Does Clinical or Radiologic Exam Better Predict Carcinomatous Invasion of the Jaw?
Abstract
Purpose: Clinical and radiologic exam are critical to determine the extent of invasion from oral squamous cell carcinoma. In this study, we examine their accuracy in the prediction of invasion of the maxilla or mandible, as judged using histopathologic correlation.
Methods: We enrolled patients into a prospective, phase one, clinical trial. The predictor variables were clinical and radiologic examination. The experimental variable was the use of cone beam CT to predict invasion of the jaw. Each variable was assessed for sensitivity, specificity, as well as diagnostic accuracy.
Results: Clinical exam, standard imaging and CBCT yielded a sensitivity of 100, 75 and 100%, a specificity of 80, 87.5 and 80% respectively and a diagnostic accuracy of 83.3% for all modalities.
Conclusion: Clinical exam, standard imaging and CBCT are of comparable diagnostic accuracy.
Keywords
Squamous cell carcinoma, Oral cancer, Mandibulectomy, Mandible invasion
Introduction
Determining the extent of invasion of oral squamous cell carcinoma (OSSCa) is paramount to obtain oncologic margins. When invasion is identified during the initial workup, this allows the surgeon to form a more definitive surgical plan. If absence of mandibular or maxillary invasion can be proven, it permits the sparing of parts of the mandible and maxilla, which are critical to facial form and function. In addition, occult infiltration of the jaw may be a source of locoregional regrowth and recurrence. Therefore, accurate clinical exam and imaging techniques are critical to treatment planning. Specifically, the accurate prediction of the presence or absence of malignant invasion of the jaw greatly influences the surgical treatment plan, potential morbidity and oncologic outcomes.
Several imaging studies have been conducted with the aim of predicting maxillary or mandibular invasion. For example, MRI, plain radiography, conventional computed tomography (CT), cone beam CT (CBCT) and PET/CT have been examined [1-15]. Cone beam CT remains a promising radiographic imaging modality for the oral and maxillofacial and head and neck surgeon. It delivers approximately 1/6 the amount of radiation and is about 1/10 the cost of a multi-slice, helical CT (the most commonly used imaging modality) [1].
In this study, our aim was to explore the accuracy of clinical and radiologic exam in predicting the presence or absence of jaw invasion by oral squamous cell carcinoma (OSSCa). Our hypothesis was that imaging and clinical exam will have similar accuracy to one another, and that CBCT will have a similar sensitivity and specificity to helical CT. Additionally, we hypothesized that CBCT may prove valuable in instances in which exam and standard imaging are equivocal, or dental artifact impairs the visualization of the primary site on helical CT.
Methods
Study design
To address the research purpose, the investigators designed and implemented a prospective, blinded, pilot clinical trial. This study was approved by the Institutional Review Board at Thomas Jefferson University. Adult patients (18 years or older) referred to our tertiary care medical center diagnosed with squamous cell carcinoma of the mandibular gingival, buccal mucosa, floor of the mouth, retro molar trigone, maxillary gingival, hard palate and tuberosity were prospectively recruited. All participants met consensus, biopsy-proven, guideline-established criteria for OSCCa.
The inclusion criteria included: adult patients age 18-85, histologic evidence of squamous cell carcinoma abutting the jaw, concern for invasion and no prior jaw surgery.
Exclusion criteria included: Prior mandibular or maxillary surgery, primary intraosseous carcinoma and prior history of radiation to the jaw. In order to isolate the detection rate of radiographic modalities, patients with obvious clinical findings of invasion including direct visual or extension into the mandible or maxilla were excluded. If it was equivocal, the patient was offered inclusion.
Those who met inclusion criteria and wished to participate were consented and enrolled.
Variables
The predictor variables were clinical and radiologic examination. The exploratory variable is the use of CBCT. The outcome variable was presence or absence of invasion of the jaw as defined by the histopathologic findings.
