Powered Endoscopic Septoplasty - How We Do It and Literature Review
Abstract
Functional endoscopic sinus surgery has become the standard of care for obstructive and inflammatory disease of the paranasal sinuses and microdebriders or shavers have also been one of the surgical tools frequently used in many endoscopic surgical procedures in otorhinolaryngology. This article describes the usefulness of endoscopic surgical repair of obstructive deviations of the nasal septum with powered instrumentation.
Powered endoscopic septoplasty (PES) represents a useful and a well-suited surgical alternative compared to the classic headlight septoplasty with better outcomes and an acceptable and less complicated learning curve during the surgical training of the otorhinolaryngologist.
Keywords
Septoplasty, Endoscopic repair, Powered instrumentation
Background
From the beginnings of ancient rhinological surgery until the end of the last decade of the 20th century, various surgical procedures and some technical proposals have been developed to correct the alteration of nasal breathing due to deviation of the septum [1]. During this period, surgical procedures of the nasal septum have evolved from primitive and aggressive techniques with less complications and better results that sometimes are not so optimal.
The role of the septum as a determinant of nasal shape and functionality has been recognized [1-4]. Currently used cartilaginous and bony septal obstruction correction techniques are still geared toward septal resection, but more emphasis has been placed on preservation, realignment, or realignment of the septum, combination of both. In fact, the term septoplasty takes its meaning from the Greek term meaning "to reshape the septum" [1]. Conventional septoplasty is a commonly performed ENT surgical procedure with some running variables for nasal airway obstruction or rhinologic headache due to sinus contact points, often in conjunction with other nasal procedures, including endoscopic surgery of the paranasal sinuses. Classic Septoplasty is traditionally performed with an external "headlight" approach. Although septal deformities and spurs have traditionally been removed with bone chisels and thru-cutting forceps.
With the advent of endoscopic sinonasal surgery, septoplasty techniques have been perfected and have made it possible to incorporate powered instrumentation, improving functional results with less discomfort due to surgical trauma.
Current knowledge of the anatomical complexities of the nasal cavities and their physiological characteristics have been better understood, allowing accurate surgical repair of nasal obstruction caused by nasal septum deviation when it is endoscopically assisted.
Endoscopy-guided septoplasty with powered instrumentation is useful because it allows to reshape in situ the obstructive defects of the nasal septum, especially those located at the top and back of the nasal cavities.
Powered Endoscopic Septoplasty (PES) is a useful procedure in which modern technological advances in surgical rhinoendoscopy, can facilitate a detailed and less invasive repair of obstructive pathology of the nasal septum.
Surgical Technique
Recommended anesthesia protocol includes the use of a short-acting intravenous sedative agent (Propofol) followed by continuous infusion of an ultra-short acting opiate (Remiphentanyl). This anesthetic scheme reduces the requirement of inhalatory agents and particularly it has given us some advantages such as less perioperative bleeding rate, faster and better wake up from general anesthesia and less post-surgery pain. Cotonoids soaked in Oxymetazoline like topical decongestant, were applied before septum infiltration in all patients. Under "headlight" visualization, 1% Lidocaine with 1:100 000 epinephrine was infiltrated mucoperichondrally bilaterally a few minutes before incision, in several areas of anticipated flap incision and elevation. Greater palatine foramina injections never performed for posterior hemostasis of posterolateral branch of the Sphenopalatine artery. Standard right hemitransfixion incision was employed for most deviations, although this incision can also be performed endoscopically anteriorly to the septal defect that is to be reshaped.
An essential step in endoscopic septoplasty is the correct and precise identification of the Subperichondrial plane. Meticulousness in finding the avascular perichondrial plane is important. Accurate identification of this plane minimizes the intraoperative bleeding during mucoperichondrial flap elevation and subsequent fogging endoscopic field of vision during surgery.
We recommend after hemitransfixion incision with "headlight" assistance, once the proper plane has been started, must be identified endoscopically with a sickle knife the perichondrial plane properly. Once the plane has been established a Cottle elevator is used to simultaneously complete the flap dissection. The contralateral flap is then raised in a similar fashion. The flaps are then dissected inferiorly to the nasal floor in order to address deflections of the Vomer. Endoscopic dissection of mucoperichondrial flap also help when raising the flap at the floor of the nose where the maxillary crest meets the cartilaginous septum. At this point, the mucoperiosteum is attached to the bony crest with fibrous bands. These bands should be dissected sharply to prevent mucosal tears. Likewise, endoscopic elevation of the perichondrial flap around spurs and sharp septal deviations must be performed more carefully. These areas usually have more tenacious attachments to the perichondrium y periosteum, secondary to thinning and scarring of the tissue after a traumatic deviation or during growth of the cartilage. Endoscopic detachment and elevation of perichondrium minimizes the risk and sometimes avoids perforating the mucosa. However, unilateral perforations are common and usually heal spontaneously. Even bilateral perforations heal well if small and asymmetrically located. Larger, bilateral, and opposing perforations require closure with a rotational mucosal flap or mucosal graft.
