Girdlestone Resection Arthroplasty: A Salvage Procedure for Severe Rheumatoid Arthritis
Abstract
Occurring as the most common form of inflammatory arthritis, rheumatoid arthritis is a progressive autoimmune disease that carries significant morbidity and mortality. Notably, there are prominent orthopedic manifestations that present continued challenges for the orthopaedic surgeon when choosing appropriate operative management. In regard to the hip joint, up to 25% of all patients with rheumatoid arthritis will demonstrate some pathology that may ultimately progress to a stage that produces significant morbidity and disability. The current favorable treatment for patients with advanced rheumatoid arthritis of the hip is cementless total hip arthroplasty; however, the literature is scarce with other treatment modalities, especially in patients that are poor candidates for total hip arthroplasty. In this case report, we identify a potential additional role of Girdlestone resection arthroplasty as it was performed in a non-ambulatory patient with advanced rheumatoid arthritis of the hip. The distinct presentation of our patient necessitates a discussion about when a less common surgical intervention, the Girdlestone resection arthroplasty, can be beneficial.
Keywords
Girdlestone resection arthroplasty, Rheumatoid arthritis, Osteopenia, Osteoporosis
Introduction
Rheumatoid arthritis (RA) is a chronic systemic autoimmune disease and is the most common form of inflammatory arthritis [1]. Inflammatory cells infiltrate the synovium causing subluxation, destruction, and deformity of affected joints. These processes most commonly present radiographically as periarticular erosions, cystic changes, and osteopenia [2]. Clinical manifestations of RA include joint stiffness, swelling, and pain, with continued progression of disease ultimately leading to joint instability and disability [3]. In approximately one-fourth of RA patients, the hip joint is affected [4]. Disease burden is commonly managed pharmacology; however, when progressed to severe stages of arthritis and instability, surgical intervention is usually warranted [5].
Surgical intervention for severe manifestations of RA of the hip most commonly consists of implantation of a cementless total hip arthroplasty (THA) [6]. Most current literature supports the use of cementless THA as use of cementless components has shown great outcomes when compared to cemented components [7]. Common surgical challenges faced in patients undergoing THA for RA are poor bone quality and the presence of instability [1,4,8]. Current literature highlights osseous erosions and synovial pannus formation as contributing factors to hip instability, and ultimately, the need for revision surgery for patients who had previously undergone THA for RA [8,9]. Importantly, patient selection for THA plays a role in predicting outcomes, and in minimal or non-ambulatory patients with severe RA of the hip, an implantation of a THA may incur more complications than benefits.
Performed as definitive treatment in extreme cases of pyogenic or tuberculosis arthritis involving the hip joint, and later for advanced osteoarthritis, Girdlestone described a radical excisional arthroplasty of the hip in which the proximal portion of the femur is resected [10,11]. Known today as the Girdlestone resection arthroplasty procedure, current literature shows that the most common indications for this salvage procedure are recurring periprosthetic joint infections, native septic arthritis, and repeatedly failed THA's (often due to recurrent instability) [9,12-15]. It is also described for non-ambulatory patients with or those suffering from severe dementia [16,17]. Proximal femoral resection arthroplasty has also been described for pediatric patients with cerebral palsy for developmental dysplasia of the hip [16]. Outside of these common indications, there is little available literature delineating other indications for a Girdlestone resection arthroplasty or its role in patients with advanced RA of the hip.
Given that other forms of definitive treatment for severe RA of the hip are not well known, we feel that this case report contributes to the subject knowledge through demonstrating the efficacy of using Girdlestone resection arthroplasty to treat patients with severe RA; particularly in patients that are poor candidates for THA. We demonstrate that severe forms of RA with associated instability can be successfully treated with girdlestone resection arthroplasty, and that the conventional indications for this procedure are not exhaustive.