Data Collection Methods
Demographic information including age, gender, and ethnicity were collected. At enrollment, participants were assessed by the evaluating physician. The presence of Carcinomatous invasion of the mandible or maxilla was assessed using clinical, radiographic, and histopathologic modalities using a binary rating system.
For clinical exam, the presence of Carcinomatous invasion of the mandible/maxilla was assessed by the treating surgeon using oral cavity physical examination.
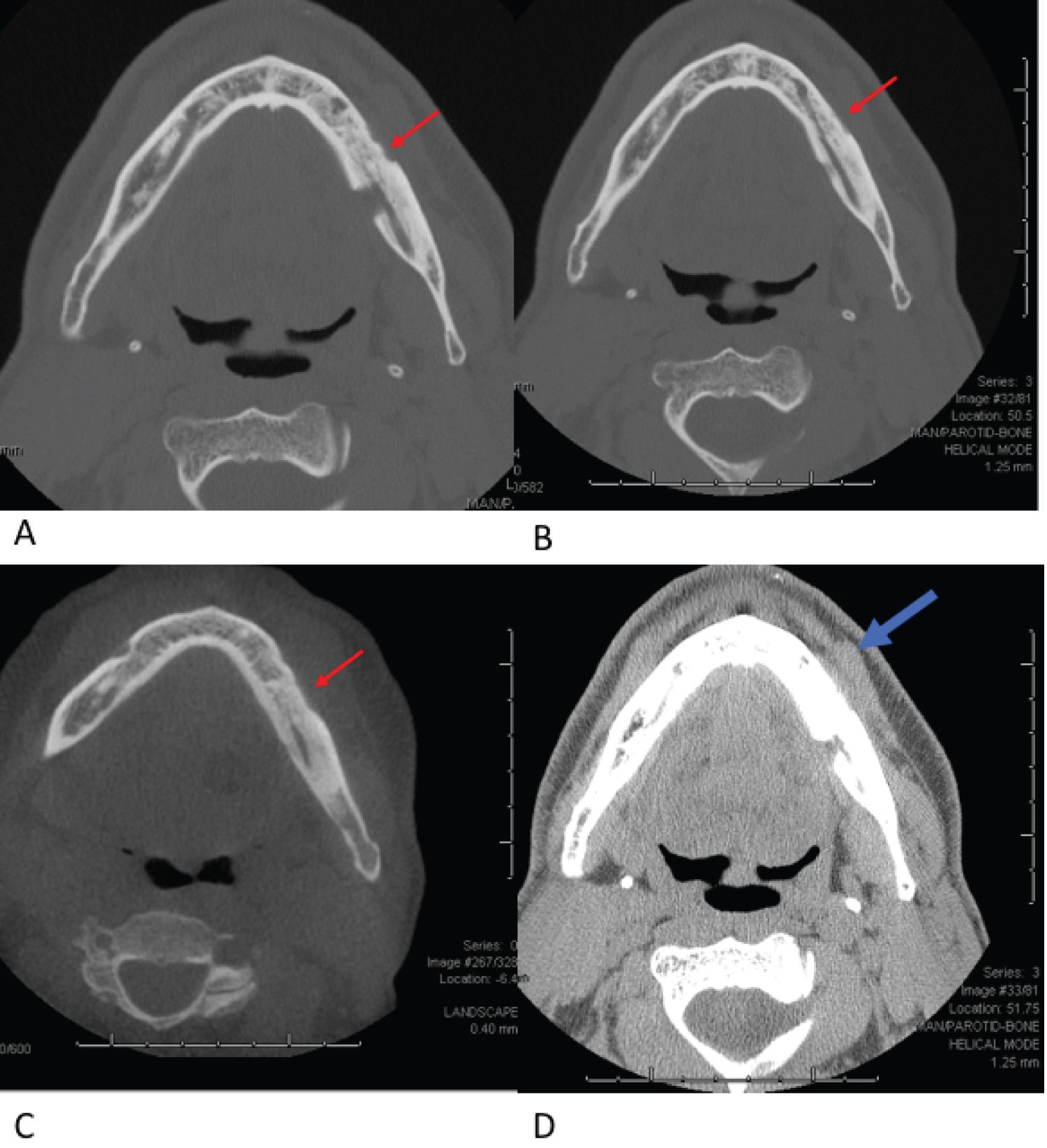
For radiologic exam, the presence of Carcinomatous invasion of the mandible or maxilla was assessed by two independent head and neck radiologists. The standard imaging was CT neck with contrast in ten of the cases and two were MRI of the face. The cone beam CT was utilized in seven instances as an adjunct to the standard imaging as ordered by the treating investigator. The head and neck radiologists were double blinded to the patient identifiers as well as to the other’s assessment. Cortical thinning, scalloping, dimpling or other irregularities were sought for tumors abutting the mandible or maxilla in order to deem there to be cortical invasion (Figure 1). When conflict occurred regarding interpretation, this was resolved by re-review and through consensus discussion.
