Treatment of COVID Encephalitis in Pediatric Patient with IVIG
Abstract
We herein report a case of encephalitis in a pediatric patient with SARS-COVID-19 infection. The diagnosis is discussed consisting of physical exam, electroencephalogram, lumbar puncture, and MRI brain features. He was successfully treated with immunosuppressive therapy, intravenous immunoglobulin. This case highlights the complexities and potential treatment for similar nervous system involvement for this novel virus.
Keywords
COVID, Encephalitis, IVIG
Introduction
The SARS-CoV-2 virus has only been around for a few years. The effects on the respiratory system are well established. Its' effect on the central nervous system (CNS) is less well established, and It's effect on central nervous system in adolescents and young children are even less well established. In the pediatric population, COVID-19 (Coronavirus disease 2019) has led to life threating CNS infections, demyelinating processes, Guillain-Barre syndrome, vascular infarcts, as well as new onset or worsening seizures.1 Children have shown different inflammatory processes in response to COVID-19 as seen in the highly documented Multisystem Inflammatory Syndrome in Children (MIS-C). Individualized treatment guidelines in this population are needed [1]. Our case is an example of successful treatment for a CNS infection with immunomodulating therapy, specifically intravenous immunoglobulin (IVIG).
Presentation
An 8-year-old Caucasian boy previously healthy presented to the emergency department with an acute headache, altered mental status, and seizure-like activity. Mother noted he had mildly decreased appetite without significant weight loss over last month. He developed a headache and fatigue a few hours prior to presentation. Earlier in the day, he went to take a nap. Then was found by the family laying down in the fetal position moaning, drooling, with decreased and slowed speech. Prior to EMS arrival, the family noticed an event of bilateral arm flexing, bilateral leg stiffening, and back arching for 2-3 minutes. He was then taken to a community emergency department. In the ED, febrile 101.8 F. Other vital signs within normal ranges (blood pressure 104/76 mm Hg, heart rate 96, SpO2 98% on room air). On a mental status exam, he was obtunded, groaning with moderate stimuli and preferring to keep eyes closed. Initial lab work, head imaging, and lumbar puncture was done at this emergency department. He was then transferred to a level 1 pediatric emergency room for further evaluation.
Investigations
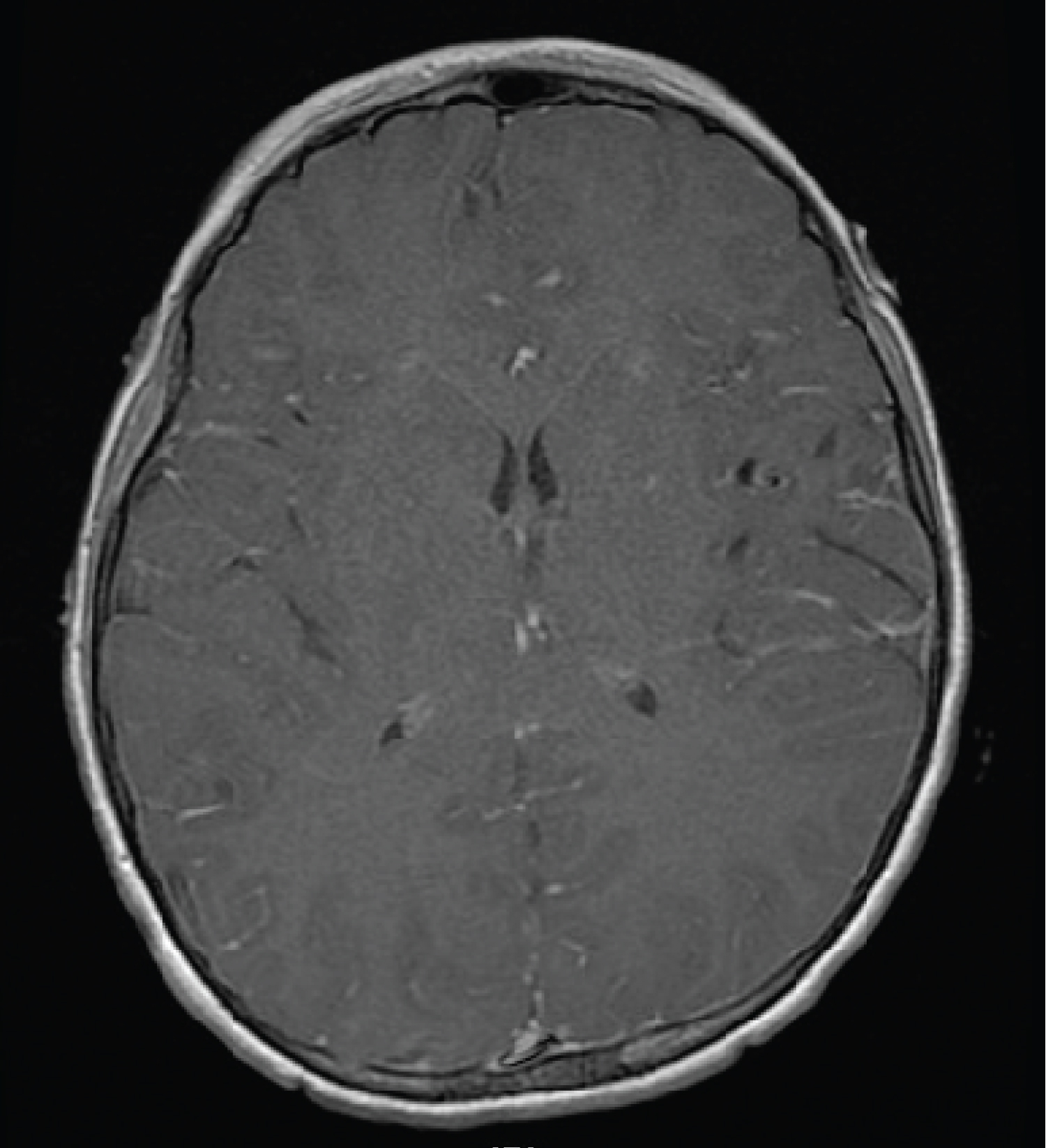
CTH was normal, obtained after giving a small amount of versed. CBC notable for mildly elevated WBC 14.1 with 80% neutrophils. CMP, ammonia, CK, salicylate level, Tylenol level, and ethanol level were unremarkable. Lumbar puncture obtained; elevated WBC 20, normal protein 36.8 and glucose 83. CSF cultures obtained and negative. Additional CSF PCR studies included cryptococcus, E coli, H. Influenza, Listeria, Neisseria Meningitidis, Group B Strep, CMV, Enterovirus, HSV-1, HSV2, HHV6, Human Parechovirus, and varicella virus negative. The urine drug screen and urine culture were negative. The viral respiratory pathogen panel via nasal swab was positive for SARS-CoV-2; the rest of the panel was negative. CoV2 IgG from a blood sample was negative. A more detailed comprehensive, expanded urine drug screen was positive for methamphetamines. MRI brain with and without contrast obtained, showed diffuse leptomeningeal enhancement (Figure 1), correlating with clinically suspected meningitis with normal brain parenchyma. Video EEG obtained for 48 hours showed frequent non rhythmic, multifocal discharges and diffuse theta slowing. By end of EEG, discharges had resolved but theta slowing persisted.