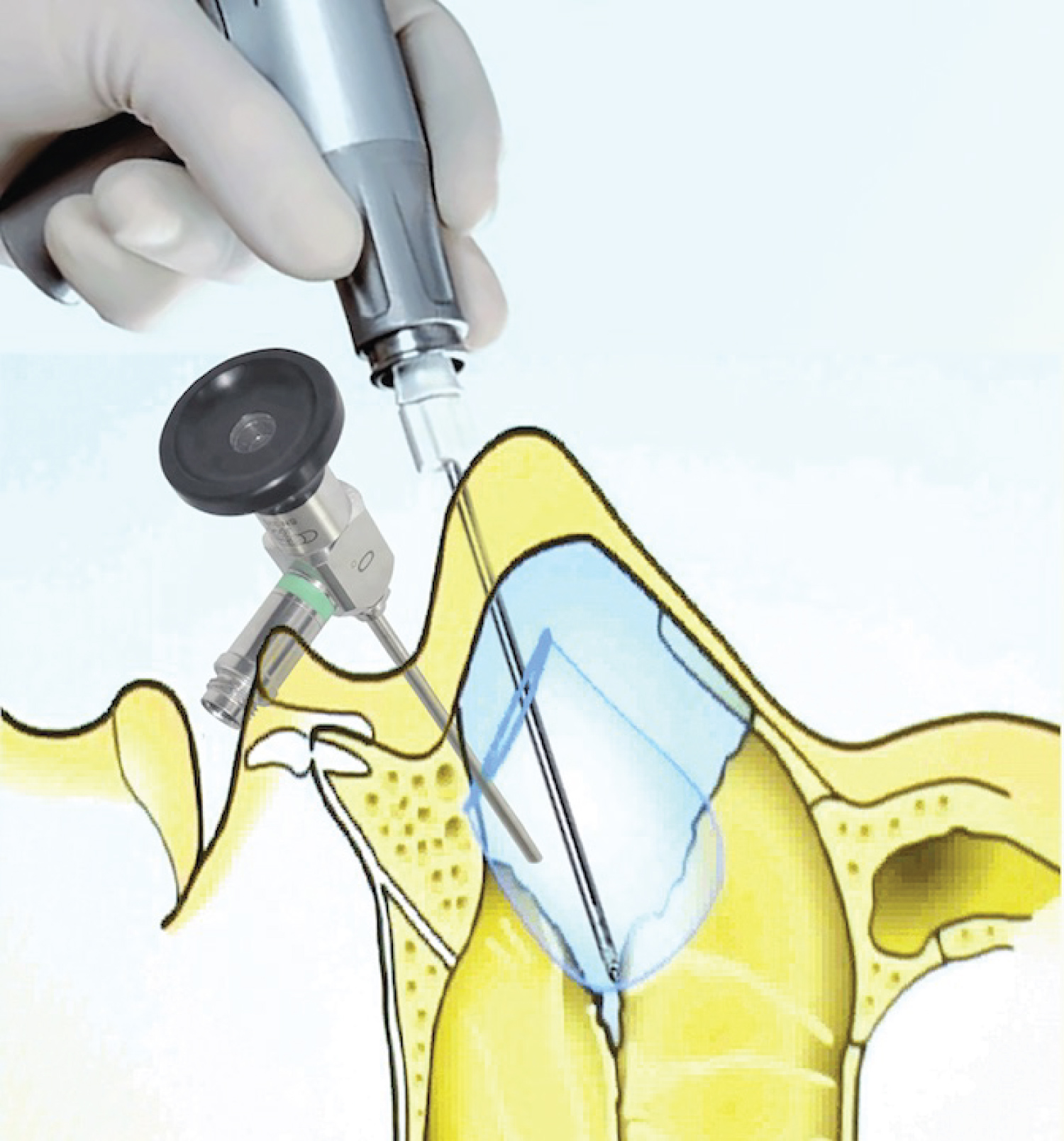
Septum deflections, spurs, fractures poorly consolidated, dislocation or contact points must be reshaped or removed endoscopically with 4 mm microdebrider bur making easy rectified defects of cartilage and bone. Use of the microdebrider system with suction and continuous irrigation allows for improved visualization during this procedure, as compared to traditional instrumentation, due to the simultaneous suctioning and resection of blood and debris (Figure 1, Figure 2 and Figure 3).