Case Presentation
A 71-year-old non-ambulatory female presented to the senior author's clinic with a chief complaint of right hip pain. Past medical history was significant for diabetes, RA treated with low-dose prednisone for multiple decades, and hypothyroidism. The patient had been wheelchair dependent for several years due to chronic back pain, deconditioning from rheumatoid disease, and debilitating right hip pain. Orthopedic surgical history was also significant for bilateral total knee arthroplasties, unilateral total shoulder arthroplasty, and multiple hand surgeries, all of which were related to complications of her RA.
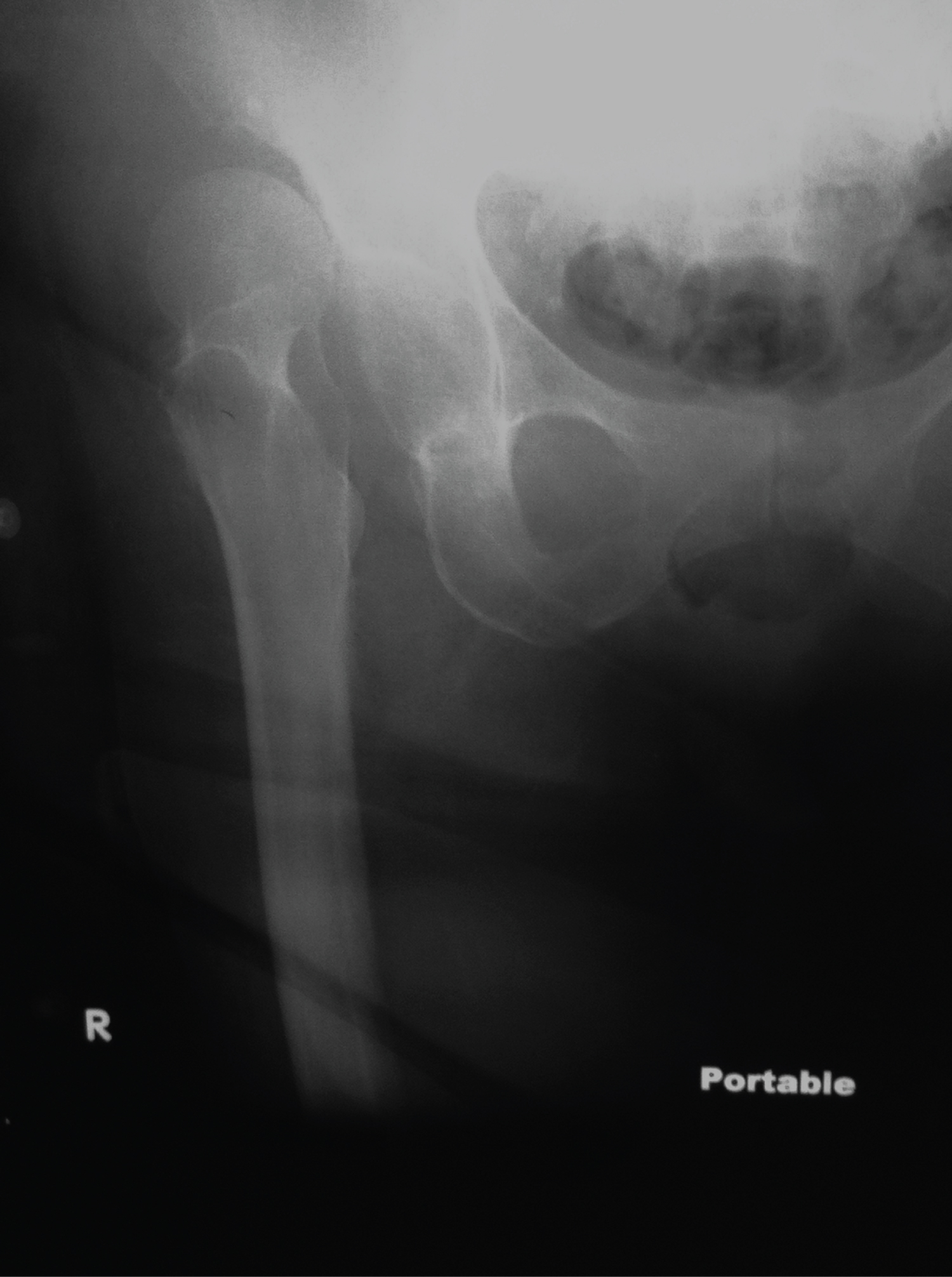
At the time of presentation, the patient reported four episodes of instability and dislocation of the right hip that required closed reduction under sedation at an outside hospital. The most recent of these being the aforementioned dislocation that occurred within the last week. The right lower extremity was held in slight flexion and internal rotation with guarding to passive motion. Motor, sensory, and vascular exams were grossly intact bilaterally. Radiographic evaluation included an anteroposterior and lateral view of the right hip as well as an anteroposterior pelvis view which showed a posterior superior right hip dislocation, significant periarticular osteopenia, and arthrosis (Figure 1).