Hospital Course
Patient was admitted to the Transitional Care Unit under pediatrics with Neurology and Infectious Disease consults. Initial workup indicative of viral meningitis/encephalitis with encephalopathic exam and findings from LP, MRI, and EEG. He was given broad spectrum antibiotics for 48 hour blood and CSF culture rule out post lumbar puncture. Additionally received acyclovir until HSV blood and CSF were negative. He was put on a clonazepam 3 day regimen for provoked seizures admidst ongoing viral infection (0.5 mg clonazepam dissolving wafer q12 hours × 6 doses). He was placed on maintenance IV fluids with poor oral intake. He had little improvement over the first 2 days; he remained difficult to arouse, had limited speech, and increased sleeping. Immunologic treatment was deferred first 2 days with unclear role of positive methamphetamine. On hospital day 3 he was given intravenous intra globulin (IVIG) 2 mg/kg in one dose. Following this patient experienced dramatic improvement with eventual return to baseline in less than 24 hours. One day after this patient did have auditory and visual hallucinations over a few hours which were self resolving. Additionally he had a low pressure headache improved with caffeine and increased fluid intake. The hospital course was complicated by the social work consult for methamphetamine use. This then revealed issues of domestic abuse at home which led to the patient being taken temporarily into DCSF (District of children, schools, and families) custody with ongoing investigation.
Discussion
The effect of SARS-CoV-2 on the brain is still not fully understood. Theories have pointed towards a direct neurologic invasion with viral replication vs. immune-mediated process vs. a secondary cytokine storm within the CNS [2,3].
Our report describes a case of encephalitis associated with SARS-CoV-2 infection which showed clear clinical improvement with IVIG therapy. Our diagnosis of COVID-19 encephalitis was based on LP, MRI findings consistent with viral CNS inflammatory process, exam and EEG consistent with encephalopathy, and positive SARS-CoV-2 PCR on viral nasal swab. We did not attempt to isolate SARS-CoV-2 PCR in CSF because of the low yield in most cases [4]. Although the positive amphetamine was a confounder in the case, the altered mental status beyond 48 hour and lack of other signs of amphetamine intoxication do not suggest it played a role in the patient's encephalopathy.
There is lacking evidence on best clinical management of SARS-CoV-2 encephalitis. This disease is primarily known for its effect on epithelial tissues in the respiratory tract causing an inflammatory process that leads to dyspnea, cough, pneumonia, and in severe cases respiratory failure [5].
Additional studies since the pandemic have shown a wider inflammatory course causing multiple organ injury. In pediatrics, widespread inflammatory system injury due to proinflammatory cytokines associated with COVID-19 can be seen in the Multisystem Inflammatory Syndrome in Children (MIS-C) case [6]. COVID-19 has been documented to cause numerous neurologic manifestations. These can be mild from headache, dizziness, loss of smell or brain fog to manifestations with higher mortality such as seizures, encephalopathy, Guillain Barre syndrome or meningitis/encephalitis [5,7,8]. In fact, IVIG has shown some evidence of being used in COVID-19 related acute respiratory distress syndrome not associated with CNS manifestations [9].