In cases with isolated superior septal deviations with contact points with the nasal lateral wall it's possible to perform a tailored unilateral approach through a vertical full thickness mucosal incision a few millimeters ahead of deflection, which typically lies at the junction between the quadrangular cartilage and the perpendicular plate of the Ethmoid. This procedure can helped significantly correct the superior septum deflection. This tailored approach is also useful in limited or isolated posterior deviations with the remainder of the septum lies straight. This type of procedure may also be called limited endoscopy septoplasty. In the same way, septal spurs can occasionally constitute the single septal pathology. A unique ipsilateral endoscopic flap dissection in these cases may be technically complicated because the mucosa overlying septal spurs is generally fragile and attenuated, which may result in an iatrogenic perforation more likely. In these cases, isolated septal spurs can be approach effectively performing a horizontal incision along the apex of the spur. Two flaps are then elevated, one along the superior aspect of the spur and a second along the inferior aspect. Next, the superior margin of the spur is fractured, dissected, and the contralateral perichondrium freed from the spur. The spur is then released and removed from its inferior attachment and the flap edges are re-approximated. Most of septal incisions through tailored approaches may not necessary the suture closure.
Usually, nasal packing is not necessary after endoscopic septoplasty. Otherwise, the placement of silicone septal splints in both nostrils offers some advantages such as stabilizing the septum, minimizing septal hematoma and synechiae and providing comfort during the initial recovery by maintaining free the airway (Figure 4). The septal splints can be removed in the first postoperative follow-up 5 days after surgery.
Discussion
Advances in rhinoendoscopic surgery are guided by the desire to offers a viable minimally invasive strategy to achieve outcomes more accurate and efficacious. The application of endoscopic techniques to the correction of septal deformities was initially described by Stammberger, et al. in 1990 [2] and Lanza, et al. in 1991 [5] and by, like a surgical alternative with best visualization, decreasing the amount of necessary dissection, decreasing the likelihood of complications, with improvement of functional outcomes and a better integration into endoscopic sinus procedures, to compared with traditional headlight septoplasty technique.
Powered instrumentation during endoscopic septoplasty has been advocated in 1994 by Becker, et al. [6] and later by the main author of this paper (De Sousa, et al.) [7] in 1999. Endoscopic septoplasty, especially when it done in conjunction with powered instrumentation has dramatically improved effectiveness as compared with traditional headlight septoplasty. Powered instrumentation is a well-suited method to resect obstructive nasal septum deflections and isolated irregularities. Unlike the traditional septoplasty, endoscopic powered instrumentation allows direct visualization of the operative site.
Many authors had proved separately the useful of microdebrider burs in the treatment of complex septal deformities and isolated septal spurs by allowing a more precise in taking down septal bony defects, refining bony irregularities and conservative straighten the septum [7-9]. PES also allowing a quickly, safely, and more precise removal targeted septal tissue, so you spend less time under anesthesia and may reduce risk of damage to healthy tissue and risk of perforated septum. Likewise, the advisable microdebrider use has proved to be a more controlled and precise surgical instrument, which may help prevent accidentally damaging or removing too much tissue [7].
The microdebrider rasps provide a precise calibrated motion, avoiding the excessive back and forth motion of manual rasps. Current drills have a protective sheath that covers all but the active part of the drill, protecting the skin-soft tissue envelope. These drills also have suction at the resection site. The rasp also provides a precise motion without undesirable rip up, even at the highest speeds when microdebrider is used wisely. Obviously, the unwise and improper use of powered instrumentation could cause undesirable tissue excursion. As with all procedures involving powered instrumentation (such as otologic surgery), higher speed allows greater precision and control. Indeed, the high speed allows greater control and provides the opportunity for greater precision in rasping. Powered instrumentation is also well-suited for modification of the cartilaginous septum. Powered reciprocating rasps reduce the cartilage thickness and weaken the tensile strength of the cartilage in some deflections of anterior septum caused by the tenseness effect or contracture, of elastic memory of the septal cartilage.
Patients undergoing to PES have a significant improvement in nasal symptom severity after surgery and a significant reduction of early post-op. discomfort and morbidity. This technique also allows more rapid post-op. recovery and satisfaction and decreased post-op. medication use. Patients with higher degree of symptomatic nasal obstruction have larger improvements after surgery and are the most benefited with this procedure.
When compared with standard headlight septoplasty, the endoscopic technique provides several important advantages [10-13]. Visualization with the endoscope enables improved evaluation of septal deformities particularly helpful in diagnosis and correction of superior and posterior septal deformities (Figure 1). In addition to improving visualization permits limited in primary surgical cases the PES is highly useful especially in the revision surgery septoplasty in which persisting, obstructing septal deviation may be with densely adherent septal mucosal flaps and the typical surgical dissection planes are obliterated. In another our study [14] in 141 patients with obstructive septal deviation, we reported that, PES allows accurate, conservative repair of nasal septum deviations, with better and most successful functional results and fewer complications. This technique also offered significant perioperative advantages with high postoperative patient satisfaction, in terms of reducing the severity of nasal symptoms.