Due to the patient's history of recurrent instability of the right hip and associated morbidity, operative treatment was elected to be undertaken. Discussion was had about constrained THA versus possible Girdlestone resection arthropaslty and the decision would be made intra-operatively by the senior attending surgeon.
Operative Procedure
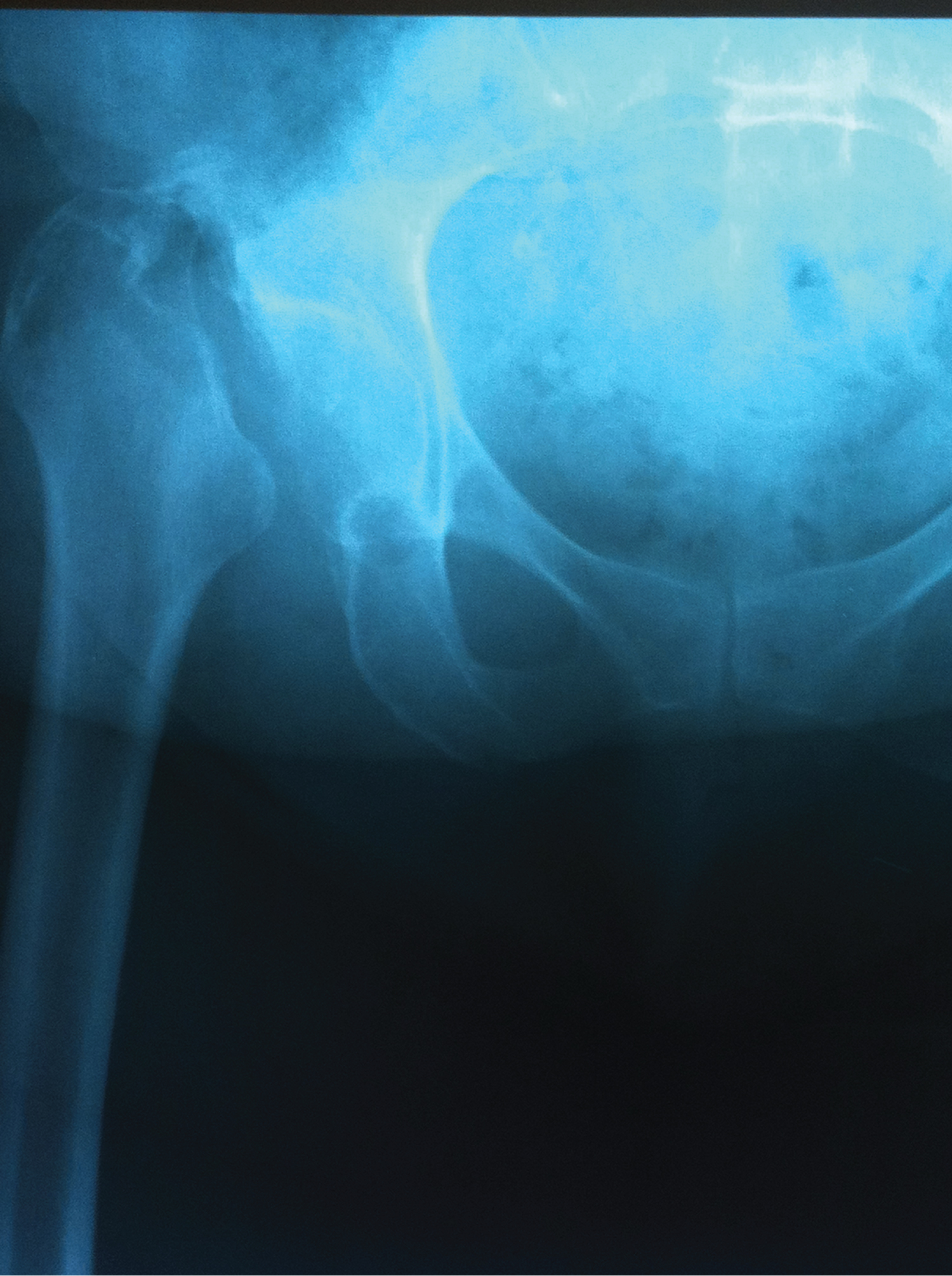
The patient was brought to the operating room and positioned supine. A standard anterolateral approach to the right hip was performed. Resection of the proximal femoral head and neck was performed in standard fashion to prepare for a THA. At the time of acetabular reaming, it was determined that the patient's bone quality was severely osteoporotic and would not be amenable to safe and stable implantation of a non-cemented acetabular cup. At this point, we did not proceed further with implantation of a cup or femoral stem and our femoral neck cuts resulted in a Girdlestone resection arthroplasty (Figure 2). The incision was closed in standard fashion and the patient did not have any immediate post-operative complications.
Postoperative Course
Postoperatively, the patient was doing well at two weeks. The pain was greatly decreased for preoperatively and the incision was well healing. At six weeks postoperatively, the patient was progressed to full weight bearing as tolerated with use of a hip-knee-ankle-foot orthosis. There were no wound complications postoperatively.
The patient reported a significant reduction in subjective instability and pain in the right hip, and was also able to obtain improved ease of transfers from bed to chair; a substantial improvement from baseline. Radiographs obtained post-operatively showed no significant proximal migration