The outcomes of each exam were recorded as either one of three options: Presence of invasion, absence of invasion, or equivocal. If the clinical or radiologic examination was equivocal, we considered it negative. This was justified following similar clinical oncologic principles in head and neck examination used for staging, such as that of extra-nodal extension (ENE) which can be found either clinically or radio logically. In order for ENE to be diagnosed, it must be unequivocally present to be clinically positive as established by the American Joint Committee on Cancer and we applied these same principles to invasion of the jaw [16]. The data was compiled into a table using Microsoft Word.
Data Analysis
Sensitivity, specificity and diagnostic accuracy was calculated for all of the variables examined. Statistical analysis was performed using R version 4.2.0. [17,18].
Results
There were twelve study participants: six male and six female for a 1:1 ratio. The median age of diagnosis and enrollment was 68 years of age. Of these patients, five were treated with marginal mandibulectomy, four with segmental mandibulectomy, two with infrastructure maxillectomy and one who had hemiglossectomy and no bony resection (Table 1).
Clinical Exam showed a sensitivity of 100% (95% CI 15.8-100), specificity of 80.0% (95% CI 44.4-97.5). It’s diagnostic accuracy was 83.3% (95% CI 51.6-97.9).
Standard Imaging showed a sensitivity of 75% (95% CI 19.4-99.4), specificity of 87.5% (95% CI 47.3-99). The diagnostic accuracy was 83.3% (95% CI 51.6-97.9).
Cone beam CT showed a sensitivity of 100% (95% CI 15.8-100), specificity of 80.0% (95% CI 44.4-97.5). The diagnostic accuracy was 83.3% (95% CI 51.6-97.9).
Discussion
In this study, we explored the accuracy of clinical and radiologic exam to predict the presence or absence of jaw invasion by oral squamous cell carcinoma (OSSCa). We hypothesized that imaging and clinical exam would have similar accuracy to one another, and that CBCT would have a similar sensitivity and specificity to standard imaging. We observed that clinical exam, standard imaging and CBCT are of comparable sensitivity and specificity and equivalent in diagnostic accuracy. Unfortunately, due to small sample size, none of our observations were statistically significant.
Other publications have examined the utility of standard imaging modalities in evaluating jaw invasion by OSSCa using CT, MRI and radionuclide bone scan. Mukherj, et al. showed that thin-section CT reconstructed with bone algorithm is an accurate technique to detect mandibular involvement by squamous cell carcinoma of the oral cavity [5]. Computed tomography was the imaging of choice from our authors as well, and we believe it represents the standard of care, particularly with the smallest slice possible. However, there are publications that advocate for the use of MRI. Bolzoni, et al. and Vidiri, et al. conclude that the high sensitivity and negative predictive value of MRI make it a useful tool in ruling out invasive disease of the jaw [6,7]. In addition, Imaizumi, et al. and Li, et al. found that MRI is more sensitive, yet less specific than CT in determining the presence and extent of mandibular invasion by squamous cell carcinoma [8,14]. Our authors posit that MRI is less sensitive in detecting subtle cortical irregularities than CT and typically does not show bony involvement until there is extension into the marrow. With the goal being early detection of invasion of the cortex, CT seems to be a superior singular study.
