PVNS (Pigmented Villonodular Synovitis) in a Child: A Case Report
Abstract
Pigmented villonodular synovitis (PVNS) is a benign proliferative disorder of uncertain etiology that affects synovial joints, bursa, and tendon sheaths. The knee is the most commonly affected joint. The Prevalence of PVNS is approximately 9.2 cases of extra-articular and 1.8 cases of intra-articular disease per 1 million population. Males are equally affected as females. PVNS rarely occurs in children thus, it can be misdiagnosed with other rheumatic diseases.
Case presentation: A 4-years-old male child presented to the orthopedic clinic in Tishreen hospital with a history of right knee pain and swelling two years ago. He had been treated with non-steroid anti-inflammatory drugs (NSAIDs) and prednisolone in response to symptoms and signs similar to juvenile idiopathic arthritis (JIA) without improvement. Physical examination revealed moderate right knee effusion with Quadriceps femoral muscle atrophy and limited range of motion. Knee MRI showed a large articular effusion with nodular intra-articular masses attached to the synovial membrane that localized in the anteromedial region of the joint. Knee arthroscopy and histologic examination were performed and histologic examination of the synovial membrane showed findings confirming the diagnosis of PVNS. Finally, after the arthroscopic synovectomy and two months of physiotherapy, the full range of motion in the knee returned to normal with no pain or swelling, and the child was followed for a year without recurrence. This case illustrates that PVNS is a disorder that can occur at any age and it can be treated arthroscopically, with good results in children and a low rate of recurrence.
Keywords
Children, Pigmented villonodular synovitis (PVNS), Knee arthroscopy
Introduction
Pigmented villonodular synovitis (PVNS), also known as diffuse tenosynovial giant cell tumor, is a benign proliferative disorder of uncertain etiology that affects synovial lined joints, bursa, and tendon sheaths [1].
This disorder results in various degrees of villous and/or nodular changes in the affected structures [2]. The knee is the most common joint, which is affected by this disease [3]. While other joints also could be affected such as the ankle, foot, hip, and elbow [4,5]. Besides, multiple joint involvements have been reported [2]. The Prevalence of PVNS is approximately 9.2 cases of extra-articular and 1.8 cases of intra-articular disease per 1 million population [6]. Males are equally affected as females [7].
PVNS is usually a benign disorder, but it may results in significant morbidity if untreated [8]. The most common symptoms are pain, joint swelling, and loss of function, in addition, eventual joint destruction can occur [9]. The management of this disease includes surgical resection and radiation therapy [9]. Recurrence is reduced with complete resection, and it is achieved more often with localized disease [8,10]. Radiation therapy may be used as a primary treatment method or in concert with surgical excision [11].
PVNS rarely occurs in children, and it could be misdiagnosed with other diseases such as juvenile idiopathic arthritis and septic arthritis [7]. Early diagnosis and successful management improve the outcome of the disease in this population because the delay in diagnosis can result in growth retardation and probable disability, thus clinicians should keep in mind PVNS as an important differential diagnosis in children that presented with chronic arthritis.
A few papers in the literature mentioned the occurrence of PVNS in children. Here we present a case of PVNS in a child that was misdiagnosed with rheumatic disease.
Case Presentation
A 4-years-old male child presented to the orthopedic clinic in Tishreen hospital with a history of right knee pain and swelling two years ago. The pain worsened with movement and improved with rest and using analgesics, in addition, the child had obvious gait abnormality and he had been treated with non-steroid anti-inflammatory drugs (NSAIDs) for seven months and prednisolone for an unknown period in response to symptoms and signs similar to juvenile idiopathic arthritis without improvement.
His parents mentioned that he had a history of right knee trauma two years ago without any gastric, ophthalmic, or dermatologic complaints and they denied any history of swelling in other joints or fever. There was no family history of rheumatic disorders.
Physical examination revealed moderate right knee effusion with Quadriceps femoral muscle atrophy and limited range of motion (Figure 1).