of the femur (Figure 3). Final follow-up at 13 months revealed no worsening of initial radiographic or clinical outcomes (Figure 4). At final follow up, the patient maintained her ability to transfer with the hip-knee-ankle-foot orthosis, and her pain level remained well below her preoperative level.
Discussion
Our case report successfully demonstrates that Girdlestone resection arthroplasty can be performed in a patient with debilitating hip arthritis and chronic dislocation due to RA. This study describes Gridlestone resection arthroplasty as an effective and safe treatment in a patient that is a poor candidate for THA. Additionally, our report demonstrated that Girdlestone can result in a significant decrease in hip pain as well as allow for patients to remain some mobility in those with RA. We advocate that this procedure should be considered for those patients with RA that are poor candidates for total hip arthroplasty.
RA commonly affects the hip joint and is a potential etiology of end-stage arthrosis [1,4,18]. Imagama, et al. reported that RA can lead to joint destruction, decreased activities of daily living, and gait disorder [19]. Often THA is the treatment for those with debilitating hip pain, arthrosis and destruction by RA [6,20]. However, patients with RA often have higher complication rates when compared to non-rheumatoid arthritis patients when undergoing total hip arthroplasty [21,22]. Ravi, et al. showed that patients undergoing THA for with RA had a significantly higher rate of dislocation compared to patient undergoing THA for osteoarthritis [20]. The patient in the current case was a poor candidate for THA due to her poor bone quality likely from RA, being nonambulatory and from chronic steroid use.