The advent and availability of CBCT has spawned interest in its utility for detection of jaw invasion by OSCCa. In 2010, Hendrikx, et al. examined CBCT to determine its ability to predict invasion of the mandible by carcinoma. Their assessment was that CBCT has the potential to obviate unnecessary mandibular resection and that it warranted further evaluation as such a tool, but there were no statistically significant conclusions drawn [3]. Several other publications have examined the use of CBCT as an imaging modality for evaluating mandibular invasion by oral squamous cell carcinoma. All have demonstrated sufficient accuracy of diagnosis and believe this to be a useful tool in pre-operative planning [10,12-14]. Uribe, et al. compared the sensitivity and specificity of CT, MRI, and CBCT and found all three tests to be of equal diagnostic values to detect mandibular bone invasion by oral SCC [15].
Ultimately, when clinical and radiologic exam is equivocal, additional imaging is often ordered. As there may be no one single study that is sufficient to accurately predict presence or absence of invasion, a combination of imaging modalities likely may be required. For example, Bouhir, et al. report that CT and MRI can be used as complementary tools for the preoperative assessment of mandibular bone invasion. [10] Acton, et al. found similar sensitivity, specificity, PPV, and NPV between CT and MRI, and conclude that the combination of studies improves accuracy [11]. Attempts have been made to formulate an algorithm using multimodal diagnostics, though none have become standardized. In 2008, Van Cann, et al. published a protocol of assessment of mandibular invasion by OSCCa [2]. They created an algorithm whereby either CT or MRI were employed as the first diagnostic test, followed by a bone SPECT when the initial imaging was negative. In their 67 patient cohorts, a negative bone SPECT ruled out mandibular invasion with 100% sensitivity. They reported diagnostic accuracy of 85% without false negative results. This provides excellent oncologic control of mandibular invasion, however false positives did occur with SPECT. Despite promising oncologic control, there is room for improvement in obviating unnecessary resection in the setting of a false positive result.
This study has several limitations. First, it was of small sample size and therefore not large enough to be able to draw any statistically significant conclusions. Second, the standard imaging was left to the discretion of the treating surgeon and though most studies ordered were the same (CT), there was some variation. Third, several patients in the study did not receive CBCT, which decreased the number of studies available as compared to those for standard imaging. A larger clinical trial with increased standardization of the protocol could yield statistically significant data that may aid practitioners in assessing jaw invasion in future patients.
Funding Sources
None.
Conflict of Interest
None.
Authors Contribution
Elliot Cherkas, BA: Data analysis, manuscript preparation; Rapheal Banoub MD: Data analysis, manuscript preparation; Allen Champion DDS: Data analysis, manuscript review; Madalina Tuluc, MD: Data analysis, manuscript preparation; Majid Khan MD: Data analysis, manuscript review; Neeta Rao MD: Data analysis, manuscript review; James C Gates, DMD, MD: Conceptualization, trial design, manuscript preparation, data analysis.
References
- Closmann JJ, Schmidt BL (2007) The use of cone beam computed tomography as an aid in evaluating and treatment planning for mandibular cancer. Journal of Oral and Maxillofacial Surgery 65: 766-771.
- Van Cann EM, Koole R, Oyenet WJG, et al. (2008) Assessment of mandibular invasion of squamous cell carcinoma by various modes of imaging: constructing a diagnostic algorithm. Int Oral Maxillofac Surg 37: 535-541.
