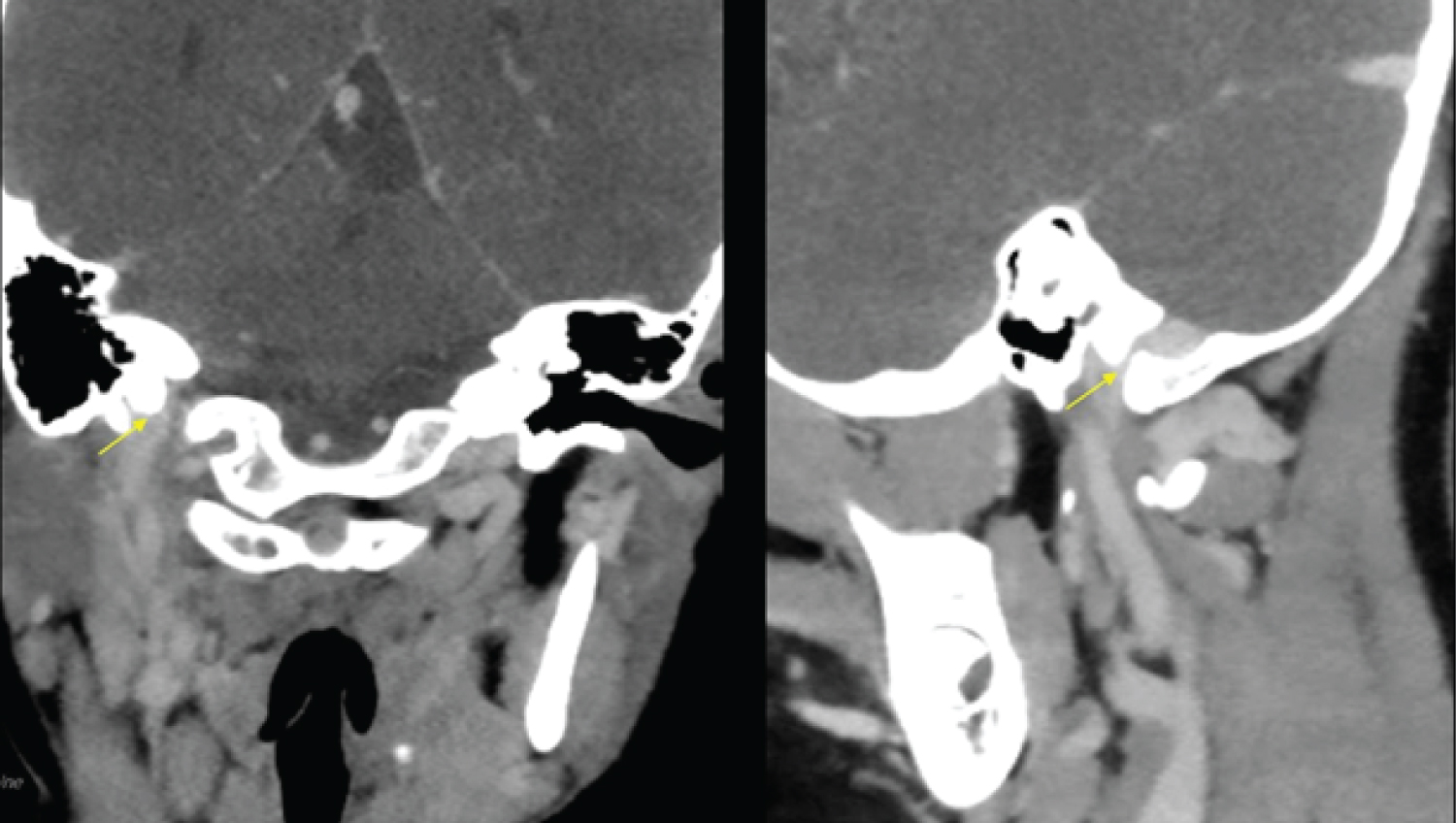
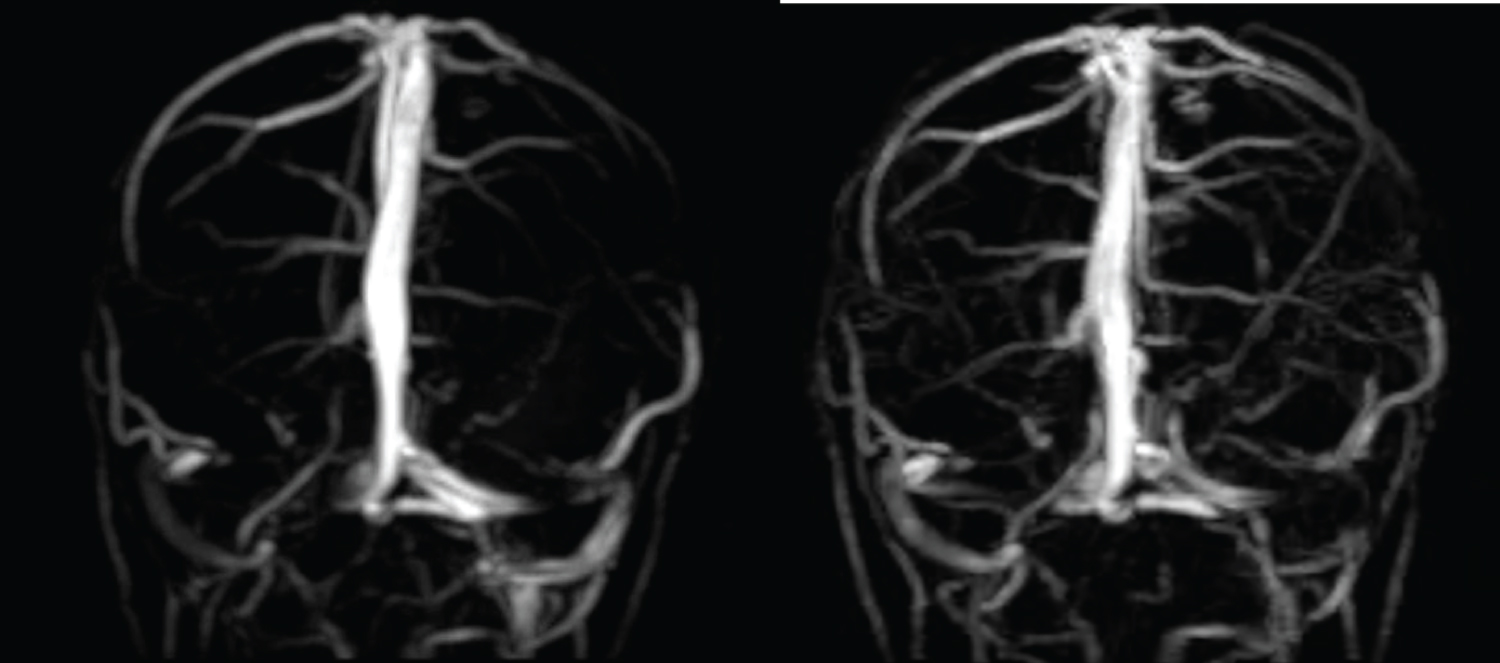
The patient underwent brain computed tomography (CT) (Figure 1 and Figure 2), magnetic resonance imaging (MRI) and high-resolution magnetic resonance venography (MRV) (Figure 3 and Figure 4) with a prediagnosis of sinus vein thrombosis. Radiological findings of sinus vein thrombosis clinic caused by perisinus abscess can be seen in CT and MR images.
Discussion
Although thrombosis is mostly known as an adult disease, many articles related with thromboembolism in paediatric patients have been published in recent years [16,17]. The frequency of thromboembolic events in childhood is lower than in adults, but mortality and morbidity are high. Lawson, et al. gave this frequency as 0.7 per 100000 per year in children [18].
Thrombosis is a multifactorial event. It usually develops with a combination of hereditary and acquired risk factors [19,20]. Common childhood infections, dehydration, some types of anaemia (sickle cell anaemia, severe iron deficiency anaemia), congenital heart diseases, nephrotic syndrome, systemic lupus erythematosus and malignancies are among the causes of thrombosis. In addition to these systemic risk factors, head or neck traumas, central nervous system tumours and venous stasis following intracranial surgery may also lead to thrombosis [21]. The rate of association with hereditary prothrombotic diseases in childhood thromboembolism cases ranges from 3.9% to 83% and is observed more frequently in contrast to adults. Lawson, et al. [22] reported the rate of detection of hereditary factors in symptomatic thromboembolism cases as 43% and Gürgey, et al. [16] reported the frequency of hereditary etiology as 32.5%. Therefore, it is beneficial to investigate prothrombotic genetic factors in childhood thrombosis cases. In our patient, protein c, protein s, antithrombin 3, homocysteine and genetic thrombophilia panel were investigated and found to be normal.