Girdlestone resection arthroplasty is most commonly used as a salvage procedure for recurrent periprosthetic joint infections [10]. This has been indicated conclusively by multiple studies regarding infection control and pain relief, especially when functional outcomes and patient expectations are realistic [6,9,14,23]. Girdlestone resection arthroplasty has shown to improve patient reported outcomes when suffering from debilitating hip pain. Supnet, et al. describe a patient with osteogenesis imperfecta who was able to achieve pain-free sitting, transition independently, and ambulate short distances [24]. Another study reported that results of Girdlestone arthroplasty appear to improve with time from surgery [25]. The patient in the current study was able to transfer and have significantly reduced hip pain after undergoing Girdlestone resection arthroplasty, which is consistent with other reports.
There have been other case reports and small series investigating the use of Girdlestone resection arthroplasty in an unconventional manner. Tejwani, et al. described the process by which renal osteodystrophy leads to osteopenia and an increased risk of osteomyelitis. They note that in this population, both poor bone quality and an increased risk of infection (due to chronic steroid/immunosuppressant use) increases the risk for periprosthetic joint infections, thus necessitating Girdlestone resection arthroplasty [14]. Landa, et al. identified an increased incidence of Girdlestone resection arthroplasties in osteopetrosis patients. This was attributed to the fact that the higher bone density and decreased intramedullary canal size of this patient population makes traditional arthroplasty exceedingly difficult [26]. Flynn, et al. reviewed the management of hip disorders in patients with cerebral palsy and noted that salvage procedures, including Girdlestone resection arthroplasty, may be needed [27]. They emphasize that a painfully dislocated hip with advanced degenerative changes often benefits from one of several different methods of resection arthroplasty [23,27].
There does not appear to be many salvage options for those suffering from debilitating hip pain from RA in the literature. In current case, along with the aforementioned reports, we were able to achieve realistic outcomes of improved pain management and ease of transfers in this non-ambulatory patient. In patient's demonstrating similar limitations in mobility and suffering from debilitating pain from advanced RA of the hip joint, that are not adequate candidates for THA, we advocate for Girdlestone resection arthroplasty as a viable and appropriate treatment option to improve a patient's quality of life.
Conclusion
The common treatment for hip instability and arthrosis associated with RA is a cementless THA; however, in certain circumstances, more unconventional modes of treatment can be more effective. It is important to remember that with appropriate patient selection as well as discussion of realistic expectations regarding outcomes with the patient and family, a Girdlestone resection arthroplasty can improve one's quality of life. This 71-year-old non-ambulatory female with severe RA and hip instability highlights the type of patient for which alternative treatments may be warranted. In this case and others like it, performing a Girdlestone resection arthroplasty can produce an equivalent, if not improved, outcome when compared to cementless THA.
Declarations of Interest
None.
References
- Littlejohn EA, Monrad SU (2018) Early diagnosis and treatment of rheumatoid arthritis. Prim Care 45: 237-255.
- Grassi W, De Angelis R, Lamanna G, et al. (1998) The clinical features of rheumatoid arthritis. Eur J Radiol 27: S18-S24.
- Kohan KJ, Thomas MA (2012) Acuteatraumatic hip dislocation in an adult with rheumatoid arthritis. Am J Phys Med Rehabil 91: 346-348.
- Girdlestone GR (1928) Arthrodesis and other operations for tuberculosis of the hip. The Robert Jones Birthday Volume. London, UK: Oxford University Press, 347-374.
- Schröder J, Saris D, Besselaar PP, et al. (1998) Comparison of the results of the girdlestone pseudarthrosis with reimplantation of a total hip replacement. Int Orthop 22: 215-218.
- Sharma H, De Leeuw J, Rowley DI (2005) Girdlestone resection arthroplasty following failed surgical procedures. Int Orthop 29: 92-95.
- Girdlestone GR (1945) Pseudoarthrosis: Discussion on the treatment of unilateral osteoarthritis of the hip joint. Proc R Soc Med 38: 363.
- Castellanos J, Flores X, Llusà M, et al. (1998) The girdlestone pseudarthrosis in the treatment of infected hip replacements. Int Orthop 22: 178-181.