Use of immunomodulators for viral encephalitis has not been well established. The use in children has shown a reputable benefit of steroids and IVIG in acute demyelinating encephalomyelitis, a more severe form of encephalitis [10,11]. The evidence has been nonconclusive for use of IVIG or steroids in other forms of viral encephalitis. Although some studies have shown possible decrease hospital stay with IVIG compared to placebo [12].
There are only a few case reports using IVIG therapy in COVID-19 encephalitis. In one case report (Mydam) a 6-year-old boy had COVID-19 induced complex febrile seizures and enhancement seen in parenchyma on MRI brain. His seizures were refractory to multiple AEDs. He then developed changes in behavior, increased sleepiness, decreased eye contact on HOD 2. He was given a 5 day course of methylprednisolone 30 mg/kg/d and 2 day course of IVIG (1 mg/kg/d). His seizures dramatically stopped after initiation of steroids and IVIG [13].
In another case, early in the pandemic, a 60-year-old man with only mild respiratory symptoms developed a severe akinetic syndrome and mutism. His viral SARS-CoV-2 nasal swab PCR test was positive. The lumbar puncture was also indicative of a viral process with negative PCR testing of common pathogens, including COVID-19. His MRI brain was normal but EEG showed generalized slowing. He was given high dose IV steroids 1g/day for 5 days. During course he had steady improvement, displaying only mild disinhibition by end of treatment. He was discharged 3 days after the end of steroid treatment and had a normal neurologic exam [14].
Conclusion
Our case report details encephalitis following COVID-19 infection in a child. His condition dramatically improved with intravenous immunoglobulins. There have been cases associated with ADEM, GBS, or autoimmune encephalitis where IVIG has been helpful in COVID-19 infected patients. There is very limited information on typical COVID-19 encephalitis treatment with immunologic therapy. Hopefully, this can serve as a successful example in further studies to determine what modality of treatment will improve patient outcome best with this novel virus.
References
- Siracusa L, Cascio A, Giordano S, et al. (2021)Neurological complications in pediatric patients with SARS-CoV-2 infection: A systematic review of the literature. Ital J Pediatr 47: 123.
- Melegari G, Rivi V, Zelent G, et al. (2021) Mild to Severe Neurological Manifestations of COVID-19: Cases Reports. Int J Environ Res Public Health 18: 3673.
- Bhola S, Trisal J, Thakur V, et al. (2022) Neurological toll of COVID-19. Neurol Sci 43: 2171-2186.
- Tandon M, Kataria S, Patel J, et al. (2021) A comprehensive systematic review of CSF analysis that defines neurological manifestations of COVID-19. Int J Infect Dis 104: 390-397.
- Veleri S (2022) Neurotropism of SARS-CoV-2 and neurological diseases of the central nervous system in COVID-19 patients. Exp Brain Res 240: 9-25.
- Kundu A, Maji S, Kumar S, et al. (2022) Clinical aspects and presumed etiology of multisystem inflammatory syndrome in children (MIS-C): A review. Clin Epidemiol Glob Health 14: 100966.
- Leonardi M, Padovani A, McArthur JC (2020) Neurological manifestations associated with COVID-19: A review and a call for action. J Neurol 267: 1573-1576.
- Gunawardhana C, Nanayakkara G, Gamage D, et al. (2021) Delayed presentation of postinfectious encephalitis associated with SARS-CoV-2 infection: A case report. Neurol Sci42: 3527-3530.
- Kindgen-Milles D, Feldt T, Jensen BEO, et al. (2022) Why the application of IVIG might be beneficial in patients with COVID-19. Lancet Respir Med 10: e15.
- Esposito S, Principi N, Semino M, et al. (2012) Steroids and childhood encephalitis. Pediatr Infect Dis J. 31: 759-760.
- Feasby T, Banwell B, Benstead T, et al. (2007) Guidelines on the use of intravenous immune globulin for neurologic conditions. Transfus Med Rev 21: S57-S107.
- Iro MA, Martin NG, Absoud M, et al. (2017) Intravenous immunoglobulin for the treatment of childhood encephalitis. Cochrane Database Syst Rev 10: 11367.
- Mydam J, Midivelly S, ValliveduChennakesavulu P, et al. (2022) Focal Seizures in a Child Following COVID-19 Infection: A Case Report. Cureus 14: e22083.
- Pilotto A, Odolini S, Masciocchi S, et al. (2020) Steroid‐responsive encephalitis in coronavirus . Annals of Neurology 88: 423-427.
Corresponding Author
Joseph Collins, MD, Pediatric Neurology Fellow, Department of Neurology, Cardinal Glennon Hospital, Saint Louis University, St. Louis, MO, USA, Tel: 8474215698
Copyright
© 2022 Collins J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.