In the literature, the most common complaint at presentation to hospital is headache [23]. In a study conducted in children at Marmara University, headache was found to be the most common presenting complaint and diplopia was the second most common presenting complaint in accordance with the literature. Papil oedema was found on neurological examination in all but one of the patients who presented with headache [24]. Our case also presented to the hospital with complaints of headache, blurred vision and diplopia and papillary oedema was found on examination.
Radiological examinations that should be performed for the diagnosis of cerebral thrombosis include brain MRI and MR venography. Cerebral conventional angiography may be performed in suspected cases in which only cortical veins are involved [25].
Although brain computed tomography is an easily accessible examination, it may be normal in 20-30% of cases [26,27]. In our case, the diagnosis was made by brain MRI and MRV. Although thrombosis in the sagittal sinus has been reported most frequently in the literature, thrombosis was found in the right sigmoid sinus in our case [28].
Antibiotic treatment with intravenous second or third generation cephalosporins is recommended in cases of cerebral thrombosis and brain abscess associated with otitis media and mastoiditis [15,21]. In our case, we used ceftriaxone, one of the third generation cephalosporins.
There is no evidence-based recommendation due to the lack of studies in the treatment of cerebral thrombosis in childhood. The aim of antithrombotic treatment is to ensure patency of the vascular bed and to prevent thrombosis spread and new thrombosis formation after acute treatment [28]. Antithrombotic agents used after the diagnosis of thrombosis in paediatric patients published in the last 10 years differ from each other [21]. Different treatment protocols are used in different centres; heparin, low molecular weight heparin or oral warfarin is preferred in the acute period, and anticoagulant treatment with low molecular weight heparin or oral warfarin is continued for 3-6 months after the acute period. In our patient, we preferred low molecular weight heparin in the acute period and afterwards.
In patients presenting with pseudotumour cerebri clinic, acetozolamide treatment may be required until the signs of increased intracranial pressure disappear and CSF pressure returns to normal; lumboperitoneal shunt may be applied in treatment-refractory cases [24]. In our case, the patient needed lumboperitoneal shunt, but the shunt was removed because he no longer needed it in the follow-up.
In conclusion, perisinus abscess mimicking cerebral thrombosis in childhood is difficult to differentiate by physicians because it is rare, both may present with similar neurological symptoms and may also occur as a complication of common infections such as otitis media. Therefore, in the presence of concomitant risk factors, the possibility of cerebral thrombosis and brain abscess should be considered in patients presenting with headache and neurological deficit, and MRI and MRV should be performed early in case of suspicion.
Conflict of Interest Declaration
There is no conflict of interest between the authors of this study.
Summary of Researchers' Contribution Ratio Declaration
All authors declare that they have contributed equally to the article.
Informed Consent
Informed written consent was obtained from the patient presented in this article.
References
- Silvis SM, Sousa DA, Ferro JM, et al. (2017) Cerebral venous thrombosis. Nat Rev Neurol 13: 555-565.
- Ulivi L, Squitieri M, Cohen H, et al. (2020) Cerebral venous thrombosis: A practical guide. Pract Neurol 20: 356-367.
- deVeber G, Andrew M, Adams C, et al. (2001) Cerebral sino venous thrombosis in children. N Engl J Med 345: 417-423.
- Kaya D (2017) The diagnosis and treatment of cerebral venous thrombosis. Turk J Neurol 23: 94-104.
- Idiculla PS, Gurala D, Palanisamy M, et al. (2020) Cerebral venous thrombosis: A comprehensive review. Eur Neurol 83: 369-379.
- Ichord RN, Benedict SL, Chan AK, et al. (2015) Paediatric cerebral sinovenous thrombosis: Findings of the International Paediatric Stroke Study. Arch Dis Child 100: 174-179.