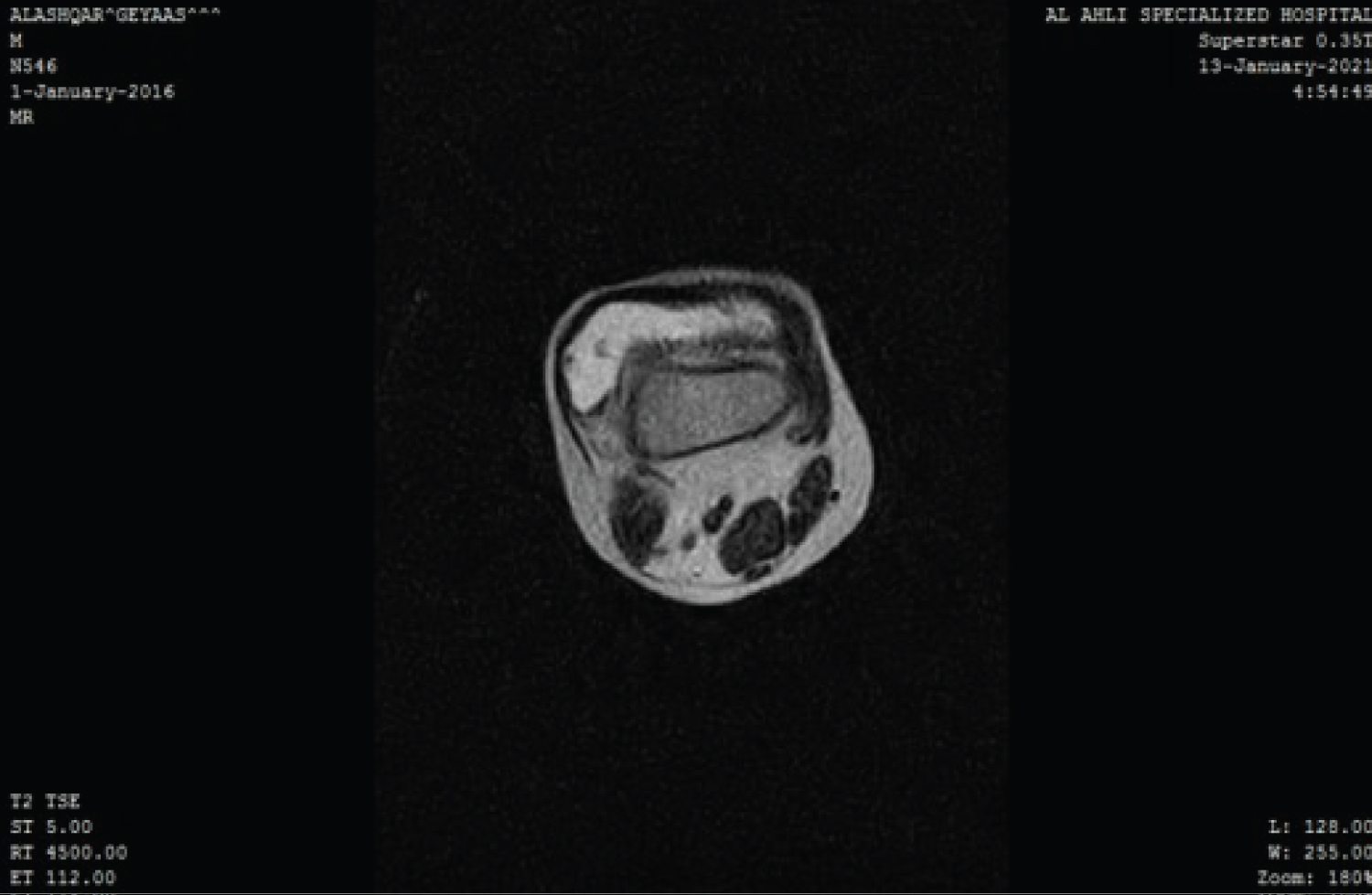
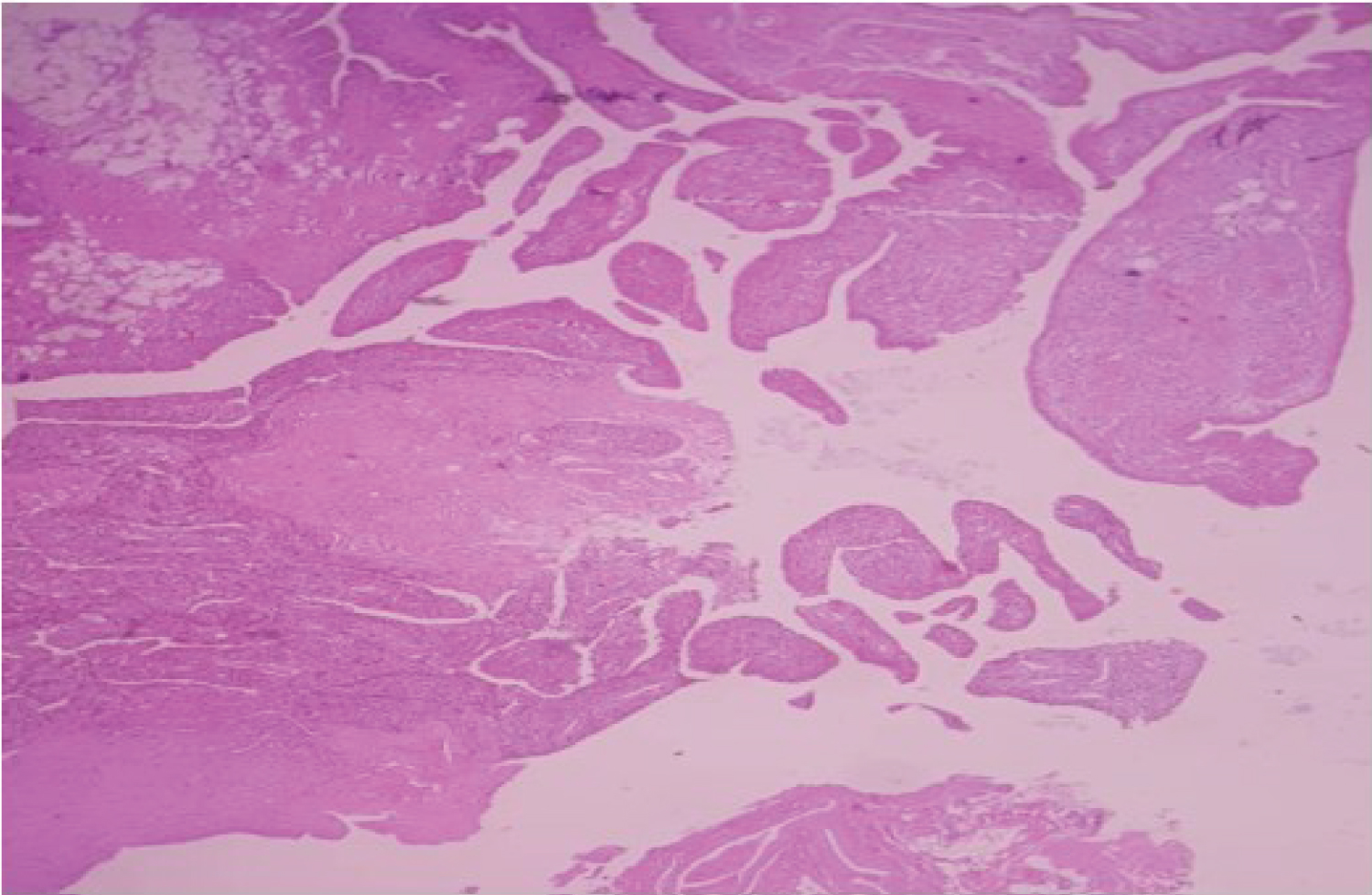
The general examination of the musculoskeletal and neurovascular systems was normal. Moreover, laboratory tests were normal, and they did not suggest that the child suffered from juvenile idiopathic arthritis or other inflammatory arthritis. While knee Ultrasonography showed high-density content effusion localized especially in the suprapatellar bursa without calcifications. Moreover, the knee MRI showed a large articular effusion with nodular intra-articular masses attached to the synovial membrane that localized in the anteromedial region of the joint (Figure 2 and Figure 3). Alongside, knee arthrocentesis was performed, and we found hemorrhagic fluid. Based on the clinical and radiographic findings, we suspected PVNS and our chosen method for confirming the diagnosis and management in our patient was surgery via Knee arthroscopy with subtotal resection of the synovial membrane and taking biopsies for histologic examination. Histologic examination of the synovial membrane shows hyperplastic synovium with papillary projections and mononuclear cells with cleaved nuclei admixed with foamy histiocytic and hemosiderin-containing macrophages, all of which supported the diagnosis of PVNS (Figure 4).
Finally, after the arthroscopic synovectomy and two months of physiotherapy, the full range of motion in the knee returned to normal with no pain or swelling. After a year of follow-up, the patient was symptom-free with a full range of motion in the knee joint, and without any signs of recurrence.
Discussion
PVNS is an uncommon disorder in children [12]. There are many reported papers describing its occurrence in the pediatric population. The median age at onset was eight-years-old with the youngest age being 12 months [7]. Our patient was four-years-old.