- Hendrikx AWF, Maal T, Dieleman F, et al. (2010) Cone-beam CT in the assessment of mandibular invasion by oral squamous cell carcinoma: Results of the preliminary study. Int J Oral Maxillofac Surg 39: 436-439.
- Momin MA, Okochi K, Watanabe H, et al. (2009) Diagnostic accuracy of cone-beam CT in the assessment of mandibular invasion of lower gingival carcinoma: Comparison with conventional panoramic radiography. Eur J Radiol 72: 75-81.
- Mukherji SK, Isaacs DL, Creager A, et al. (2001) detection of mandibular invasion by squamous cell carcinoma of the oral cavity. AJR Am J Roentgenol 177: 237-243.
- Bolzoni A, Cappiello J, Piazza C, et al. (2004) Diagnostic accuracy of magnetic resonance imaging in the assessment of mandibular involvement in oral-oropharyngeal squamous cell carcinoma: A Prospective Study. Arch Otolaryngology Head Neck Surg 130: 837-843.
- Vidiri A, Guerrisi A, Pellini R, et al. (2010) Multi-detector row computed tomography (mdct) and magnetic resonance imaging (mri) in the evaluation of the mandibular invasion by squamous cell carcinomas (scc) of the oral cavity. Correlation with pathological data. J Exp Clin Cancer Res 29: 73.
- Imaizumi A, Yoshino N, Yamada I, et al. (2006) A potential pitfall of mr imaging for assessing mandibular invasion of squamous cell carcinoma in the oral cavity. AJNR Am J Neuroradiol 27: 114-122.
- Lewis-Jones HG, Rogers SN, Beirne JC, et al. (2000) Radionuclide bone imaging for detection of mandibular invasion by squamous cell carcinoma. The British Journal of Radiology 73: 488-493.
- Bouhir S, Mortuaire G, Dubrulle-Berthelot F, et al. (2019) Radiological assessment of mandibular invasion in squamous cell carcinoma of the oral cavity and oropharynx. European Annals of Otorhinolaryngology, Head and Neck Diseases 136: 361-366.
- Acton, Layt, Gwynne, et al. (2000) Investigative modalities of mandibular invasion by squamous cell carcinoma. The Laryngoscope 110: 2050-2055.
- Bombeccari GP, Candotto V, Giannì AB, et al. (2019) Accuracy of the Cone Beam Computed Tomography in the Detection of Bone Invasion in Patients with Oral Cancer: A Systematic Review. Eurasian J Med 51: 298-306.
- Wang Z, Zhang S, Pu Y, et al. (2020) Accuracy of cone-beam computed tomography for the evaluation of mandible invasion by oral squamous cell carcinoma. 10 March PREPRINT (Version 1) available at Research Square.
- Islam MA, Uddin MN, Ali MS, et al. (2018) Cone-beam computed tomography to assess mandibular invasion in oral squamous cell carcinoma. Update Dental College Journal 8: 18-22.
- Li C, Yang W, Men Y, et al. (2014) M agnetic resonance imaging for diagnosis of mandibular involvement from head and neck cancers: A systematic review and meta-analysis. PLOS One 9: e112267.
- Uribe S, Rojas LA, Rosas CF, et al. (2013) Accuracy of imaging methods for detection of bone tissue invasion in patients with oral squamous cell carcinoma. Dentomaxillofac Radiol 42: 20120346.
- Amin MB, Edge S, Greene F, et al. (2007) AJCC Cancer staging manual. (8th edn), Springer international publishing: American Joint Commission on Cancer.
- R Core Team (2022) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria.
Corresponding Author
James C Gates, DMD, MD, Department of Oral and Maxillofacial Surgery, Perelman Center for Advanced Medicine, 3400 Civic Center Blvd, 4th Floor, South Tower, Philadelphia, PA, 19104, USA, Tel: 215-662-3580; 215-908-4681
Copyright
© 2023 Cherkas E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.