- Heller C, Heinecke A, Junker R, et al. (2008) Cerebral venous thrombosis in children: a multifactorial origin. Circulation 108: 1362-1367.
- Sebire G, Tabarki B, Saunders DE, et al. (2005) Cerebral venous sinus thrombosis in children: Risk factors, presentation, diagnosis and outcome. Brain 128: 477-489.
- Grunt S, Wingeier K, Wehrli E, et al. (2010) Cerebral sinus venous thrombosis in Swiss children. Dev Med Child Neurol 52: 1145-1150.
- Wasay M, Bakshi R, Bobustuc G, et al. (2008) Cerebral venous thrombosis: Analysis of a multicenter cohort from the United States. J Stroke Cerebro Vasc Dis 17: 49-54.
- Coutinho JM (2015) Cerebral venous thrombosis. J Thromb Haemost 13: S238-S244.
- Ferro JM, Bousser MG, Canhão P, et al. (2017) European Stroke Organization guideline for the diagnosis and treatment of cerebral venous thrombosis-endorsed by the European Academy of Neurology. Eur J Neurol 24: 1203-1213.
- Saposnik G, Barinagarrementeria F, Brown RD Jr, et al. (2011) Diagnosis and management of cerebral venous thrombosis: Guidelines for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42: 1158-1192.
- Altiparmak U, Yalniz Z, Solmaz Fatana B, et al. (2008) Cerebral vein thrombosis and bilateral optic atrophy in a case with hyperhomocysteinaemia T. Oft Gaz 38: 269-272.
- Bodilsen J, D'Alessandris QG, Humphreys H, et al. (2024) European society of Clinical Microbiology and Infectious diseases guidelines on diagnosis and treatment of brain abscess in children and adults. Clin Microbiol Infect 30: 66-89.
- GürgeyA, Aslan D (2001) Outcome of non catheter-related thrombosis in children: Influence of underlying or coexisting factors. J Pediatr Hematol Oncol 23: 159-164.
- Andrew M, David M, Adams M, et al. (1994) Venous thromboembolic complications (VTE) in children: First analyses of the Canadian Registry of VTE. Blood 83: 1251-1257.
- Sutor AH, Uhl M (1997) Diagnosis of thromboembolic disease uring infancy and childhood. Semin Thromb Hemost 23: 237-246.
- Revel-Vilk S, Massirotte P (2003) Thromboembolic diseases of childhood. Blood Rev 17: 1-6.
- Bonduel M, Sciuccati G, Hepner M, et al. (2006) Arterial ischemic stroke and cerebral venous thrombosis in children: A 12-year Argentinean registry. Acta Haematol 115: 180-185.
- Dlamini N, Billinghurst L, Kirkham FJ (2010) Cerebral venous sinus (synovenous) thrombosis in children. Neurosurg Clin N Am 21: 511-527.
- Lawson SE, Butler D, Enayat MS, et al. (1999) Congenital thrombophilia and thrombosis: A study in a single centre. Arch Dis Child 81: 176-178.
- Ferro JM, Canhao P, Stam J, et al. (2004) Prognosis of cerebral vein and dural sinus thrombosis: Results of the international study on cerebral vein and dural sinus thrombosis (ISCVT). Stroke 35: 664-670.
- ünver O, Ekinci G, kutlubay B, et al. (2016) Evaluation of cerebral thrombosis cases in children. Archives of Turkish Paediatrics 51: 87-93.
- Kamisli Ö, Arslan D, Altinayar S, et al. (2009) Cerebral venous sinus thrombosis: clinical evaluation. Turkish Journal of Cerebrovascular Diseases 2: 39-42.
- Crassard I, Bousser MG. (2004) Cerebral venous thrombosis. J Neuroophthalmol 24: 156-163.
- Renowden S (2004) Cerebral venous sinus thrombosis. Eur Radiol 14: 215-226.
- Menascu S, Lotan A, Ben Zeev B, et al. (2011) Cerebral venous thrombosis in the Mediterranean area in children. Mediterr J Haematol Infect Dis 3: e2011029.
Corresponding Author
Dilara Çiçekli Yener, Department of Paediatrics, Health Sciences University Kartal Dr Lütfi Kirdar City Hospital, Istanbul, Turkey.
Copyright
© 2024 Yener DC, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.