The symptoms vary from pain to limited range of motion and marked disability in the affected joint [1]. The disease could be misdiagnosed with other conditions such as juvenile idiopathic arthritis, tuberculosis, hemophilic arthroplasty, and malignant processes [7]. Our patient had a delay in diagnosis of about two years that he was treated for JIA without any improvement in his symptoms.
The most useful method for diagnosis is MRI [13]. The early stages of the disease may show no definitive sign-on X-ray or ultrasonography that could be normal or show only soft tissue swelling [8]. On the other hand, histologic examination shows pathognomic findings that confirm the diagnosis of PVNS [14]. The histologic examination of the synovial tissue confirmed the diagnosis of PVNS in our patient.
Generally, the available options of treatment in PVNS are surgery and radiotherapy. The standard method of treatment in case of joint involvement in our patient is synovectomy via open or arthroscopic surgery, as radiotherapy is controversial in this population due to the possibility of destruction of physis, and the possibility of post-radiation sarcomas [1]. Surgery aims to remove all the affected tissues to prevent joint destruction and reduce pain and local recurrence. We chose arthroscopic synovectomy for our patient to avoid infections and the complication of open surgery.
Recurrence can occur so all patients should be followed after surgery. In our patient, there was no sign of recurrence during 24 months of follow-up.
Conclusion
This case illustrates that PVNS is a disorder that can occur at any age, Thus Clinicians should consider this disease as a differential diagnosis in children when they have suggestive articular symptoms. Moreover, PVNS can be treated arthroscopically, with good results in children and a low rate of recurrence.
Acknowledgment
None.
Funding
None.
References
- Karami M, Soleimani M, Shari R (2018) Pigmented villonodular synovitis in the pediatric population: A review of the literature and a case report. Pediatr Rheumatol Online J 16: 6.
- Mukhopadhyay K, Smith M, Hughes PM (2006) Multifocal PVNS in a child--followed over 25 years. Skeletal Radiol 35: 539-542.
- Hong CM, Hing LT (2015) Acute knee pain in a child due to pigmented villonodular synovitis. J Orthop Case Rep 5: 78-80.
- Su H, Gould E, Penna J, et al. (2008) A rare manifestation of pigmented villonodular synovitis of the elbow in a child. Radiol Case Rep 3: 156.
- Soifer T, Guirguis S, Vigorito VJ, et al. (1993) Pigmented villonodular synovitis in a child. J Pediatr Surg 28: 1597-1600.
- Baroni E, Russo BD, Masquijo JJ, et al. (2010) Pigmented villonodular synovitis of the knee in skeletally immature patients. J Child Orthop 4: 123-127.
- Turkucar S, Makay B, Tatari H, et al. (2019) Pigmented villonodular synovitis: Four pediatric cases and brief review of the literature. J Postgrad Med 65: 233-236.
- Willimon SC, Busch MT, Perkins CA (2018) Pigmented villonodular synovitis of the knee: An underappreciated source of pain in children and adolescents. J Pediatr Orthop 38: e482-e485.
- Poutoglidou F, Metaxiotis D, Mpeletsiotis A (2020) Pigmented villonodular synovitis of the knee joint in a 10-year-old patient treated with an all-arthroscopic synovectomy: A case report. Cureus 12: e11929.
- Willimon SC, Schrader T, Perkins CA (2018) Arthroscopic management of pigmented villonodular synovitis of the hip in children and adolescents. Orthop J Sports Med 6: 2325967118763118.
- Kramer DE, Frassica FJ, Frassica DA, et al. (2009) Pigmented villonodular synovitis of the knee: Diagnosis and treatment. J Knee Surg 22: 243-254.
- Declercq J, Dobbelaere A, Baelde N, et al. (2020) Spontaneous swelling of the ankle in a child: A difficult diagnosis. Acta Orthop Belg 86: 342-346.
- Cheng XG, You YH, Liu W, et al. (2004) MRI features of pigmented villonodular synovitis (PVNS). Clin Rheumatol 23: 31-34.
- Chang YS, Ku MC, Hsu KC, et al. (1993) Pigmented villonodular synovitis. Zhonghua Yi Xue Za Zhi Chin Med J Free China Ed 52: 92-99.
Corresponding Author
Samaher Almousaa, Head of Rheumatology and Immunology Department, Tishreen Hospital, Barzeh Street, Damascus, 12143-17213, Syria, Tel: 00963-11-5160050, Fax: 00963-11-5160051
Copyright
© 2022 Almousaa S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.