- Lee YH, Ko PY, Kao SL, et al. (2020) Risk of total knee and hip arthroplasty in patients with rheumatoid arthritis: A 12-Year retrospective cohort study of 65,898 patients. J Arthroplasty 35: 3517-3523.
- Young BL, Watson SL, Perez JL, et al. (2018) Trends in joint replacement surgery in patients with rheumatoid arthritis. J Rheumatol 45: 158-164.
- Taylor-Williams O, Nossent J, Inderjeeth CA (2020) Incidence and complication rates for total hip arthroplasty in rheumatoid arthritis: A systematic review and meta-analysis across four decades. Rheumatol Ther 7: 685-702.
- Bourne RB, Hunter GA, Rorabeck CH, et al. (1984) A six-year follow-up of infected total hip replacements managed by Girdlestone's arthroplasty. J Bone Joint Surg Br 66: 340-343.
- Oheim R, Gille J, Schoop R, et al. (2011) Surgical therapy of hip-joint empyema. Is the girdlestone arthroplasty still up to date? Int Orthop 36: 927-933.
- Tejwani NC, Schachter AK, Immerman I, et al. (2016) Renal osteodystrophy. J Am Acad Orthop Surg 14: 303-311.
- Soong M, Rubash HE, Macaulay W (2004) Dislocation after total hip arthroplasty. J Am Acad Orthop Surg 12: 314-321.
- Yuasa T, Maezawa K, Nozawa M, et al. (2016) Cementless total hip arthroplasty for patients with rheumatoid arthritis: A more than 10-year follow-up. Eur J Orthop Surg Traumatol 26: 599-603.
- Mäkelä KT, Eskelinen A, Pulkkinen P, et al. (2011) Cemented versus cementless total hip replacements in patients fifty-five years of age or older with rheumatoid arthritis. J Bone Joint Surg Am 93: 178-186.
- Towheed TE, Brouillard D, Yendt E, et al. (1995) Osteoporosis in rheumatoid arthritis: Findings in the metacarpal, spine, and hip and a study of the determinants of both localized and generalized osteopenia. J Rheumatol 22: 440-443.
- Imagama T, Tokushige A, Seki K, et al. (2017) Weight bearing joints destruction in rheumatoid arthritis. Curr Rheumatol Rev 13: 37-42.
- Ravi B, Escott B, Shah PS, et al. (2012) A systematic review and meta-analysis comparing complications following total joint arthroplasty for rheumatoid arthritis versus for osteoarthritis. Arthritis Rheum 64: 3839-3849.
- Glick EN, Mason RM, Wenley WG (1963) Rheumatoid arthritis affecting the hip joint. Ann Rheum Dis 22: 416-423.
- Zwartelé RE, Witjes S, Doets HC, et al. (2011) Cementless total hip arthroplasty in rheumatoid arthritis: A systematic review of the literature. Arch Orthop Trauma Surg 132: 535-546.
- Baxter MP, D'Astous JL (1986) Proximal femoral resection-interposition arthroplasty: Salvage hip surgery for the severely disabled child with cerebral palsy. J Pediatr Orthop 6: 681-685.
- Cordero-Ampuero J (2012) Girdlestone procedure: When and why. Hip Int 22: S36-S39.
- Supnet I, Abiera JE, Alcausin MML, et al. (2021) Functional outcomes of an adult with osteogenesis imperfecta after rehabilitation post bilateral Girdlestone procedure. BMJ Case Rep 14:
- Landa J, Margolis N, Di Cesare P (2007) Orthopaedic management of the patient with osteopetrosis. J Am Acad Orthop Surg 15: 654-662.
- Flynn JM, Miller F (2002) Management of hip disorders in patients with cerebral palsy. J Am Acad Orthop Surg 10: 198-209.
Corresponding Author
Daniel T DeGenova, Department of Orthopedics, OhioHealth/Doctors Hospital, 5100 West Broad Street, Columbus, OH 43228, USA
Copyright
© 2023 DeGenova DT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.