The ability to directly address a persisting deviation in these cases, involves elevating the mucosal flap directly over the offending deviation by using endoscopic techniques, greatly facilitates treatment and minimizes risk damage in adjacent mucosa. Furthermore, a more natural transition between septoplasty and EPS is possible when the 2 procedures are performed jointly with the endoscope [15]. Finally, PES provides an excellent teaching tool. In this study we review our clinical experience, the effectiveness, and long-term results in 141 consecutive patients undergoing PES.
Conclusions
Endoscopy has undoubtedly improved our ability to accurately diagnose the disease during the preoperative evaluation and has also provided an opportunity for surgeons to perform operations in a minimally invasive method. A thorough examination of the nasal cavity in patients with chronic nasal obstruction symptoms is reinforced by the conduct of office nasal endoscopy and its correlation with sinus CT scan.
PES represents is a useful and verified alternative compared to traditional headlight septoplasty with a better integration into endoscopic sinus procedures and acceptable outcomes and effectiveness. PES allows a best visibility and correlation of nasal septum anatomy and its biomechanics, especially in cases involving superior or/and posterior deviations and/or isolated spurs, but also allows a septal flap dissection with minimal mucosal trauma, especially in patients with densely adherent septal mucosal flaps, typically found in cases of revision septoplasty, alike a best accuracy resection of septal deformity. Likewise discrete but very symptomatic septal deformities such as isolated deflection, spurs, and contact points can be managed with this technique, decreasing the amount of necessary mucosal dissection, thus less the likelihood of complications and improving functional outcomes. In our experience this approach offers significant peri-op. and post-op. advantages expressed in a less post-op. discomfort, fewer peri-op. and post-op. complications and symptomatic improvement of chronic nasal obstruction in most patients.
Patients undergoing to PES have a significant improvement in nasal symptom severity after surgery and a significant reduction of post-op discomfort and decreased post-op failures.
Financial Aid
None.
Conflict of Interest
None.
References
- Killian G (1905) The submucous window resection of the nasal septum. Ann Otol Rhinol Laryngol 14: 363-393.
- Stammberger H, Posawetz W (1990) Functional endoscopic sinus surgery. Concept, indications, and results of the Messerklinger technique. Eur Arch Otorhinolaryngol 247: 63-76.
- Nayak DR, Balakrishnan R, Murthy KD (1998) An endoscopic approach to the deviated nasal septum – A preliminary study. J Laryngol Otol 112: 934-939.
- Sindwani R, Wright ED (2003) Role of endoscopic septoplasty in the treatment of atypical facial pain. J Otolaryngol 32: 77-80.
- Lanza DC, Rosin DF, Kennedy DW (1993) Endoscopic septal spur resection. Am J Rhinol 7: 213-216.
- Becker DG, Park SS, Toriumi DM (1999) Powered instrumentation for rhinoplasty and septoplasty. Otolaryngol Clin North Am 32: 683-693.
- De Sousa A, Inciarte L, Levine H (2005) Powered endoscopic nasal septal surgery. Acta Med Port 18: 249-256.
- Lopez MA, Westine JG, Toriumi DM (2005) The role of powered instrumentation in rhinoplasty and septoplasty. J Long Term Eff Med Implants 15: 283-288.
- Raynor E (2005) Powered endoscopic septoplasty for septal deviation and isolated spurs. Arch Facial Plast Surg 7: 410-412.
- Giles WC, Gross CW, Abram AC, et al. (1994) Endoscopic septoplasty. Laryngoscope 104: 1507-1509.
- Durr DG (2003) Endoscopic septoplasty: Technique and outcomes. J Otolaryngol 32: 6-9.
- Chung BJ, Batra PS, Citardi MJ, et al. (2007) Endoscopic septoplasty: Revisitation of the technique, indications, and outcomes. Am J Rhinol 21: 307-311.
- Getz AE, Hwang PH (2008) Endoscopic septoplasty. Curr Opin Otolaryngol Head Neck Surg 16: 26-31.
- De Sousa Fontes A, Sandrea Jiménez M, Chacaltana Ayerve RR (2013) Endoscopic septoplasty in primary cases using electromechanical instruments: Surgical technique, efficacy, and results. Acta Otorrinolaringol Esp 64: 317-322.
- Hwang PH, McLaughlin RB, Lanza DC, et al. (1999) Endoscopic septoplasty: Indications, technique, and results. Otolaryngol Head Neck Surg 120: 678-682.
Corresponding Author
Aderito De Sousa F, MD, Rhinoendoscopic Division and Endoscopic Sinus & Skull Base Surgery workgroup, Instituto Medico La Floresta, Av. Ppal. Urb La Floresta, piso 2, cons. 217. Caracas 1060, Venezuela, Tel: +58-212-28645223
Copyright
© 2022 Aderito DSF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.